Abstract
Purpose
To assess cognitive functioning in occupationally active non-central nervous system cancer survivors with cognitive complaints using neuropsychological tests, and to investigate the association between (1) formally assessed cognitive functioning and self-reported work-related outcomes and (2) self-reported cognitive functioning at work and self-reported work-related outcomes.
Methods
Baseline data of a multicenter, randomized controlled trial (n = 279) were used. Associations between neuropsychological test performance (Amsterdam Cognition Scan) and self-reported cognitive functioning (Cognitive Symptom Checklist-work) with work ability (Work Ability Index) and work functioning (Work Role Functioning Questionnaire) were examined using multivariate linear regression.
Results
Thirty percent of cancer survivors had lower than expected performance on neuropsychological tests. Higher overall neuropsychological test performance was associated with better work ability (Cohen’s f2 = 0.014) and physical functioning at work (Cohen’s f2 = 0.13). Furthermore, higher motor performance was associated with better work ability (Cohen’s f2 = 0.018). In addition, self-reported work-related cognitive complaints were associated with self-reported work-related outcomes (Cohen’s f2 = 0.13–0.35).
Conclusions
The percentage of cancer survivors with lower than expected performance on neuropsychological tests exceeded the percentage expected in a normal population. This neuropsychological test performance was weakly associated with various aspects of work ability and work functioning. Stronger associations were found between self-reported cognitive functioning at work with self-reported work-related outcomes.
Implications for cancer survivors.
A cognitive rehabilitation approach that specifically aims at reducing cognitive symptoms at work could be a valuable part of interventions that aim to improve work-related outcomes.
Trial registration
The study is registered at ClinicalTrials.gov (NCT03900806) at 03 April 2019 (current status: ongoing), https://clinicaltrials.gov/ct2/show/NCT03900806?term=NCT03900806&draw=2&rank=1


Similar content being viewed by others
References
Wefel JS, Kesler SR, Noll KR, Schagen SB. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA a cancer journal for clinicians. 2015;65:123–38. https://doi.org/10.3322/caac.21258.
Ahles TA, Root JC. Cognitive effects of cancer and cancer treatments. Annu Rev Clin Psychol. 2018. https://doi.org/10.1146/annurev-clinpsy-050817-084903.
Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int rev psychiatry (Abingdon, England). 2014;26:102–13. https://doi.org/10.3109/09540261.2013.864260.
Schagen SB et al. Monitoring and optimising cognitive function in cancer patients: present knowledge and future directions. EJC supplements : EJC : official journal of EORTC, European Organization for Research and Treatment of Cancer ... [et al.] 12, 29–40, https://doi.org/10.1016/j.ejcsup.2014.03.003 (2014).
Mayo SJ, et al. Cancer-related cognitive impairment in patients with non-central nervous system malignancies: an overview for oncology providers from the MASCC Neurological Complications Study Group. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2020. https://doi.org/10.1007/s00520-020-05860-9.
Boykoff N, Moieni M, Subramanian SK. Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. Journal of cancer survivorship : research and practice. 2009;3:223–32. https://doi.org/10.1007/s11764-009-0098-x.
Hardy SJ, Krull KR, Wefel JS, Janelsins M. Cognitive changes in cancer survivors. American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Annual Meeting. 2018;38:795–806. https://doi.org/10.1200/edbk_201179.
Harrison RA, Wefel JS. Neurocognitive function in adult cancer patients. Neurol Clin. 2018;36:653–74. https://doi.org/10.1016/j.ncl.2018.04.014.
Duijts SF, Kieffer JM, van Muijen P, van der Beek AJ. Sustained employability and health-related quality of life in cancer survivors up to four years after diagnosis. Acta Oncol. 2017;56:174–82. https://doi.org/10.1080/0284186X.2016.1266083.
de Boer AG. The European Cancer and Work Network: CANWON. J Occup Rehabil. 2014;24:393–8. https://doi.org/10.1007/s10926-013-9474-5.
de Boer A, et al. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD007569.pub3.
Von Ah D, et al. Cancer, cognitive impairment, and work-related outcomes: an integrative review. Oncol Nurs Forum. 2016;43:602–16. https://doi.org/10.1188/16.ONF.602-616.
de Boer AG, et al. Long-term work retention after treatment for cancer: a systematic review and meta-analysis. Journal of cancer survivorship : research and practice. 2020;14:135–50. https://doi.org/10.1007/s11764-020-00862-2.
Mehnert A, de Boer A, Feuerstein M. Employment challenges for cancer survivors. Cancer. 2013;119(Suppl 11):2151–9. https://doi.org/10.1002/cncr.28067.
