Abstract
Background and objective
Nightmares are typically underdiagnosed and undertreated, even though frequent nightmares are quite common in patients with sleep-related breathing disorders. Based on a previous study, we investigated whether patients would respond if they were specifically asked whether they would be interested in telephone counselling about nightmares and nightmare treatment.
Materials and methods
The present study included 537 patients with sleep-related breathing disorders who completed a nightmare questionnaire and—if interested—provided their contact data for a telephone counselling session.
Results
Of the total patients, 5.40% were interested in the telephone counselling. Most of these patients had never sought help for their nightmare condition before. This percentage is much lower than in a previous study, possibly due to the higher time expenditure related to the new consent procedure.
Conclusion
The findings indicate that patients with nightmare problems can be reached with this approach even though they have never sought professional help before. In order to minimize the threshold, it would be desirable to have clinical in-house nightmare counselling, which would not require a detailed study information brochure and informed consent.
Zusammenfassung
Hintergrund und Fragestellung
Albträume sind häufig unterdiagnostiziert und unterbehandelt, auch wenn häufige Alpträume recht oft bei Patienten mit nächtlichen Atemregulationsstörungen zu finden sind. Aufbauend auf einer früheren Studie untersuchten die Autoren die Frage, ob Patienten Interesse an einer telefonischen Beratung zum Thema Albtraum sowie Albtraumtherapie haben, wenn sie explizit gefragt werden.
Material und Methoden
Die vorliegende Studie schloss 537 Patienten mit nächtlichen Atemregulationsstörungen ein, die einen Albtraumfragebogen ausfüllten und – falls sie Interesse hatten – ihre Kontaktdaten für die telefonische Albtraumberatung angaben.
Ergebnisse
An der telefonischen Albtraumberatung waren 5,40 % der Patienten interessiert, die meisten hatten noch nie professionelle Hilfe wegen ihrer Albträume aufgesucht. Dieser Prozentsatz ist deutlich geringer als in der Vorgängerstudie, möglicherweise bedingt durch den erhöhten zeitlichen Aufwand in Zusammenhang mit dem veränderten Prozess der Einwilligung.
Schlussfolgerung
Die Ergebnisse zeigen, dass Patienten mit Albtraumproblemen mit diesem Angebot erreicht werden können, obwohl sie vorher noch nie professionelle Hilfe in Anspruch genommen haben. Um die Hemmschwelle zu minimieren, wäre ein internes klinisches Behandlungsangebot wünschenswert, das keine formale Patienteninformation und Einwilligung benötigt.
Similar content being viewed by others
Nightmare disorder (F51.5) is characterized by extended, extremely dysphoric, and well-remembered dreams that cause clinically significant distress and/or impairment in social, occupational, or other important areas of functioning [1]. The prevalence of nightmare disorder in the general population is estimated to be about 2 to 6% [11] and about 30% in a patient group with various mental disorders, e.g., mood and anxiety disorders [27]. Even though effective treatment strategies such as like imagery rehearsal therapy (IRT) are available [2, 5, 30], nightmares are typically undertreated [12, 17]. This is of clinical importance as frequent nightmare sufferers often report severe burden [6], and nightmares have been identified as an independent predictor of suicidal ideation and suicide [13].
