Opinion statement
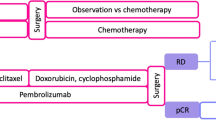
Triple-negative breast cancer (TNBC) is a particularly aggressive subtype of breast cancer. TNBC is a heterogenous subtype of breast cancer that is beginning to be refined by its molecular characteristics and clinical response to a targeted therapeutic approach. Until recently the backbone of therapy against TNBC has been cytotoxic chemotherapy. However, the breast oncology community is now seeing encouraging clinical activity from molecularly targeted approaches to TNBC. Recently, we have seen 3 newly approved targeted therapies for TNBC, including the PARP inhibitors olaparib and talazoparib for germline BRCA mutation associated breast cancer (gBRCAm-BC) and most recently the checkpoint inhibitor, atezolizumab in combination with nab-paclitaxel for programmed death-ligand 1 (PD-L1+) advanced TNBC. Improved biomarkers are needed to inform better patient selection for treatment with checkpoint inhibition. Higher response rates are seen when checkpoint inhibitors are combined with chemotherapy in the first-line setting and the use of these agents at an earlier stage of the disease does show promise. Antibody-drug conjugates are generating much excitement and may allow re-examination of prior cytotoxics that failed in development due to toxicity. Tumor sequencing is identifying potential molecular targets and ongoing studies are evaluating novel small molecule agents in this field such as AKT inhibition and many others. The treatment paradigm of chemotherapy as “one size fits all” approach for management of TNBC is changing based on molecular subtyping. Soon, the term TNBC may no longer be appropriate, as this heterogenous subtype of breast cancer is further refined by its molecular characteristics and clinical response to a targeted therapeutic approach.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–34.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Prat A, Perou CM. Deconstructing the molecular portraits of breast cancer. Mol Oncol. 2011;5(1):5–23.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011;121(7):2750–67.
Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol. 2014;25(8):1544–50.
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19(1):40–50.
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast Cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32(27):2959–66.
Loi SDD, Adams S, et al. Pooled individual patient data analysis of stomal tumor infiltrating lymphocytes in primary triple negative breast cancer treated with anthracycline-based chemotherapy. San Antonio Breast Cancer Symposium. 2015:S1–03.
Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature. 2013;500(7463):415–21.
Adams S, Schmid P, Rugo HS, Winer EP, Loirat D, Awada A, et al. Phase 2 study of pembrolizumab (pembro) monotherapy for previously treated metastatic triple-negative breast cancer (mTNBC): KEYNOTE-086 cohort a. J Clin Oncol. 2017;35(15_suppl):1008.
• Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108–21 This is a practice changing study, showing a benefit to the addition of atezolizumab in combination with nab-paclitaxel for PD-L1+ TNBC as first line therapy. This study resulted in the FDA approval of the first checkpoint inhibitor in breast cancer.
Schmid P, Park YH, Munoz-Couselo E, et al. Pembrolizumab + chemotherapy as neoadjuvant treatment for triple negative breast cancer (TNBC): preliminary results from KEYNOTE-173. J Clin Oncol. 2017 (suppl; abstr 556);35:556.
Nanda R, Liu MC, Yau C, Asare S, Hylton N, Veer LV', et al. Pembrolizumab plus standard neoadjuvant therapy for high risk breast cancer (BC): results from I-SPY 2. J Clin Oncol. 2017 (suppl; abstr 506);35:506.
Gonzalez-Angulo AM, Timms KM, Liu S, Chen H, Litton JK, Potter J, et al. Incidence and outcome of BRCA mutations in unselected patients with triple receptor-negative breast Cancer. Clin Cancer Res. 2011;17(5):1082–9.
Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, et al. Inhibition of poly (ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361(2):123–34.
Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376(9737):235–44.
Kaufman B, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, Balmaña J, et al. Olaparib monotherapy in patients with advanced Cancer and a germline BRCA1/2 mutation. J Clin Oncol. 2015;33(3):244–50.
• Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N Engl J Med. 2017;377(6):523–33 This study was the first to show a superior benefit for the PARP inhibitor olaparib in a randomized phase III study compared with chemotherapy for patients with germline BRCA mutation. It led to the FDA approval for the first PARP inhibitor in breast cancer.
• Litton JK, Rugo HS, Ettl J, et al. Talazoparib in patients with advanced breast cancer with a germline BRCA mutation. N Engl J Med. 2018;379(8):753–63 This study in a very similar design to the phase III OlympiAD study, also demonstrated superior outcome for the PARP inhibitor talazoparib over chemotherapy for patients with germline BRCA mutation and lead to the FDA approval of the second PARP inhibitor in breast cancer.
