Abstract
Introduction
During the COVID-19 pandemic, most medical services were shut down and resources were redistributed. Closures included pain management departments where many staff were redeployed. The aim of this study was to assess the impact of COVID-19 on chronic pain services in the Republic of Ireland.
Methods
An online survey was sent to pain consultants working in public hospitals in the Republic of Ireland between the 22nd and 28th September 2020.
Results
We received responses from 18 consultants from all 15 public hospitals in the Republic of Ireland with chronic pain services. Procedural volume during lockdown fell to 26% of pre-COVID levels. This had recovered somewhat by the time of the survey to 71%. Similarly, in-person outpatient clinic volume fell to 10% of per-COVID numbers and recovered to 50%. On average, 39% of public hospital activity was made up for by the availability of private hospitals. This varied significantly across the country. The use of telemedicine increased significantly during the pandemic. Before COVID, on average, 13% of outpatient clinic volume was composed of telephone or video consultations. This increased to 46% at the time of the survey.
Conclusion
This survey of consultant pain physicians in the Republic of Ireland has revealed how chronic pain services have been affected during the pandemic and how they have evolved.
Similar content being viewed by others
Background
During the COVID-19 pandemic, most medical services were shut down and resources were redistributed [1]. Closures included pain management departments where many staff were redeployed into theater and intensive care where their skillset was directly transferable. Chronic pain services in the Republic of Ireland could ill afford this reduction in activity as significant waiting lists exist with over 12,000 currently waiting to be seen in a chronic pain clinic nationally [2]. There are significant costs to this with a systematic review demonstrating that wait times in excess of six months are associated with a significant clinical deterioration [3].
Aims
To assess the impact of COVID-19 on chronic pain services in the Republic of Ireland, we conducted a survey of public hospital chronic pain services. We wished to determine the impact of the pandemic on procedural and clinic volumes and prescribing rates. We also wished to investigate how the service has evolved during this time period.
Methods
An online survey was sent to pain consultants working in public hospitals in the Republic of Ireland. Responses were collected between the 22nd and 28th September 2020. For assessing procedural and clinic volumes, respondents were asked to compare pre-COVID volume to volume during the lockdown and current volume. The lockdown period was defined as the time period where restrictions were placed on normal medical services due to COVID-19 that came into place in the Republic of Ireland after the 12th March 2020. Current volume was determined as the date of collection of survey responses. During the lockdown measures, a deal was reached between private hospitals and the state to allow for public patients to be treated in private hospitals. Respondents were asked to what extent the reduced public hospital activity made up for by access to private hospitals. Respondents were also asked about their views on prescribing during the pandemic and attitudes to telemedicine. Ethical committee approval was granted for the study by the local research and ethics committee.
Results
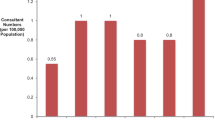
We received responses from 18 consultants from all 15 public hospitals in Ireland with chronic pain services. Procedural volume during lockdown fell to 26% of pre-COVID levels. This had recovered somewhat by the time of the survey to 71%. Similarly, in-person outpatient clinic volume fell to 10% of per-COVID numbers and recovered to 50% (Fig. 1). The most common reasons stated behind this drop in activity were concern for staff safety (78%, n = 14), concern for patients (67%, n = 12), public safety (61%, n = 11), patients did not want to come (61%, n = 11), and administrative requirements (39%, n = 7) (Fig. 2).
On average, 39% of public hospital activity was made up for by the availability of private hospitals. This varied significantly across the country with three respondents reporting a 100% transfer of activity and three respondents reporting 0%. One respondent reported their activity increased during the pandemic to 160% of their normal activity within the public system.