Two possible explanations for why nightmares are rarely treated have been investigated. First, nightmare disorders are rarely diagnosed, even in sleep centers. Krakow reported that 16.3% of sleep-disordered patients (N = 718) also have problems with nightmares; however, for this specific research project, all clinicians were instructed to ask every patient explicitly about nightmares [7]. The information about problematic nightmares would have been lost in the routine procedures typical for this sleep medicine center. In a German multicenter study with N = 4001 patients undergoing diagnostic procedures for various reasons in different sleep laboratories [20], 13.4% of patients reported nightmares at least once a week—a typical cut-off for diagnosing a nightmare disorder. However, only 1.6% of the sample actually received a nightmare disorder diagnosis. The second factor reflects that nightmare sufferers rarely seek professional help for their condition. An online survey indicated that only 29.6% of 335 nightmare sufferers had ever asked a health care provider for help [28]. Similar or even lower figures were reported for persons with frequent nightmares (nightmares once a week or more often), i.e., 15.19% [18], 22.79% [22], and 33.00% [21], or students with relevant nightmare disorder symptoms (11.11%; [12]). Nightmare frequency and nightmare distress were correlated with seeking professional help [12, 18, 21], but no effects of gender, age, and education on this variable were reported [18, 21, 22]. Even if professional help was sought, only a minority rated the help as beneficial (31.76% [22] and 19% [28]). Overall, nightmare sufferers seldom asked for professional help and even if they did, their efforts were not rewarded, clearly indicating that the majority of this patient group is not treated adequately. Unfortunately, the surveys did not elicit the particulars of the treatment options provided by the health care providers. Thus, the question of whether something can be done about the problem of the very low treatment rates in nightmare sufferers is still unanswered. Schredl et al. [21] implemented the following approach in two sleep laboratories: patients received a questionnaire including questions about nightmare frequency, nightmare distress, and nightmare content, and were asked if they were interested in telephone counselling including information about nightmare etiology and a simple intervention for coping with nightmares (based on the principles of IRT [8]). Overall, about 20% of all patients who participated in the study were interested in councelling. Looking at the subgroup of persons with frequent nightmares (once a week or more often) who had never sought professional help (N = 134), almost 50% (N = 65) were interested in the telephone counselling. The percentage of those persons with frequent nightmares interested in the telephone counselling who had sought help previously (N = 66) was even higher, i.e., about 64% (N = 42), indicating that the previous consultation attempts were not beneficial. Unfortunately, due to lack of resources, it was not possible to carry out the telephone counselling with the 234 patients (20% of all patients) who stated their interest. Nevertheless, the study indicated that it is possible to reach out to patients with nightmare problems in a new way.
The present study used exactly the same methodology as the previous study [21] and was carried out in one of the previously participating sleep laboratories (Theresienkrankenhaus, Mannheim, Germany). The major difference was that due to the new General Data Protection Regulation laws in Europe (valid since May 28th, 2018), the patients who wanted to participate in the counseling had to read a six-page information sheet outlining the study’s aims and how data would be handled prior to giving their consent (within the previous study patients gave general consent [two pages] regarding processing of their clinical data). It was expected that a considerable number of persons who had never sought professional help before would be interested in this counseling offer that included information about nightmare etiology and a brief intervention. Due to the higher time expenditure regarding the consenting process, it was expected that the percentage of patients interested in counseling would be lower in 2019.
Methods
Participants
Overall, 537 patients (348 men, 189 women) underwent polysomnographic diagnostic procedures in the sleep laboratory of the Theresienkrankenhaus, Mannheim, from February 2019 to August 2019. Mean age of the total group was 60.66 ± 12.49 years (range 20 to 90 years). Almost all patients (N = 531) received a diagnosis of a sleep-related breathing disorder, three patients did not receive any diagnosis; restless legs syndrome, periodic limb movement disorder, and primary insomnia were each diagnosed once. Most patients (N = 481) had additional somatic diagnoses. For the purpose of this analysis, these diagnoses were grouped into more or less broad categories as follows: diabetes (21.23%); hypertension (17.88%); thyroid diseases (14.15%); heart diseases including coronary heart disease, atrial fibrillation, cardiomyopathy, heart failure, etc. (61.45%); asthma (8.75%); lung diseases such as chronic obstructive pulmonary disease (11.55%); hypercholesterolemia (21.42%); and mental disorders like mood and anxiety disorders (10.99%). Other diagnoses such as pain syndromes, cancer, and neurological disorders occurred in less than 5% of the patients. Most of the patients (N = 430) were in the sleep laboratory for diagnostic purposes and, if necessary, starting treatment, whereas 88 patients underwent continuous positive airway pressure (CPAP) control nights and in 12 patients the effectiveness of non-invasive ventilation therapy was evaluated.
The subsample recruited at the sleep laboratory of the Theresienkrankenhaus, Mannheim, 5 years earlier (one of the participating sleep laboratories of [21]) and which used the same questionnaire consisted of 747 patients (496 men, 251 women) with a mean age of 57.81 ± 11.88 years (range 19 to 93 years). Whereas the gender distribution did not differ between the two samples (χ2 = 0.4, p = 0.552), the current sample was significantly older than the previous one (t = 4.2, p < 0.0001).