Tamminga SJ, et al. Factors associated with an adverse work outcome in breast cancer survivors 5–10 years after diagnosis: a cross-sectional study. (2019);13, 108–116, https://doi.org/10.1007/s11764-018-0731-7.
Bijker R, et al. Functional impairments and work-related outcomes in breast cancer survivors: a systematic review. J Occup Rehabil. 2018;28:429–51. https://doi.org/10.1007/s10926-017-9736-8.
Von Ah D, Storey S, Crouch A. Relationship between self-reported cognitive function and work-related outcomes in breast cancer survivors. J Cancer Surviv. 2018;12:246–55.
Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77:109–30. https://doi.org/10.1016/j.critrevonc.2010.01.004.
Von Ah D, Crouch A. Relationship of perceived everyday cognitive function and work engagement in breast cancer survivors. Support Care Cancer. 2021. https://doi.org/10.1007/s00520-020-05950-8.
Lange M, et al. Cancer-related cognitive impairment: an update on state of the art, detection, and management strategies in cancer survivors. Annals of oncology : official journal of the European Society for Medical Oncology. 2019;30:1925–40. https://doi.org/10.1093/annonc/mdz410.
Nieuwenhuijsen K, de Boer A, Spelten E, Sprangers MA, Verbeek JH. The role of neuropsychological functioning in cancer survivors’ return to work one year after diagnosis. Psychooncology. 2009;18:589–97. https://doi.org/10.1002/pon.1439.
Calvio L, Peugeot M, Bruns GL, Todd BL, Feuerstein M. Measures of cognitive function and work in occupationally active breast cancer survivors. J Occup Environ Med. 2010;52:219–27. https://doi.org/10.1097/JOM.0b013e3181d0bef7.
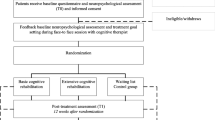
Klaver K, et al. Internet-based cognitive rehabilitation for WORking Cancer survivors (i-WORC): study protocol of a randomized controlled trial. Trials. 2020;21:664. https://doi.org/10.1186/s13063-020-04570-1.
Feenstra HEM, Murre JMJ, Vermeulen IE, Kieffer JM, Schagen SB. Reliability and validity of a self-administered tool for online neuropsychological testing: The Amsterdam Cognition Scan. J Clin Exp Neuropsychol, (2017); 1–21, https://doi.org/10.1080/13803395.2017.1339017.
Feenstra HE, Vermeulen IE, Murre JM, Schagen SB. Online self-administered cognitive testing using the Amsterdam cognition scan: establishing psychometric properties and normative data. J Med Internet Res. 2018;20:e192. https://doi.org/10.2196/jmir.9298.
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A. Work ability index. (Institute of Occupational Health Helsinki, 1994).
Ahlstrom L, Grimby-Ekman A, Hagberg M, Dellve L. The work ability index and single-item question: associations with sick leave, symptoms, and health–a prospective study of women on long-term sick leave. Scand J Work Environ Health. 2010;36:404–12.
El Fassi M, et al. Work ability assessment in a worker population: comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health. 2013;13:305. https://doi.org/10.1186/1471-2458-13-305.
Abma FI, van der Klink JJ, Bultmann U. The work role functioning questionnaire 2.0 (Dutch version): examination of its reliability, validity and responsiveness in the general working population. J occup rehabil. 2013;23:135–47. https://doi.org/10.1007/s10926-012-9379-8.
Dorland HF, et al. Work functioning trajectories in cancer patients: results from the longitudinal Work Life after Cancer (WOLICA) study. Int J Cancer. 2017;141:1751–62. https://doi.org/10.1002/ijc.30876.
Dorland HF, et al. The Cognitive Symptom Checklist-Work in cancer patients is related with work functioning, fatigue and depressive symptoms: a validation study. J cancer survivorship : res pract. 2016;10:545–52. https://doi.org/10.1007/s11764-015-0500-9.
Wefel JS, Vardy J, Ahles T, Schagen SB. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12:703–8. https://doi.org/10.1016/s1470-2045(10)70294-1.
Leys C, Ley C, Klein O, Bernard P, Licata L. Detecting outliers: do not use standard deviation around the mean, use absolute deviation around the median. J Exp Soc Psychol. 2013;49:764–6.
Selya AS, Rose JS, Dierker LC, Hedeker D, Mermelstein RJ. A practical guide to calculating Cohen’s f(2), a measure of local effect size, from PROC MIXED. Front Psychol. 2012;3:111. https://doi.org/10.3389/fpsyg.2012.00111.
Ahles TA, Root JC. Cognitive effects of cancer and cancer treatments. Annu Rev Clin Psychol. 2018;14:425–51. https://doi.org/10.1146/annurev-clinpsy-050817-084903.
