Abstract
Purpose of Review
Given the rising prevalence of obstructive sleep apnea (OSA), we aimed to review the epidemiologic and pathophysiologic relationship of OSA, hypertension, and cardiovascular disease, and to summarize recent advances in the treatment of OSA.
Recent Findings
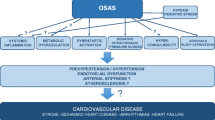
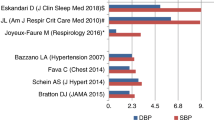
OSA is associated with an elevated risk of hypertension and cardiovascular disease. Several pathophysiologic factors contribute to the relationship between OSA and vascular risk, including neurohormonal dysregulation, endothelial dysfunction, and inflammation. While CPAP reduces blood pressure, it has not been demonstrated to reduce cardiovascular risk. The combination of CPAP and weight loss has a synergistic effect on blood pressure and several metabolic parameters. Adherence to CPAP is poor across studies, potentially contributing to the attenuation of perceived cardiovascular benefit from CPAP therapy.
Summary
A greater emphasis on adherence to CPAP and the combination of CPAP and weight loss are central to reducing cardiovascular risk among individuals with OSA.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. https://doi.org/10.5664/jcsm.6506 Clinical practice guideline on the diagnosis of obstructive sleep apnea, favoring the use of polysomnography for diagnosis.
Kryger MH. Sleep apnea. From the needles of Dionysius to continuous positive airway pressure. Arch Intern Med. 1983;143(12):2301–3.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–5. https://doi.org/10.1056/NEJM199304293281704.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14. https://doi.org/10.1093/aje/kws342.
Garvey JF, Pengo MF, Drakatos P, Kent BD. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis. 2015;7(5):920–9. https://doi.org/10.3978/j.issn.2072-1439.2015.04.52.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol. 2005;99(4):1592–9. https://doi.org/10.1152/japplphysiol.00587.2005.
Neelapu BC, Kharbanda OP, Sardana HK, Balachandran R, Sardana V, Kapoor P, et al. Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: a systematic review and meta-analysis of cephalometric studies. Sleep Med Rev. 2017;31:79–90. https://doi.org/10.1016/j.smrv.2016.01.007.
Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA. 2004;291(16):2013–6. https://doi.org/10.1001/jama.291.16.2013.
Basoglu OK, Tasbakan MS. Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath. 2018;22(1):241–9. https://doi.org/10.1007/s11325-017-1482-9.
Dong JY, Zhang YH, Qin LQ. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229(2):489–95. https://doi.org/10.1016/j.atherosclerosis.2013.04.026.
Loke YK, Brown JW, Kwok CS, Niruban A, Myint PK. Association of obstructive sleep apnea with risk of serious cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012;5(5):720–8. https://doi.org/10.1161/CIRCOUTCOMES.111.964783.
Xie C, Zhu R, Tian Y, Wang K. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis. BMJ Open. 2017;7(12):e013983. https://doi.org/10.1136/bmjopen-2016-013983.
Zhao E, Chen S, Du Y, Zhang Y. Association between sleep apnea hypopnea syndrome and the risk of atrial fibrillation: a meta-analysis of cohort study. Biomed Res Int. 2018;2018:5215868. https://doi.org/10.1155/2018/5215868.
•• Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, et al. Association of obstructive sleep apnea with hypertension: a systematic review and meta-analysis. J Glob Health. 2018;8(1):010405. https://doi.org/10.7189/jogh.08.010405 A systematic review and meta-analysis demonstrating the cross-sectional increased prevalence of hypertension in OSA as well as the prospectively increased risk of new onset hypertension in OSA.
• Strausz S, Havulinna AS, Tuomi T, Bachour A, Groop L, Makitie A, et al. Obstructive sleep apnoea and the risk for coronary heart disease and type 2 diabetes: a longitudinal population-based study in Finland. BMJ Open. 2018;8(10):e022752. https://doi.org/10.1136/bmjopen-2018-022752 A population-based cohort study of 36,963 individuals in Finland followed up to 25 years, demonstrating that OSA is an independent risk factor for the development of coronary artery disease, diabetes, and diabetic chronic kidney disease.