Research instruments
To elicit nightmare frequency, an eight-point frequency scale (0 = never, 1 = less than once a year, 2 = about once a year, 3 = about 2 to 4 times a year, 4 = about once a month, 5 = 2 to 3 times a month, 6 = about once a week, and 7 = several times a week) was presented. A specific definition for nightmares was not given in this study. Retest reliability (4-week interval) of the scale was high (r = 0.75) [26]. To determine the distress associated with the nightmares a five-point scale “If you currently experience nightmares, how distressing are they?” (0 = none, 1 = low, 2 = medium, 3 = high, and 4 = very high) was presented. The retest reliability of this scale over a two-week interval was r = 0.673 [19].
Furthermore, one item measured whether participants had sought professional help regarding their nightmares in the past (yes or no), and if so, what kind of help it was (open-ended question). Lastly, patients were asked to state whether they would be interested in telephone counseling (yes or no) including further information about nightmare etiology and nightmare treatment, and a brief version of the IRT [14]. If interested, patients were asked to provide their address and telephone number.
Procedure
During the study period, all patients were asked to fill out the questionnaire prior to their first night in the sleep laboratory, which was embedded in the standard diagnostic routines. Due to this procedure, most patients completed the questionnaire, whereas an estimated 5% might not have completed the questionnaire mainly due to language problems. The patients who were interested in being contacted by the research team for telephone counselling had to read and sign a six-page informed consent according to the European General Data Protection Regulation that has been valid since May 25th, 2018, in order for personal data (addresses and phone numbers) to be used by the experimenters.
Statistical analyses were carried out with SAS 9.4 for windows (SAS Institute, Cary, NC, USA). To examine the effects of sociodemographic variables (age, gender), nightmare frequency, and nightmare distress on the “seeking help for nightmares” and “interest in telephone counselling” variables, a logistic regression procedure was used. Ordinal regressions were computed for nightmare frequency and nightmare distress.
Results
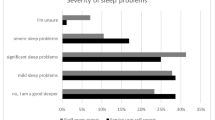
Table 1 shows the distribution of nightmare frequency scale for the 2019 sample compared to the sample elicited 5 years earlier in the same sleep laboratory [21]. About 11% of patients in the 2019 sample had frequent nightmares (at least one nightmare a week). The ordinal regression indicated that age (standardized estimate: −0.0926, χ2 = 10.5, p = 0.0012) and gender (standardized estimate: 0.1094, χ2 = 15.0, p = 0.0001) had an effect on nightmare frequency, with older persons reporting nightmares less often than younger persons and women reporting more nightmares than men. In addition, the participants of the 2019 sample reported significantly less nightmares overall than the participants of the 2014 sample (standardized estimate: −0.0850, χ2 = 9.0, p = 0.0027). The findings regarding nightmare distress are shown in Table 2. About 9% of the 2019 sample reported high or very high distress. The ordinal regression that controlled for nightmare frequency as the major factor associated with nightmare distress (standardized estimate: 0.7116, χ2 = 241.4, p < 0.0001) indicated a small but significant difference between the two samples (standardized estimate: −0.0957, χ2 = 6.0, p = 0.0141), with slightly lower values for the 2019 sample. Moreover, women tended to report more nightmare distress than men (standardized estimate: 0.1604, χ2 = 17.2, p < 0.0001), even though the gender difference regarding nightmare frequency is statistically controlled for. Age was not related to nightmare distress (standardized estimate: 0.3081, χ2 = 1.0, p = 0.3267).
Overall, 28 (5.30%) of 528 participants with valid answers for this item reported that they had ever sought help for their nightmares (see Table 3). The figure for the patients with frequent nightmares (once a week or more often) was higher, at 22.41%. The open questions were answered by 26 participants. The largest group of healthcare professionals asked for help were psychologists/psychotherapists (N = 21), general practitioners/neurologists (N = 3), and psychiatrists during inpatient treatment in a psychiatric clinic (N = 2). Logistic regression indicated that nightmare frequency was—as expected—the strongest predictor (see Table 4), whereas age and being part of the 2014 or 2019 sample were not related to the “seeking professional help” variable. Women reported having sought help more often than men, even though nightmare frequency was statistically controlled.
