Abstract
Purpose of Review
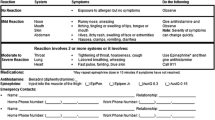
Food allergy is increasing in prevalence, and management focuses on strict avoidance of known allergens and appropriately treating reactions. Any reaction has the potential to result in anaphylaxis, which can be fatal. Children spend a significant amount of time in the childcare or school setting, and interactions between families, school personnel, and clinicians are important to ensure the health and safety of children with allergies and asthma.
Recent Findings
This review examines current food allergy guidelines and legislation, an assessment of allergen-free schools, the importance of written anaphylaxis action plans, training and education of school personnel, emerging treatment options, and the social implications of having food allergies. As the clinical use and research into food allergen immunotherapy continues to expand, an additional level of education and management is required of school personnel and caregivers.
Summary
Food allergy has both medical and social implications, which are magnified in the school setting.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):e9–17.
Prescott SL, Pawankar R, Allen KJ, Campbell DE, Sinn JKH, Fiocchi A, et al. A global survey of changing patterns of food allergy burden in children. World Allergy Organ J. 2013;6(1):21.
Sicherer SH, Sampson HA. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141(1):41–58.
Park JH, Godbold JH, Chung D, Sampson HA, Wang J. Comparison of cetirizine and diphenhydramine in the treatment of acute food-induced allergic reactions. J Allergy Clin Immunol. 2011;128(5):1127–8.
Karam M, Scherzer R, Ogbogu PU, Green TD, Greenhawt M. Food allergy prevalence, knowledge, and behavioral trends among college students - a 6-year comparison. J Allergy Clin Immunol Pract. 2017;5(2):504–6 e5.
Poirot E, et al. Deaths, hospitalizations, and emergency department visits from food-related anaphylaxis, New York City, 2000–2014: implications for fatality prevention. J Public Health Manag Pract. 2020. https://doi.org/10.1097/phh.0000000000001137.
Motosue MS, Bellolio MF, van Houten HK, Shah ND, Campbell RL. Increasing emergency department visits for anaphylaxis, 2005-2014. J Allergy Clin Immunol Pract. 2017;5(1):171–5 e3.
Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155(7):790–5.
Wang J, Bingemann T, Russell AF, Young MC, Sicherer SH. The allergist’s role in anaphylaxis and food allergy management in the school and childcare setting. J Allergy Clin Immunol Pract. 2018;6(2):427–35.
Sicherer SH, Furlong TJ, DeSimone J, Sampson HA. The US peanut and tree nut allergy registry: characteristics of reactions in schools and day care. J Pediatr. 2001;138(4):560–5.
•• Shaker MS, et al. Anaphylaxis - a 2020 practice parameter update, systematic review and grade analysis. J Allergy Clin Immunol. 2020;145(4):1082–123. This is the updated anaphylaxis practice parameter, which encompasses not just food allergy but all causes of anaphylaxis.
Anagnostou K. Anaphylaxis in children: epidemiology, risk factors and management. Curr Pediatr Rev. 2018;14(3):180–6.
Wang J, et al. Guidance on completing a written allergy and anaphylaxis emergency plan. Pediatrics. 2017;139(3):e20164005.
Lemanske RF Jr, Kakumanu S, Shanovich K, Antos N, Cloutier MM, Mazyck D, et al. Creation and implementation of SAMPRO: a school-based asthma management program. J Allergy Clin Immunol. 2016;138(3):711–23.
Vale S, Smith J, Said M, Mullins RJ, Loh R. ASCIA guidelines for prevention of anaphylaxis in schools, pre-schools and childcare: 2015 update. J Paediatr Child Health. 2015;51(10):949–54.
Cicutto L, Julien B, Li NY, Nguyen-Luu NU, Butler J, Clarke A, et al. Comparing school environments with and without legislation for the prevention and management of anaphylaxis. Allergy. 2012;67(1):131–7.
Chan ES, Dinakar C, Gonzales-Reyes E, Green TD, Gupta R, Jones D, et al. Review article: unmet needs of children with peanut allergy: aligning the risks and the evidence. Ann Allergy Asthma Immunol. 2020. In press;124:479–86.
Lawlis T, Bakonyi S, Williams LT. Food allergy in schools: the importance of government involvement. Nutr Diet. 2017;74(1):82–7.
Polloni L, Lazzarotto F, Toniolo A, Ducolin G, Muraro A. What do school personnel know, think and feel about food allergies? Clin Transl Allergy. 2013;3(1):39.
Sicherer SH, Muñoz-Furlong A, Godbold JH, Sampson HA. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol. 2010;125(6):1322–6.
Hu Y, Chen J, Li H. Comparison of food allergy prevalence among Chinese infants in Chongqing, 2009 versus 1999. Pediatr Int. 2010;52(5):820–4.
Kotz D, Simpson CR, Sheikh A. Incidence, prevalence, and trends of general practitioner-recorded diagnosis of peanut allergy in England, 2001 to 2005. J Allergy Clin Immunol. 2011;127(3):623–30 e1.