Puhalla SBJ, Pahuja S, et al. Final results of a phase 1 study of single-agent veliparib (V) in patients (pts) with either BRCA1/2-mutated cancer (BRCA+), platinum-refractory ovarian, or basal-like breast cancer (BRCA-wt). J Clin Oncol. 2014;32(Suppl):abstract 2570.
Han HS, Sook DV, Robson ME, Palácová M, et al. Efficacy and tolerability of veliparib (V; ABT-888) in combination with carboplatin (C) and paclitaxel (P) vs placebo (plc)+C/P in patients (pts) with BRCA1 or BRCA2 mutations and metastatic breast cancer: a randomized, phase 2 study. Cancer Res. 2017;77(4 Supplement):S2-05-02 SABCS16-s2-05.
Rugo HS, Olopade OI, DeMichele A, Yau C, van ‘t Veer LJ, Buxton MB, et al. Adaptive randomization of Veliparib–carboplatin treatment in breast Cancer. N Engl J Med. 2016;375(1):23–34.
Loibl S, O’Shaughnessy J, Untch M, et al. Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple-negative breast cancer (BrighTNess): a randomised, phase 3 trial. Lancet Oncol. 2018; published online Feb 28;19:497–509. https://doi.org/10.1016/S1470-2045(18)30111-6.
Litton JK, Scoggins M, Hess KR, Adrada B, Barcenas CH, Murthy RK, et al. Neoadjuvant talazoparib (TALA) for operable breast cancer patients with a BRCA mutation (BRCA+). J Clin Oncol. 2018;36(15_suppl:508.
Domchek SM P-VS, Bang Y-J, et al. An open-label, multitumor, phase II basket study of olaparib and durvalumab (MEDIOLA): Results in germline BRCA-mutated (gBRCAm) HER2-negative metastatic breast cancer (MBC). San Antonio Breast Cancer Symposium 2017; Abstract PD6–11.
Bardia A, Mayer IA, Diamond JR, Moroose RL, Isakoff SJ, Starodub AN, et al. Efficacy and safety of anti-Trop-2 antibody drug conjugate Sacituzumab Govitecan (IMMU-132) in heavily pretreated patients with metastatic triple-negative breast Cancer. J Clin Oncol. 2017;35(19):2141–8.
Modi S, Pusztai L, Forero A, et al. Phase 1 study of the antibody-drug conjugate ladiratuzumab vedotin (SGN-LIV1A) in patients with heavily pretreated triple-negative metastatic breast cancer. Presented at: 2016 San Antonio breast Cancer symposium; December 5–9, 2017; San Antonio, Texas. Abstract PD3-14.
Tamura K, Tsurutani J, Iwata H, et al. Trastuzumab deruxtecan (DS-8201a) in patients with HER2-positive breast cancer previously treated with trastuzumab emtansine: a dose-expansion, phase 1 study. Lancet Oncol. 2019;20(6):816–26.
Modi S, Tsurutani J, Takahashi S, et al. Safety and efficacy results from a phase 1 study of DS-8201a in patients with HER2 expressing breast cancers. Presented at: 2017 San Antonio breast Cancer symposium; December 5–9, 2017; San Antonio, Texas. Abstract PD3–P07.
Zardavas D, Marvelde LT, Milne RL, Fumagalli D, Fountzilas G, Kotoula V, et al. Tumor PIK3CA genotype and prognosis in early-stage breast Cancer: a pooled analysis of individual patient data. J Clin Oncol. 2017;74:8301.
Kim S-B, Dent R, Im S-A, Espié M, Blau S, Tan AR, et al. Ipatasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (LOTUS): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2017;18(10):1360–72.
Schmid P, Abraham J, Chan S, Wheatley D, Brunt M, Nemsadze G, et al. AZD5363 plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (PAKT): a randomised, double-blind, placebo-controlled, phase II trial. J Clin Oncol. 2018;36(15_suppl:1007.
Dent R, Im S-A, Espie M, Blau S, Tan AR, Isakoff SJ, et al. Overall survival (OS) update of the double-blind placebo (PBO)-controlled randomized phase 2 LOTUS trial of first-line ipatasertib (IPAT) + paclitaxel (PAC) for locally advanced/metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2018;36(15_suppl:1008.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tomas G. Lyons declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Breast Cancer
Rights and permissions
About this article
Cite this article
Lyons, T.G. Targeted Therapies for Triple-Negative Breast Cancer. Curr. Treat. Options in Oncol. 20, 82 (2019). https://doi.org/10.1007/s11864-019-0682-x
Published:
DOI: https://doi.org/10.1007/s11864-019-0682-x