About 5.40% of the participants were interested in the offered telephone counselling and provided their contact data. The figures differed significantly between the two samples, with participants of the 2019 study not showing interest as often as those of the 2014 sample (Table 4). About 15.52% of the individuals with frequent nightmares (once a week or more often) expressed their interest in telephone counselling. Interest in telephone counselling was not related to age and gender but was related to nightmare frequency (Table 4). Adding nightmare distress to the variables age, gender, nightmare frequency, and the “2019 sample vs. 2014 sample” variable into the regression analysis for the “interest in telephone counselling” variable also yielded a significant effect of year (standardized estimate = −0.3813, Chi2 = 36.8, p < 0.0001, N = 740). That is, the interest in nightmare counseling was considerably lower in the 2019 study than in the 2014 study—even when statistically controlling for nightmare frequency and nightmare distress. Interestingly, 24 of the 29 participants who were interested in the counselling offer had never sought help for their nightmares previously.
In Table 5 the associations between nightmare frequency and major comorbidities (in addition to the sleep-related breathing disorder) are depicted. Only the presence of mental disorders (mood disorders, anxiety disorders) was related to an increased nightmare frequency, whereas somatic illnesses were not. A similar analysis for the participants with data regarding the severity of their sleep-related breathing disorder (N = 454) showed that neither respiratory disturbance index (RDI; standardized estimate: −0.0117, χ2 = 0.1, p = 0.8304) nor oxygen saturation nadir (standardized estimate: −0.0189, χ2 = 0.1, p = 0.7260) was related to nightmare frequency. This analysis was also controlled for age (standardized estimate: −0.0695, χ2 = 2.1, p = 0.1483) and gender (standardized estimate: 0.0242, χ2 = 0.3, p = 0.6119). The indices showed a high variability in the group of patients who underwent diagnostic procedures (RDI: 61.31 ± 25.32/h, N = 426; and oxygen saturation nadir: 76.92 ± 9.85, N = 424). The values for the CPAP control group (RDI: 16.37 ± 14.73/h, N = 30; and oxygen saturation nadir: 84.17 ± 5.40, N = 34) and the other group (RDI: 5.56 ± 7.94/h, N = 7; and oxygen saturation nadir: 82.00 ± 9.99, N = 10) were less severe.
Lastly, we compared the 19 participants who actually received telephone counselling to the 10 participants who did not (Table 6). The reasons for not taking part were inability of the experimenter to contact the participant (N = 2), participant no longer interested (N = 4), participant did not return the informed consent despite being interested (N = 1), and participant wanted the counselling at a later time because they were currently very busy (N = 3). Age and gender distribution did not differ between the two groups, but those with a higher nightmare frequency and more distress were more likely to receive the counselling (p < 0.10, marginally significant).
Discussion
The findings indicate that a considerable percentage (about 11%) of patients with sleep-related breathing disorders report frequent nightmares (once a week or more often), which is in line with previous research [7, 20, 21]. The low percentage of persons seeking professional help for their nightmare condition also replicates previous studies [12, 18, 22, 28]. As in the previous study [21], the counselling offer also interested persons who had never sought professional help before; however, the overall percentage of interested persons was considerably lower compared to the study 5 years ago [21].
The responder rate in the current study is very high because the nightmare questionnaire was part of the clinical routine, i.e., the estimated prevalence rate of frequent nightmares in patients with sleep-related breathing disorders is quite accurate. The main reason for not participating was most likely language problems (patients who were not able to read German). A limitation of the study is that no specific definition for nightmare was provided, e.g., becoming rapidly oriented and alert after awaking from a nightmare [1]. One might speculate that the reported frequencies could be overestimations, as patients might have included night terror episodes or rapid eye movement (REM) sleep behavior disorder episodes. However, as these sleep disorders are quite rare [1], a possible overestimation should be small. The decline in nightmare frequency with age has been reported in two representative German samples [15, 16] and, thus, supports the validity of the present findings. In addition, the present gender difference, with women tending to report nightmares more often than men, is in line with a meta-analysis [23], thus also supporting the validity of the findings.