•• Bartnikas LM, et al. Impact of school peanut-free policies on epinephrine administration. J Allergy Clin Immunol. 2017;140(2):465–73. This is the first article looking at the impact of peanut-free policies in schools on epinephrine administration.
Banerjee DK, Kagan RS, Turnbull E, Joseph L, St Pierre Y, Dufresne C, et al. Peanut-free guidelines reduce school lunch peanut contents. Arch Dis Child. 2007;92(11):980–2.
Stukus DR. Peanut-free schools: what does it really mean, and are they necessary? J Allergy Clin Immunol. 2017;140(2):391–2.
Abrams EM, Greenhawt M. The role of peanut-free school policies in the protection of children with peanut allergy. J Public Health Policy. 2020;41(2):206–13.
Shaker MS, Schwartz J, Ferguson M. An update on the impact of food allergy on anxiety and quality of life. Curr Opin Pediatr. 2017;29(4):497–502.
Leo HL, Clark NM. Addressing food allergy issues within child care centers. Curr Allergy Asthma Rep. 2012;12(4):304–10.
Sicherer SH, Mahr T, the Section on Allergy and Immunology. Management of food allergy in the school setting. Pediatrics. 2010;126(6):1232–9.
Fleischer DM, Perry TT, Atkins D, Wood RA, Burks AW, Jones SM, et al. Allergic reactions to foods in preschool-aged children in a prospective observational food allergy study. Pediatrics. 2012;130(1):e25–32.
Aktas ON, Kao LM, Hoyt A, Siracusa M, Maloney R, Gupta RS. Implementation of an allergic reaction reporting tool for school health personnel: a pilot study of three Chicago schools. J Sch Nurs. 2019;35(5):316–24.
Groseclose SL, Buckeridge DL. Public health surveillance systems: recent advances in their use and evaluation. Annu Rev Public Health. 2017;38:57–79.
The treatment in school of children who have food allergies. Committee report from the Adverse Reactions to Food Committee of the American Academy of Allergy and Immunology. J Allergy Clin Immunol. 1991;87(3):749–51.
Kastner M, Harada L, Waserman S. Gaps in anaphylaxis management at the level of physicians, patients, and the community: a systematic review of the literature. Allergy. 2010;65(4):435–44.
Robinson JM, Ficca M. Managing the student with severe food allergies. J Sch Nurs. 2012;28(3):187–94.
Foster AA, et al. Anaphylaxis preparedness among preschool staff before and after an educational intervention. J Allergy (Cairo). 2015;2015:231862.
Fierstein JL, Chadha AS, Valaika SS, Gupta RS. Understanding food allergy education needs in early childhood schools. Ann Allergy Asthma Immunol. 2020;124(1):91–3.
Sirin Kose S, Asilsoy S, Tezcan D, al S, Atay O, Kangalli O, et al. Is there an optimal training interval to improve the correct use of adrenaline auto-injectors? Int Arch Allergy Immunol. 2020;181(2):136–40.
Lanser BJ, Covar R, Bird JA. Food allergy needs assessment, training curriculum, and knowledge assessment for child care. Ann Allergy Asthma Immunol. 2016;116(6):533–7 e4.
Gupta RS, Rivkina V, DeSantiago-Cardenas L, Smith B, Harvey-Gintoft B, Whyte SA. Asthma and food allergy management in Chicago public schools. Pediatrics. 2014;134(4):729–36.
Szychlinski C, Schmeissing KA, Fuleihan Z, Qamar N, Syed M, Pongracic JA, et al. Food allergy emergency preparedness in Illinois schools: rural disparity in guideline implementation. J Allergy Clin Immunol Pract. 2015;3(5):805–7 e8.
Portnoy JM, Shroba J. Managing food allergies in schools. Curr Allergy Asthma Rep. 2014;14(10):467.
Kao L, Bhangoo PS, Roy L, Bird JA. Identification of peanuts and tree nuts: are allergists smarter than their patients? Ann Allergy Asthma Immunol. 2013;111(4):282–5.
DeSantiago-Cardenas L, Rivkina V, Whyte SA, Harvey-Gintoft BC, Bunning BJ, Gupta RS. Emergency epinephrine use for food allergy reactions in Chicago public schools. Am J Prev Med. 2015;48(2):170–3.
Neupert K, Cherian S, Varshney P. Epinephrine use in Austin Independent School District after implementation of unassigned epinephrine. J Allergy Clin Immunol Pract. 2019;7(5):1650–2 e4.
Simons E, Sicherer SH, Simons FE. Timing the transfer of responsibilities for anaphylaxis recognition and use of an epinephrine auto-injector from adults to children and teenagers: pediatric allergists’ perspective. Ann Allergy Asthma Immunol. 2012;108(5):321–5.
Simons E, Sicherer SH, Weiss C, Simons FER. Caregivers' perspectives on timing the transfer of responsibilities for anaphylaxis recognition and treatment from adults to children and teenagers. J Allergy Clin Immunol Pract. 2013;1(3):309–11.
