Abstract
Background
Epistaxis is the most prevalent ENT emergency and a significant burden on ENT services. Our objective was to study the incidence and outcomes of patients presenting with epistaxis at a major teaching hospital.
Methods
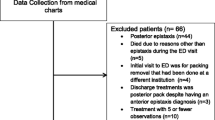
A retrospective descriptive study of 721 patients, who presented with epistaxis over a 1-year period, was carried out. Data collected was analysed using SPSS software version 20.
Results
Of the 721 patients, initial treatment consisted of nasal cautery (298), nasal packing (200), or no treatment (223). Fifty-nine patients were admitted. The mean age of admitted patients was 66.8 years and the male to female ratio was 2:1. 69.5% had hypertension and 78% used an antiplatelet/anticoagulation medication. The majority of admitted and return patients were out of hours referrals from ED and the mean admission duration was five nights. Surgical treatment for intractable epistaxis included arterial ligation or endovascular embolisation. Successful treatment was defined as no recurrent epistaxis following pack removal or no readmission with epistaxis within 24 h of hospital discharge. Six hundred forty-four patients had successful treatment.
Conclusion
More return and admitted patients presented at out-of-hours times with less clinical staff on site. Most non-admitted patients received no treatment. These factors possibly lead to increased stress on the ENT casualty service. Cautery and nasal packing are the most common treatment modalities in first-time and admitted patients yet result in considerable rates of representation.



Similar content being viewed by others
References
Kucik CJ, Clenney T (2005) Management of epistaxis. Am Fam Physician 71(2):305–311
Traboulsi H, Alam E, Hadi U (2015) Changing trends in the management of epistaxis. Int J Otolaryngol 2015:263987. https://doi.org/10.1155/2015/263987
Melia L, McGarry GW (2011) Epistaxis: update on management. Curr Opin Otolaryngol Head Neck Surg 19(1):30–35. https://doi.org/10.1097/MOO.0b013e328341e1e9
Pallin DJ, Chng YM, McKay MP, Emond JA, Pelletier AJ, Camargo CA Jr (2005) Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med 46(1):77–81. https://doi.org/10.1016/j.annemergmed.2004.12.014
Fox R, Nash R, Liu ZW, Singh A (2016) Epistaxis management: current understanding amongst junior doctors. J Laryngol Otol 130(3):252–255. https://doi.org/10.1017/S0022215115003400
Strachan D, England J (1998) First-aid treatment of epistaxis—confirmation of widespread ignorance. Postgrad Med J 74(868):113–114. https://doi.org/10.1136/pgmj.74.868.113
Tanner R, Harney MS (2015) The initial management of epistaxis. Ir Med J 108(4):123–124
Murphy CM, Kearney PM, Shelley EB, Fahey T, Dooley C, Kenny RA (2016) Hypertension prevalence, awareness, treatment and control in the over 50s in Ireland: evidence from The Irish Longitudinal Study on Ageing. J Public Health 38(3):450–458. https://doi.org/10.1093/pubmed/fdv057
Isezuo SA, Segun-Busari S, Ezunu E, Yakubu A, Iseh K, Legbo J, Alabi BS, Dunmade AE, Ologe FE (2008) Relationship between epistaxis and hypertension: a study of patients seen in the emergency units of two tertiary health institutions in Nigeria. Niger J Clin Pract 11(4):379–382
Lubianca Neto JF et al (1999) Is epistaxis evidence of end-organ damage in patients with hypertension? Laryngoscope 109(7 Pt 1):1111–1115. https://doi.org/10.1097/00005537-199907000-00019
Hart RG, Pearce LA (1993) In vivo antithrombotic effect of aspirin: dose versus nongastrointestinal bleeding. Stroke 24(1):138–139
Beran M, Petruson B (1986) Occurrence of epistaxis in habitual nose-bleeders and analysis of some etiological factors. ORL J Otorhinolaryngol Relat Spec 48(5):297–303. https://doi.org/10.1159/000275886
Tay HL, McMahon AD, Evans JMM, MacDonald TM (1998) Aspirin, nonsteroidal anti-inflammatory drugs, and epistaxis. A regional record linkage case control study. Ann Otol Rhinol Laryngol 107(8):671–674. https://doi.org/10.1177/000348949810700808
Gokdogan O et al (2017) The rate of epistaxis incidence in new-generation anticoagulants and perioperative approach in otorhinolaryngological practices. J Craniofac Surg 28(2):e178–e182. https://doi.org/10.1097/SCS.0000000000003135
Musgrave KM, Powell J (2016) A systematic review of anti-thrombotic therapy in epistaxis. Rhinology 54(4):292–391. https://doi.org/10.4193/Rhin16.040
Houses of the Oireachtas, Republic of Ireland (2017) Houses of the Oireachtas Committee on the Future of Healthcare: Slaintecare Report. Houses of the Oireachtas, Republic of Ireland
Funding
This study did not receive any external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of Informed Consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Carey, B., Sheahan, P. Aetiological profile and treatment outcomes of epistaxis at a major teaching hospital: a review of 721 cases. Ir J Med Sci 187, 761–766 (2018). https://doi.org/10.1007/s11845-017-1721-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1721-x