Regarding medication prescribing, 72% (n = 13) did not increase their prescribing rates and 50% (n = 9) reported reduced prescribing (Fig. 3). Some reported increased prescribing of neuropathic agents (22%, n = 4) and opioids (17%, n = 3). Sixty-one percent of respondents reported a concern regarding the use of corticosteroids during the pandemic (n = 11), 28% reported no concerns (n = 5) regarding medication use, and only one respondent each reported a concern regarding prescriptions of anti-inflammatories or opioids (6%) (Fig. 4).
The use of telemedicine increased significantly during the pandemic. Before COVID, on average, 13% of outpatient clinic volume was composed of telephone or video consultations (Fig. 4). This increased to 46% at the time of the survey. Seventy-two percent of respondents stated that they were either likely or very likely to continue using telemedicine after easing of restrictions (n = 13). Some concerns were reported around the use of telemedicine, most notably the inability to perform a physical exam (59%, n = 10) and concerns about liability (24%, n = 4) while 35% reported no concerns (n = 6).
Discussion
This survey examined the effects of the COVID-19 pandemic on chronic pain activity within the Republic of Ireland. We discovered that procedural volume and in-person outpatient clinic volume fell significantly during the pandemic to 26% and 10% of pre-COVID levels, respectively. This has recovered somewhat to 71% and 50%, respectively. Telemedicine use increased substantially during the pandemic to account for this shortfall in activity. Access to private hospitals during the pandemic allowed many interventional services to continue to operate with some consultants reporting transfer of 100% or greater of activity to the private hospital system. This varied significantly across the country with an average of 39%. Prescribing rates for most did not increase and the majority of respondents reported a concern around corticosteroid use.
There was a substantial drop in procedural and clinic volume during the pandemic. As staff for chronic pain services are frequently shared with other frontline services, redeployments during the pandemic removed access for many patients to a full time specialist. This is in contrast to other specialities where shadow services were largely able to remain in place throughout the pandemic. While procedural and clinic volumes have recovered somewhat, substantial waiting lists exist chronic pain services in Ireland which have been increasing year on year. According to the National Treatment Purchase Fund data, the numbers of waiting to be seen in pain therapy clinics nationally has nearly doubled between January 2015 and January 2019 from 5143 to 10,011. Since then, they have increased by a further 25% to 12,490 at August 2020. While the total numbers since the start of the year have increased broadly in line with the previous rate of growth, the numbers waiting longer than 12 months have surged since the start of the year from 4946 to 6720—an increase of more than a third. This suggests that the numbers of new referrals has dropped off since COVID-19; however, the individuals already on the waiting list are not being seen.
The arrangement which involved the state taking full capacity of private hospitals in Ireland for provision of public healthcare cost an estimated €115 million per month [4]. In this timeframe, patients who normally access private chronic pain services were unable to do so. On average, only 39% of public hospital activity was made up for by the availability of private hospitals. This varied significantly across the country. It is unknown why there was such a large variability across the country; however, this may be related to geographic concentrations of private hospitals or a bias towards facilitating those with existing private hospital privileges. Three consultants reported that this arrangement fully accounted for the usual public hospital activity with one respondent reporting an increase in their activity to 160% of normal. It could be argued that greater efficiency was possible in certain private hospitals due to the competitive pressure against a commercial bottom line that traditionally exists in this environment [5]. Other factors such as a greater medical complexity in public hospitals and a carefully selected case mix may also be relevant here. Excluding the three respondents who had no access to private hospitals, access to private hospitals accounted for 47% of usual public activity. Therefore, while this arrangement helped to alleviate some of the strain on services during this period, access was largely insufficient to account for the usual throughput.