•• Miller J, et al. Quality of life in food allergic children: Results from 174 quality-of-life patient questionnaires. Ann Allergy Asthma Immunol. 2020;124(4):379–84. Quality of life in food-allergic children worsens with age, as adolescents have significantly worsened emotional, dietary, and social impacts.
Bock SA, Munoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001-2006. J Allergy Clin Immunol. 2007;119(4):1016–8.
Robinson M, Koplin JJ, Field MJ, Sasaki M, Peters RL, McWilliam V, et al. Patterns of carriage of prescribed adrenaline autoinjectors in 10- to 14-year-old food-allergic students: a population-based study. J Allergy Clin Immunol Pract. 2019;7(2):437–43.
Warren CM, Dyer AA, Otto AK, Smith BM, Kauke K, Dinakar C, et al. Food allergy-related risk-taking and management behaviors among adolescents and young adults. J Allergy Clin Immunol Pract. 2017;5(2):381–90 e13.
Herbert L, Shemesh E, Bender B. Clinical management of psychosocial concerns related to food allergy. J Allergy Clin Immunol Pract. 2016;4(2):205–13 quiz 214.
Egan M, Sicherer S. Doctor, my child is bullied: food allergy management in schools. Curr Opin Allergy Clin Immunol. 2016;16(3):291–6.
Bingemann T, Herbert LJ, Young MC, Sicherer SH, Petty CR, Phipatanakul W, et al. Deficits and opportunities in allergists’ approaches to food allergy-related bullying. J Allergy Clin Immunol Pract. 2020;8(1):343–5 e2.
Annunziato RA, Rubes M, Ambrose MA, Mullarkey C, Shemesh E, Sicherer SH. Longitudinal evaluation of food allergy-related bullying. J Allergy Clin Immunol Pract. 2014;2(5):639–41.
Feng C, Kim JH. Beyond avoidance: the psychosocial impact of food allergies. Clin Rev Allergy Immunol. 2019;57(1):74–82.
Lieberman JA, Weiss C, Furlong TJ, Sicherer M, Sicherer SH. Bullying among pediatric patients with food allergy. Ann Allergy Asthma Immunol. 2010;105(4):282–6.
Shemesh E, Annunziato RA, Ambrose MA, Ravid NL, Mullarkey C, Rubes M, et al. Child and parental reports of bullying in a consecutive sample of children with food allergy. Pediatrics. 2013;131(1):e10–7.
Feuille E, Nowak-Wegrzyn A. Allergen-specific immunotherapies for food allergy. Allergy Asthma Immunol Res. 2018;10(3):189–206.
Vickery BP, et al. AR101 oral immunotherapy for peanut allergy. N Engl J Med. 2018;379(21):1991–2001.
Eapen AA, Lavery WJ, Siddiqui JS, Lierl MB. Oral immunotherapy for multiple foods in a pediatric allergy clinic setting. Ann Allergy Asthma Immunol. 2019;123(6):573–81 e3.
Wasserman RL, Hague AR, Pence DM, Sugerman RW, Silvers SK, Rolen JG, et al. Real-world experience with peanut oral immunotherapy: lessons learned from 270 patients. J Allergy Clin Immunol Pract. 2019;7(2):418–26 e4.
Kim EH, Yang L, Ye P, Guo R, Li Q, Kulis MD, et al. Long-term sublingual immunotherapy for peanut allergy in children: clinical and immunologic evidence of desensitization. J Allergy Clin Immunol. 2019;144(5):1320–6 e1.
Fleischer DM, Greenhawt M, Sussman G, Bégin P, Nowak-Wegrzyn A, Petroni D, et al. Effect of epicutaneous immunotherapy vs placebo on reaction to Peanut protein ingestion among children with peanut allergy: the PEPITES randomized clinical trial. JAMA. 2019;321(10):946–55.
Chu DK, Wood RA, French S, Fiocchi A, Jordana M, Waserman S, et al. Oral immunotherapy for peanut allergy (PACE): a systematic review and meta-analysis of efficacy and safety. Lancet. 2019;393(10187):2222–32.
Wood RA. Food allergen immunotherapy: current status and prospects for the future. J Allergy Clin Immunol. 2016;137(4):973–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
JWH and MC declare that they have no conflict of interest relevant to this manuscript.
Dr. Lanser reports grants and personal fees from Aimmune Therapeutics, grants from DBV Technologies, grants from Regeneron, personal fees from Allergenis, personal fees from Hycor, personal fees from GSK, personal fees from Genentech, outside the submitted work, and is a member of the NIH/NIAID-sponsored CoFAR.
Human and Animal Rights and Informed Consent
This article does not contain any unpublished studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Allergy and Immunology
Rights and permissions
About this article
Cite this article
Hui, J.W., Copeland, M. & Lanser, B.J. Food Allergy Management at School in the Era of Immunotherapy. Curr Allergy Asthma Rep 20, 32 (2020). https://doi.org/10.1007/s11882-020-00933-5
Published:
DOI: https://doi.org/10.1007/s11882-020-00933-5