Nadeem R, Singh M, Nida M, Waheed I, Khan A, Ahmed S, et al. Effect of obstructive sleep apnea hypopnea syndrome on lipid profile: a meta-regression analysis. J Clin Sleep Med. 2014;10(5):475–89. https://doi.org/10.5664/jcsm.3690.
Jin S, Jiang S, Hu A. Association between obstructive sleep apnea and non-alcoholic fatty liver disease: a systematic review and meta-analysis. Sleep Breath. 2018;22(3):841–51. https://doi.org/10.1007/s11325-018-1625-7.
Nagayoshi M, Punjabi NM, Selvin E, Pankow JS, Shahar E, Iso H, et al. Obstructive sleep apnea and incident type 2 diabetes. Sleep Med. 2016;25:156–61. https://doi.org/10.1016/j.sleep.2016.05.009.
Strand LB, Carnethon M, Biggs ML, Djousse L, Kaplan RC, Siscovick DS, et al. Sleep disturbances and glucose metabolism in older adults: the cardiovascular health study. Diabetes Care. 2015;38(11):2050–8. https://doi.org/10.2337/dc15-0137.
Deacon NL, Jen R, Li Y, Malhotra A. Treatment of obstructive sleep apnea. Prospects for personalized combined modality therapy. Ann Am Thorac Soc. 2016;13(1):101–8. https://doi.org/10.1513/AnnalsATS.201508-537FR.
Knauert M, Naik S, Gillespie MB, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg. 2015;1(1):17–27. https://doi.org/10.1016/j.wjorl.2015.08.001.
Mezzanotte WS, Tangel DJ, White DP. Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism). J Clin Invest. 1992;89(5):1571–9. https://doi.org/10.1172/JCI115751.
Oliven R, Cohen G, Dotan Y, Somri M, Schwartz AR, Oliven A. Alteration in upper airway dilator muscle coactivation during sleep: comparison of patients with obstructive sleep apnea and healthy subjects. J Appl Physiol. 2018;124(2):421–9. https://doi.org/10.1152/japplphysiol.01067.2016.
Imayama I, Prasad B. Role of leptin in obstructive sleep apnea. Ann Am Thorac Soc. 2017;14(11):1607–21. https://doi.org/10.1513/AnnalsATS.201702-181FR.
Minokoshi Y, Kim YB, Peroni OD, Fryer LG, Muller C, Carling D, et al. Leptin stimulates fatty-acid oxidation by activating AMP-activated protein kinase. Nature. 2002;415(6869):339–43. https://doi.org/10.1038/415339a.
Chai SB, Sun F, Nie XL, Wang J. Leptin and coronary heart disease: a systematic review and meta-analysis. Atherosclerosis. 2014;233(1):3–10. https://doi.org/10.1016/j.atherosclerosis.2013.11.069.
Phillips BG, Kato M, Narkiewicz K, Choe I, Somers VK. Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Am J Physiol Heart Circ Physiol. 2000;279(1):H234–7. https://doi.org/10.1152/ajpheart.2000.279.1.H234.
Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, et al. Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med. 1997;157(15):1746–52.
Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ. 2000;320(7233):479–82. https://doi.org/10.1136/bmj.320.7233.479.
Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811–7. https://doi.org/10.1161/HYPERTENSIONAHA.111.179788.
Martinez-Garcia MA, Navarro-Soriano C, Torres G, Barbe F, Caballero-Eraso C, Lloberes P, et al. Beyond resistant hypertension. Hypertension. 2018;72(3):618–24. https://doi.org/10.1161/HYPERTENSIONAHA.118.11170.
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283(14):1829–36. https://doi.org/10.1001/jama.283.14.1829.
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111(5):614–21. https://doi.org/10.1161/01.CIR.0000154540.62381.CF.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000a;342(19):1378–84. https://doi.org/10.1056/NEJM200005113421901.
O’Connor GT, Caffo B, Newman AB, Quan SF, Rapoport DM, Redline S, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179(12):1159–64. https://doi.org/10.1164/rccm.200712-1809OC.