The pandemic has allowed a service infrastructure to emerge that is radically different to the previous status quo. A substantial increase in the use of telemedicine resulted. The proportion of telemedicine clinic appointments has more than trebled with the majority of respondents indicating an intention to continue using telemedicine when services return to normal. Telemedicine consults are particularly useful for pre- and post-procedural consultations to determine whether a procedure was beneficial, for screening for COVID-19 symptoms and for patient triaging based on urgency of symptoms and the risk of deterioration, and for those who have difficulty accessing services due to geographical or time factors [6]. While we did not distinguish between modes of telemedicine, these consults can take many forms including telephone review, video review, or internet-based virtual platforms. The benefits of telephone review are that it is a minimally disruptive technology; however, over half of respondents reported concerns around the inability to perform a physical exam and a quarter indicated this led to concerns around liability. Video review can allow for a modified clinical assessment to take place and for images to be shared. Telemedicine also includes remotely delivered internet-based interventions such as pain management programs or cognitive behavioural therapy which have demonstrated improvements in disability, pain, anxiety, and depression that are comparable to in-person interventions [7]. A number of internet-based assessment and management systems have been developed in chronic pain such as the PAIN OUT and CHOIR system [8, 9]. These systems allow for a multi-disciplinary assessment to be conducted online prior to the patient being physically seen. While we did not specifically examine the use of such platforms in this survey, these are particularly attractive where long waiting lists exist such as in chronic pain, particularly regarding to its potential for scalability.
The majority of consultants surveyed did not increase their prescribing rates and half reported reduced prescribing during the pandemic. It is likely that prescribing was reduced as hospital pain clinics were not being run and patients were instead being managed in the community. It is unknown whether prescribing rates for chronic pain patients were increased in the community setting. It is speculated that due to the postponement of many surgeries and interventional treatments that prescribing rates could increase substantially during the crisis. Opioids in particular have the potential to be overprescribed in this setting [10]. Only 3 respondents (17%) however reported increased prescribing rates of opioids and one respondent (6%) reported concerns around opioid prescribing during the crisis.
In comparison, 61% (n = 11) reported a concern around the use of corticosteroids during the pandemic. The concern over steroid use arises from their known suppression of the immune system and associated increased risk of infections. Suppression of the hypothalamic–pituitary adrenal axis occurs following exogenous steroid administration and typically lasts for less than three weeks but can persist for over a month [11]. The Spine Intervention Society has stated that “there is no clear evidence of a causative effect between spinal injections and periprocedural infections and complications in immunosuppressed patients”; however, at least a theoretical risk of an increased infection risk exists [12]. Multiple randomized controlled trials have examined the doses of corticosteroids used in epidural injections and concluded that the doses used in clinical practice are excessive. The World Institute of Pain states that there is no evidence for doses greater than 10 mg dexamethasone, 20 mg triamcinolone, or 40 mg methylprednisolone for interlaminar epidural steroid injections [13]. In practice, steroids appear to be safe to use during the pandemic; however, patients should be informed during the consent process of the risk of infection and the lowest effective dose of steroid should be used [14].
Interestingly, only one respondent (6%) reported a concern around the use of NSAIDs during the pandemic. Concern arose during the pandemic over the use of NSAIDs and the increased risk of COVID-19 infection. This gained prominence following a tweet on 14th March by the French Health Minister which stated: “La prise d’anti-inflammatoires (ibuprofène, cortisone, …) pourrait être un facteur d’aggravation de l’infection. En cas de fièvre, prenex du paracetamol”—taking anti-inflammatories could worsen the infection. This purportedly came from four cases of young people who had been taking anti-inflammatories and were admitted to the intensive care unit in the south of France with a serious COVID-19 infection which remain unpublished. The WHO responded with a tweet four days later stating “Based on currently available information, WHO does not recommend against the use of ibuprofen”. A subsequent study has shown that ibuprofen may be associated with lower risk of hospitalization and ventilation and may in fact be protective in COVID-19 [15]. While at least a theoretical risk also exists with NSAIDs and COVID-19 infection, further evidence is still required to settle this question [16].