The high percentage (more that 10% compared to about 5% prevalence in the general population) of persons with frequent nightmares in patients with sleep-related breathing disorders has been reported previously [20, 21], indicating that this patient group might benefit from offering nightmare therapy. Interesting, nightmare frequency in the 2019 sample was lower compared to the 2014 sample, whereby the older age could not have contributed to this difference as it was statistically controlled for. It might be that the older patients had more comorbidities compared to the previous sample, but unfortunately, this could not be tested, as comorbidities were not elicited in the previous sample.
It was also found that persons with frequent nightmares relatively rarely sought professional help for their condition, which corroborated previous findings [12, 18, 22, 28]. As most patients in this patient sample suffered from quite severe sleep apnea syndromes and a variety of somatic disorders (Table 5), one might speculate that nightmares are a minor problem with respect to general health status and, thus, unlikely to be addressed by the patients. However, as these low figures for help-seeking behavior are also reported in population-based samples [18, 22], it would be very interesting to carry out qualitative studies exploring the motivation/lack of motivation for seeking professional help, as frequent nightmares are typically very distressing [1]. One possible explanation might be the attitude that people believe there are no treatment options for nightmares [12]. Large-scale studies informing the public about the effectiveness of current nightmare treatment strategies might increase the percentage of persons seeking professional help.
As in the previous study [21], we were able to reach out to persons with nightmare problems who had never sought professional help before (even though not all of them received the telephone counselling). Overall, this indicated that this counselling offer is able reduce the gap between those persons with frequent nightmares and those receiving adequate treatment for their condition. Interestingly, the percentage of persons with an interest in telephone counseling in 2019 was much lower compared to the 2014 sample. This difference was still significant if the differences in nightmare frequency and nightmare distress were accounted for. Even though part of the difference might be explained by more severe somatic illnesses in the 2019 sample due to older age, it seems plausible that the time expenditure required to read the six pages about data protection regulations might have put some of the patients off participating in the counselling. It would be interesting to establish an in-house treatment option for persons with nightmare problems, as this is not regulated by the European General Data Protection Regulation, and study whether patients are more likely to participate counselling if the threshold is lower.
Lastly, we did not find any correlations between nightmare frequency and somatic comorbidities or sleep apnea severity, as has been reported previously [24, 25], i.e., the idea that shortage of breath might cause nightmares [4] is very unlikely. The association with comorbid mental disorders is in line with current models of nightmare etiology [14] and the heightened prevalence of nightmare disorders in patients with mental disorders [27].
To summarize, the present study replicated findings that nightmares are underdiagnosed (none of the patients had received diagnosis of a nightmare disorder) and undertreated (a minority of the patients had sought professional help for their condition), and also showed that a specific offer can reach nightmare sufferers who have never sought professional help before. As telephone counselling is quite labor intensive, one might think about offering internet-based treatment programs—the effectiveness of such programs has been shown [3, 9, 10]. Clinicians, whether they are working in sleep medicine or other areas of professional health care, should be encouraged to ask specifically about nightmare frequency and nightmare distress, and diagnose, if present, a nightmare disorder (F51.5) and refer patients to specialized treatment units. This would also imply that cognitive behavioral therapists should be trained using IRT [29] in order to provide enough treatment options. In contrast to a previous study [28] reporting that nightmare sufferers sought help mainly by consulting general practitioners, patients in this study sought help from psychotherapists.