Cano-Pumarega I, Duran-Cantolla J, Aizpuru F, Miranda-Serrano E, Rubio R, Martinez-Null C, et al. Obstructive sleep apnea and systemic hypertension: longitudinal study in the general population: the Vitoria Sleep Cohort. Am J Respir Crit Care Med. 2011;184(11):1299–304. https://doi.org/10.1164/rccm.201101-0130OC.
Zhou M, Guo B, Wang Y, Yan D, Lin C, Shi Z. The association between obstructive sleep apnea and carotid intima-media thickness: a systematic review and meta-analysis. Angiology. 2017;68(7):575–83. https://doi.org/10.1177/0003319716665985.
• Korcarz CE, Peppard PE, Young TB, Chapman CB, Hla KM, Barnet JH, et al. Effects of obstructive sleep apnea and obesity on cardiac remodeling: the Wisconsin Sleep Cohort Study. Sleep. 2016;39(6):1187–95. https://doi.org/10.5665/sleep.5828 A prospective study of individuals with OSA, demonstrating that higher apnea-hypopnea index is associated with reduced left and right ventricular function.
Gottlieb DJ, Yenokyan G, Newman AB, O’Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–60. https://doi.org/10.1161/CIRCULATIONAHA.109.901801.
Javaheri S, Blackwell T, Ancoli-Israel S, Ensrud KE, Stone KL, Redline S, et al. Sleep-disordered breathing and incident heart failure in older men. Am J Respir Crit Care Med. 2016;193(5):561–8. https://doi.org/10.1164/rccm.201503-0536OC.
Foster GE, Brugniaux JV, Pialoux V, Duggan CT, Hanly PJ, Ahmed SB, et al. Cardiovascular and cerebrovascular responses to acute hypoxia following exposure to intermittent hypoxia in healthy humans. J Physiol. 2009;587(Pt 13):3287–99. https://doi.org/10.1113/jphysiol.2009.171553.
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol. 2017;69(7):841–58. https://doi.org/10.1016/j.jacc.2016.11.069.
Fletcher EC. Sympathetic over activity in the etiology of hypertension of obstructive sleep apnea. Sleep. 2003;26(1):15–9. https://doi.org/10.1093/sleep/26.1.15.
Hedner J, Ejnell H, Sellgren J, Hedner T, Wallin G. Is high and fluctuating muscle nerve sympathetic activity in the sleep apnoea syndrome of pathogenetic importance for the development of hypertension? J Hypertens Suppl. 1988;6(4):S529–S31.
Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–904. https://doi.org/10.1172/JCI118235.
Lam JC, Yan CS, Lai AY, Tam S, Fong DY, Lam B, et al. Determinants of daytime blood pressure in relation to obstructive sleep apnea in men. Lung. 2009;187(5):291–8. https://doi.org/10.1007/s00408-009-9161-7.
Phillips CL, O’Driscoll DM. Hypertension and obstructive sleep apnea. Nat Sci Sleep. 2013;5:43–52. https://doi.org/10.2147/NSS.S34841.
Jin ZN, Wei YX. Meta-analysis of effects of obstructive sleep apnea on the renin-angiotensin-aldosterone system. J Geriatr Cardiol. 2016;13(4):333–43. https://doi.org/10.11909/j.issn.1671-5411.2016.03.020.
Foster GE, Hanly PJ, Ahmed SB, Beaudin AE, Pialoux V, Poulin MJ. Intermittent hypoxia increases arterial blood pressure in humans through a renin-angiotensin system-dependent mechanism. Hypertension. 2010;56(3):369–77. https://doi.org/10.1161/HYPERTENSIONAHA.110.152108.
• Khalyfa A, Zhang C, Khalyfa AA, Foster GE, Beaudin AE, Andrade J, et al. Effect on intermittent hypoxia on plasma exosomal micro RNA signature and endothelial function in healthy adults. Sleep. 2016;39(12):2077–90. https://doi.org/10.5665/sleep.6302 An in vitro study in ten men demonstrating an association between intermittent hypoxia and serologic markers of endothelial dysfunction.