Limitations
Our survey was restricted to pain specialists; however, since many patients were unable to access specialist services during the pandemic, it would be useful to get the perspective of general practitioners on managing this patient cohort throughout the pandemic. We did not survey physiotherapists or psychologists as part of this study and therefore the impact on these services was not quantified directly in this study. We did not survey patients on their experiences of pain services throughout the pandemic; however, it would be useful to match the data presented in our study to the user experience. Data presented within this study was self-reported survey data and therefore limitations inherent to such data are present including recall bias.
Conclusion
This survey of consultant pain physicians in the Republic of Ireland has revealed how chronic pain services have been affected during the pandemic and how they have evolved. While interventional procedures and in-person clinic volumes were greatly reduced, these have recovered somewhat. The availability of private hospitals made up for some of the lost volume of procedures but this varied greatly across hospitals. Services have developed during the pandemic with telemedicine outpatient consultations now comprising nearly half of all outpatient consultations.
Data availability
Data is available from the corresponding author upon reasonable request.
References
Deer TR, Sayed D, Pope JE et al (2020) Emergence from the COVID-19 pandemic and the care of chronic pain: guidance for the interventionalist. Anesth Analg 131(2):387–394
NTPF. National Outpatient Waiting List Data. 2020
Lynch ME, Campbell F, Clark AJ et al (2008) A systematic review of the effect of waiting for treatment for chronic pain. Pain. 136(1–2):97–116
IHCA. Statement by the IHCA on private hospitals agreement. 2020
Tynkkynen LK, Vrangbæk K (2018) Comparing public and private providers: a scoping review of hospital services in Europe. BMC Health Serv Res 18(1):141
Soegaard Ballester JM, Scott MF, Owei L et al (2018) Patient preference for time-saving telehealth postoperative visits after routine surgery in an urban setting. Surgery. 163(4):672–679
Eccleston C, Fisher E, Craig L et al (2014) Psychological therapies (Internet-delivered) for the management of chronic pain in adults. Cochrane Database Syst Rev 2014(2):Cd010152
Zaslansky R, Rothaug J, Chapman CR et al (2015) PAIN OUT: the making of an international acute pain registry. Eur J Pain 19(4):490–502
Sturgeon JA, Dixon EA, Darnall BD, Mackey SC (2015) Contributions of physical function and satisfaction with social roles to emotional distress in chronic pain: a Collaborative Health Outcomes Information Registry (CHOIR) study. Pain. 156(12):2627–2633
Barnett ML (2020) Opioid prescribing in the midst of crisis — myths and realities. N Engl J Med 382(12):1086–1088
Cohen SP, Bicket MC, Jamison D et al (2013) Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med 38(3):175–200
Popescu A, Patel J, Smith CC, Committee SISsPS (2019) Spinal injections in immunosuppressed patients and the risks associated with procedural care: to inject or not to inject? Pain Med 20(6):1248–1249
Van Boxem K, Rijsdijk M, Hans G et al (2019) Safe use of epidural corticosteroid injections: recommendations of the WIP Benelux Work Group. Pain Pract 19(1):61–92
Anaesthetists FoPMotRCo. FPM & BPS joint guidance on pain interventions during the COVID-19 recovery phase. 2020
Victor M Castro RAR, Sean MJ McBride, Roy H Perlis. Identifying common pharmacotherapies associated with reduced COVID-19 morbidity using electronic health records. PREPRINT. 2020
Kutti Sridharan G, Kotagiri R, Chandiramani VH et al (2020) COVID-19 and avoiding ibuprofen. How good is the evidence? Am J Ther 27(4):e400–e4e2
Funding
The authors have no sources of funding to declare for this manuscript.
Author information
Authors and Affiliations
Contributions
CFM, DH, TOC conceived of the presented idea. CFM and TOC carried out the initiative and verified the analytical methods. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Code availability (software application or custom code)
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mullins, C.F., Harmon, D. & O’Connor, T. Quantifying the impact of COVID-19 on chronic pain services in the Republic of Ireland. Ir J Med Sci 191, 7–11 (2022). https://doi.org/10.1007/s11845-021-02509-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02509-2