Vardy JL, Dhillon HM. “Mind the gaps”: cognition and cancer. Psychooncology. 2018;27:10–2. https://doi.org/10.1002/pon.4582.
Cerulla Torrente N, Navarro Pastor JB, de la OsaChaparro N. Systematic review of cognitive sequelae of non-central nervous system cancer and cancer therapy. J cancer survivorship : res pract. 2020;14:464–82. https://doi.org/10.1007/s11764-020-00870-2.
Hardy SJ, Krull KR, Wefel JS, Janelsins M. Cognitive changes in cancer survivors. American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Annual Meeting, (2018); 795–806, https://doi.org/10.1200/edbk_201179.
Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100:2292–9. https://doi.org/10.1002/cncr.20272.
Duijts SF, et al. Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psychooncology. 2014;23:481–92. https://doi.org/10.1002/pon.3467.
Paalman CH, et al. Employment and social benefits up to 10 years after breast cancer diagnosis: a population-based study. Br J Cancer. 2016;114:81–7. https://doi.org/10.1038/bjc.2015.431.
Boscher C, et al. Perceived cognitive impairment in breast cancer survivors and its relationships with psychological factors. Cancers (Basel) (2020);12, https://doi.org/10.3390/cancers12103000.
Wolvers MDJ, Leensen MCJ, Groeneveld IF, Frings-Dresen MHW, De Boer A. Longitudinal associations between fatigue and perceived work ability in cancer survivors. J Occup Rehabil. 2019;29:540–9. https://doi.org/10.1007/s10926-018-9814-6.
Von Ah D, et al. Relationship of self-reported attentional fatigue to perceived work ability in breast cancer survivors. Cancer Nurs. 2017;40:464–70. https://doi.org/10.1097/ncc.0000000000000444.
Dorland HF, et al. Fatigue and depressive symptoms improve but remain negatively related to work functioning over 18 months after return to work in cancer patients. J cancer survivorship : res pract. 2018;12:371–8. https://doi.org/10.1007/s11764-018-0676-x.
Markovic C, Mackenzie L, Lewis J, Singh M. Working with cancer: A pilot study of work participation among cancer survivors in Western Sydney. Aust Occup Ther J. 2020;67:592–604. https://doi.org/10.1111/1440-1630.12685.
Horsboel TA, et al. Are fatigue, depression and anxiety associated with labour market participation among patients diagnosed with haematological malignancies? A prospective study Psychooncology. 2015;24:408–15. https://doi.org/10.1002/pon.3658.
Dorland HF, et al. Work functioning trajectories in cancer patients: results from the longitudinal Work Life after Cancer (WOLICA) study. Int J Cancer. 2017;141:1751–62. https://doi.org/10.1002/ijc.30876.
van Muijen P, Duijts SF, Bonefaas-Groenewoud K, van der Beek AJ, Anema JR. Factors associated with work disability in employed cancer survivors at 24-month sick leave. BMC Cancer. 2014;14:236. https://doi.org/10.1186/1471-2407-14-236.
Boelhouwer IG, Vermeer W, van Vuuren T. Late effects of cancer (treatment) and work ability: guidance by managers and professionals. BMC Public Health. 2021;21:1255. https://doi.org/10.1186/s12889-021-11261-2.
Von Ah D, Jansen C, Allen DH, Schiavone RM, Wulff J. Putting evidence into practice: evidence-based interventions for cancer and cancer treatment-related cognitive impairment. Clin J Oncol Nurs. 2011;15:607–15. https://doi.org/10.1188/11.CJON.607-615.
Gehring K, et al. in Cognitive rehabilitation and neuroimaging: examining the evidence from brain to behavior (eds John DeLuca, Nancy D. Chiaravalloti, & Erica Weber) 221–254 (Springer International Publishing, 2020).
Acknowledgements
We thank cancer survivors for their participation in this study. We thank Jacobien Kieffer and Joost Agelink van Rentergem for statistical counseling.
Funding
This trial is funded by the Dutch Cancer Society (grant number NKI 2015–7937).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kete Klaver. The first draft of the manuscript was written by Kete Klaver and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All procedures were reviewed and approved by the Medical Ethical Board Committee of the Netherlands Cancer Institute (METC18.0036).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Klaver, K.M., Duijts, S.F.A., Geusgens, C.A.V. et al. Neuropsychological test performance and self-reported cognitive functioning associated with work-related outcomes in occupationally active cancer survivors with cognitive complaints. J Cancer Surviv 18, 412–424 (2024). https://doi.org/10.1007/s11764-022-01223-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01223-x