Nieto FJ, Herrington DM, Redline S, Benjamin EJ, Robbins JA. Sleep apnea and markers of vascular endothelial function in a large community sample of older adults. Am J Respir Crit Care Med. 2004;169(3):354–60. https://doi.org/10.1164/rccm.200306-756OC.
Gjorup PH, Sadauskiene L, Wessels J, Nyvad O, Strunge B, Pedersen EB. Abnormally increased endothelin-1 in plasma during the night in obstructive sleep apnea: relation to blood pressure and severity of disease. Am J Hypertens. 2007;20(1):44–52. https://doi.org/10.1016/j.amjhyper.2006.05.021.
Ip MS, Lam B, Chan LY, Zheng L, Tsang KW, Fung PC, et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med. 2000;162(6):2166–71. https://doi.org/10.1164/ajrccm.162.6.2002126.
Munoz-Hernandez R, Vallejo-Vaz AJ, Sanchez Armengol A, Moreno-Luna R, Caballero-Eraso C, Macher HC, et al. Obstructive sleep apnoea syndrome, endothelial function and markers of endothelialization. Changes after CPAP. PLoS One. 2015;10(3):e0122091. https://doi.org/10.1371/journal.pone.0122091.
Ohike Y, Kozaki K, Iijima K, Eto M, Kojima T, Ohga E, et al. Amelioration of vascular endothelial dysfunction in obstructive sleep apnea syndrome by nasal continuous positive airway pressure--possible involvement of nitric oxide and asymmetric NG, NG-dimethylarginine. Circ J. 2005;69(2):221–6.
Ip MS, Tse HF, Lam B, Tsang KW, Lam WK. Endothelial function in obstructive sleep apnea and response to treatment. Am J Respir Crit Care Med. 2004;169(3):348–53. https://doi.org/10.1164/rccm.200306-767OC.
Kheirandish-Gozal L, Gozal D. Obstructive sleep apnea and inflammation: proof of concept based on two illustrative cytokines. Int J Mol Sci. 2019;20(3). https://doi.org/10.3390/ijms20030459.
Testelmans D, Tamisier R, Barone-Rochette G, Baguet JP, Roux-Lombard P, Pepin JL, et al. Profile of circulating cytokines: impact of OSA, obesity and acute cardiovascular events. Cytokine. 2013;62(2):210–6. https://doi.org/10.1016/j.cyto.2013.02.021.
Nadeem R, Molnar J, Madbouly EM, Nida M, Aggarwal S, Sajid H, et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med. 2013;9(10):1003–12. https://doi.org/10.5664/jcsm.3070.
Taheri S, Austin D, Lin L, Nieto FJ, Young T, Mignot E. Correlates of serum C-reactive protein (CRP)--no association with sleep duration or sleep disordered breathing. Sleep. 2007;30(8):991–6. https://doi.org/10.1093/sleep/30.8.991.
Seicean S, Kirchner HL, Gottlieb DJ, Punjabi NM, Resnick H, Sanders M, et al. Sleep-disordered breathing and impaired glucose metabolism in normal-weight and overweight/obese individuals: the Sleep Heart Health Study. Diabetes Care. 2008;31(5):1001–6. https://doi.org/10.2337/dc07-2003.
Hwu DW, Lin KD, Lin KC, Lee YJ, Chang YH. The association of obstructive sleep apnea and renal outcomes-a systematic review and meta-analysis. BMC Nephrol. 2017;18(1):313. https://doi.org/10.1186/s12882-017-0731-2.
Dixon JB, Schachter LM, O’Brien PE, Jones K, Grima M, Lambert G, et al. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;308(11):1142–9. https://doi.org/10.1001/2012.jama.11580.
Sarkhosh K, Switzer NJ, El-Hadi M, Birch DW, Shi X, Karmali S. The impact of bariatric surgery on obstructive sleep apnea: a systematic review. Obes Surg. 2013;23(3):414–23. https://doi.org/10.1007/s11695-012-0862-2.