References
American Academy of Sleep Medicine (2014) The international classification of sleep disorders. (ICSD-3). AASM, Darien
Augedal AW, Hansen KS, Kronhaug CR et al (2013) Randomized controlled trials of psychological and pharmacological treatments for nightmares: a meta-analysis. Sleep Med Rev 7:143–152
Böckermann M, Gieselmann A, Sorbi M et al (2015) Entwicklung und Evaluation einer internetbasierten begleiteten Selbsthilfe-Intervention zur Bewältigung von Albtraumen. Z Psychiatr Psychol Psychother 63:117–124
Boerner J (1855) Das Alpdrücken: Seine Begründung und Verhütung. Carl Joseph Becker, Würzburg
Hansen K, Höfling V, Kröner-Borowik T et al (2013) Efficacy of psychological interventions aiming to reduce chronic nightmares: a meta-analysis. Clin Psychol Rev 33:146–155
Köthe M, Pietrowsky R (2001) Behavioral effects of nightmares and their correlations to personality patterns. Dreaming 11:43–52
Krakow B (2006) Nightmare complaints in treatment-seeking patients in clinical sleep medicine settings: diagnostic and treatment implications. Sleep 29:1313–1319
Krakow B, Zadra AL (2010) Imagery rehearsal therapy: principles and practice. Sleep Med Clin 5:289–298
Lancee J, Spoormaker VI, Van Den Bout J (2010) Cognitive-behavioral self-help treatment for nightmares: a randomized controlled trial. Psychother Psychosom 79:371–377
Lancee J, Spoormaker VI, Van Den Bout J (2011) Long-term effectiveness of cognitive–behavioural self-help intervention for nightmares. J Sleep Res 20:454–459
Levin R, Nielsen TA (2007) Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull 133:482–528
Nadorff MR, Nadorff DK, Germain A (2015) Nightmares: under-reported, undetected, and therefore untreated. J Clin Sleep Med 11:747–750
Nadorff MR, Nazem S, Fiske A (2011) Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep 34:93–98
Schredl M (2013) Nightmare disorder. In: Kushida C (ed) The encyclopedia of sleep. Academic Press, Waltham, MA, pp 219–224
Schredl M (2010) Nightmare frequency and nightmare topics in a representative German sample. Eur Arch Psychiatry Clin Neurosci 260:565–570
Schredl M (2013) Nightmare frequency in a representative German sample. Int J Dream Res 6:119–122
Schredl M (2010) Nightmares: an under-diagnosed and undertreated condition? Commentary on Li et al. Prevalence and correlates of frequent nightmares: a community-based 2‑phase study. Sleep 33:733–734
Schredl M (2013) Seeking professional help for nightmares: a representative study. Eur J Psychiatry 27:259–264
Schredl M, Berres S, Klingauf A et al (2014) The Mannheim dream questionnaire (MADRE): retest reliability, age and gender effects. Int J Dream Res 7:141–147
Schredl M, Binder R, Feldmann S et al (2012) Dreaming in patients with sleep disorders: a multicenter study. Somnologie 16:32–42
Schredl M, Dehmlow L, Schmitt J (2016) Interest in information about nightmares in patients with sleep disorders. J Clin Sleep Med 12:973–977
Schredl M, Göritz AS (2014) Umgang mit Alpträumen in der Allgemeinbevölkerung: Eine Online-Studie. Psychother Psychosom Med Psychol 64:192–196
Schredl M, Reinhard I (2011) Gender differences in nightmare frequency: a meta-analysis. Sleep Med Rev 15:115–121
Schredl M, Schmitt J (2009) Dream recall frequency and nightmare frequency in patients with sleep disordered breathing. Somnologie 13:12–17
Schredl M, Schmitt J, Hein G et al (2006) Nightmares and oxygen desaturations: is sleep apnea related to heightened nightmare frequency? Sleep Breath 10:203–209
Stumbrys T, Erlacher D, Schredl M (2013) Reliability and stability of lucid dream and nightmare frequency scales. Int J Dream Res 6:123–126
Swart ML, Van Schagen AM, Lancee J et al (2013) Prevalence of nightmare disorder in psychiatric outpatients. Psychother Psychosom 82:267–268
Thünker J, Norpoth M, Aspern MV et al (2014) Nightmares: knowledge and attitudes in health care providers and nightmare sufferers. J Public Health Epidemiol 6:223–228
Thünker J, Pietrowsky R (2011) Alpträume – Ein Therapiemanual. Hogrefe, Göttingen
Yucel DE, Van Emmerik AAP, Souama C et al (2019) Comparative efficacy of imagery rehearsal therapy and prazosin in the treatment of trauma-related nightmares in adults: A meta-analysis of randomized controlled trials. Sleep Med Rev 50:101248
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
M. Schredl, K. Lüth, and J. Schmitt declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schredl, M., Lüth, K., Schmitt, J. et al. Interest in telephone nightmare counselling in patients with sleep-related breathing disorders. Somnologie 24 (Suppl 1), 2–10 (2020). https://doi.org/10.1007/s11818-020-00254-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11818-020-00254-9