Spicuzza L, Caruso D, Di Maria G. Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis. 2015;6(5):273–85. https://doi.org/10.1177/2040622315590318.
de Vries GE, Wijkstra PJ, Houwerzijl EJ, Kerstjens HAM, Hoekema A. Cardiovascular effects of oral appliance therapy in obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:55–68. https://doi.org/10.1016/j.smrv.2017.10.004.
Phillips CL, McEwen BJ, Morel-Kopp MC, Yee BJ, Sullivan DR, Ward CM, et al. Effects of continuous positive airway pressure on coagulability in obstructive sleep apnoea: a randomised, placebo-controlled crossover study. Thorax. 2012;67(7):639–44. https://doi.org/10.1136/thoraxjnl-2011-200874.
Hu X, Fan J, Chen S, Yin Y, Zrenner B. The role of continuous positive airway pressure in blood pressure control for patients with obstructive sleep apnea and hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens (Greenwich). 2015;17(3):215–22. https://doi.org/10.1111/jch.12472.
Bazzano LA, Khan Z, Reynolds K, He J. Effect of nocturnal nasal continuous positive airway pressure on blood pressure in obstructive sleep apnea. Hypertension. 2007;50(2):417–23. https://doi.org/10.1161/HYPERTENSIONAHA.106.085175.
Iftikhar IH, Valentine CW, Bittencourt LR, Cohen DL, Fedson AC, Gislason T et al. Effects of continuous positive airway pressure on blood pressure in patients with resistant hypertension and obstructive sleep apnea: a meta-analysis. J Hypertens 2014;32(12):2341–2350; discussion 50. https://doi.org/10.1097/HJH.0000000000000372.
Pengo MF, Ratneswaran C, Berry M, Kent BD, Kohler M, Rossi GP, et al. Effect of continuous positive airway pressure on blood pressure variability in patients with obstructive sleep apnea. J Clin Hypertens (Greenwich). 2016;18(11):1180–4. https://doi.org/10.1111/jch.12845.
Dudenbostel T, Calhoun DA. Resistant hypertension, obstructive sleep apnoea and aldosterone. J Hum Hypertens. 2012;26(5):281–7. https://doi.org/10.1038/jhh.2011.47.
Pedrosa RP, Drager LF, de Paula LKG, Amaro ACS, Bortolotto LA, Lorenzi-Filho G. Effects of OSA treatment on BP in patients with resistant hypertension: a randomized trial. Chest. 2013;144(5):1487–94. https://doi.org/10.1378/chest.13-0085.
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, Martinez-Alonso M, Carmona C, Barcelo A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161–8. https://doi.org/10.1001/jama.2012.4366.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53. https://doi.org/10.1016/S0140-6736(05)71141-7.
Fu Y, Xia Y, Yi H, Xu H, Guan J, Yin S. Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breath. 2017;21(1):181–9. https://doi.org/10.1007/s11325-016-1393-1.
•• McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–31. https://doi.org/10.1056/NEJMoa1606599 A randomized controlled trial of 2717 adults with moderate-to-severe OSA and a prior history of cardiovascular disease, which demonstrated that CPAP plus usual care did reduce the risk of cardiovascular events compared with usual care alone.
Parra O, Sanchez-Armengol A, Bonnin M, Arboix A, Campos-Rodriguez F, Perez-Ronchel J, et al. Early treatment of obstructive apnoea and stroke outcome: a randomised controlled trial. Eur Respir J. 2011;37(5):1128–36. https://doi.org/10.1183/09031936.00034410.
Abuzaid AS, Al Ashry HS, Elbadawi A, Ld H, Saad M, Elgendy IY, et al. Meta-analysis of cardiovascular outcomes with continuous positive airway pressure therapy in patients with obstructive sleep apnea. Am J Cardiol. 2017;120(4):693–9. https://doi.org/10.1016/j.amjcard.2017.05.042.
Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunstrom E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med. 2016;194(5):613–20. https://doi.org/10.1164/rccm.201601-0088OC.
da Silva PF, Zhang L. Continuous positive airway pressure for adults with obstructive sleep apnea and cardiovascular disease: a meta-analysis of randomized trials. Sleep Med. 2019;54:28–34. https://doi.org/10.1016/j.sleep.2018.09.030.
•• Yu J, Zhou Z, McEvoy RD, Anderson CS, Rodgers A, Perkovic V, et al. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: a systematic review and meta-analysis. JAMA. 2017;318(2):156–66. https://doi.org/10.1001/jama.2017.7967 A systematic review and meta-analysis of randomized controlled trials comparing the effectiveness of CPAP compared with controls with regard to the development of cardiovascular events and death. The meta-analysis demonstrated that CPAP did not reduce the risk of adverse cardiovascular outcomes or death compared with controls.
Lettieri CJ, Williams SG, Collen JF, Wickwire EM. Treatment of obstructive sleep apnea: achieving adherence to positive airway pressure treatment and dealing with complications. Sleep Med Clin. 2017;12(4):551–64. https://doi.org/10.1016/j.jsmc.2017.07.005.
Loube DI, Loube AA, Erman MK. Continuous positive airway pressure treatment results in weight less in obese and overweight patients with obstructive sleep apnea. J Am Diet Assoc. 1997;97(8):896–7.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000b;284(23):3015–21. https://doi.org/10.1001/jama.284.23.3015.
Pasha S, Kumar S, Chatterjee AB, Krishnaswamy G. An obstructive sleep apnea primer: what the practicing allergist needs to know. Ann Allergy Asthma Immunol. 2017;118(3):259–68. https://doi.org/10.1016/j.anai.2016.07.033.
Drager LF, Diegues-Silva L, Diniz PM, Bortolotto LA, Pedrosa RP, Couto RB, et al. Obstructive sleep apnea, masked hypertension, and arterial stiffness in men. Am J Hypertens. 2010;23(3):249–54. https://doi.org/10.1038/ajh.2009.246.
• Hudgel DW, Patel SR, Ahasic AM, Bartlett SJ, Bessesen DH, Coaker MA, et al. The role of weight management in the treatment of adult obstructive sleep apnea. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2018;198(6):e70–87. https://doi.org/10.1164/rccm.201807-1326ST A clinical practice guidline from the American Thoracic Society supporting weight loss interventions, particularly using comprehensive lifestyle modifications, as an integral part of the treatment of individuals with OSA.
Chirinos JA, Gurubhagavatula I, Teff K, Rader DJ, Wadden TA, Townsend R, et al. CPAP, weight loss, or both for obstructive sleep apnea. N Engl J Med. 2014;370(24):2265–75. https://doi.org/10.1056/NEJMoa1306187.
Cohen JB, Cohen DL. Cardiovascular and renal effects of weight reduction in obesity and the metabolic syndrome. Curr Hypertens Rep. 2015;17(5):34. https://doi.org/10.1007/s11906-015-0544-2.
Peromaa-Haavisto P, Tuomilehto H, Kössi J, Virtanen J, Luostarinen M, Pihlajamäki J, et al. Obstructive sleep apnea: the effect of bariatric surgery after 12 months. A prospective multicenter trial. Sleep Med. 2017;35:85–90. https://doi.org/10.1016/j.sleep.2016.12.017.
Wong A, Barnes HN, Joosten SA, Landry SA, Dabscheck E, Mansfield DR, et al. The effect of surgical weight loss on obstructive sleep apnoea: a systematic review and meta-analysis. Sleep Med Rev. 2018;42:85–99.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Liann Abu Salman, Rachel Shulman, and Jordana B. Cohen declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hypertension
Rights and permissions
About this article
Cite this article
Salman, L.A., Shulman, R. & Cohen, J.B. Obstructive Sleep Apnea, Hypertension, and Cardiovascular Risk: Epidemiology, Pathophysiology, and Management. Curr Cardiol Rep 22, 6 (2020). https://doi.org/10.1007/s11886-020-1257-y
Published:
DOI: https://doi.org/10.1007/s11886-020-1257-y