Abstract
Objectives
Prolonged air leak after pulmonary resection strongly influences chest tube duration and hospitalization. This prospective study aimed to report a series of experiences with a synthetic sealant (TissuePatch™) and compare them with a combination covering method (polyglycolic acid sheet + fibrin glue) for air leaks after pulmonary surgery.
Methods
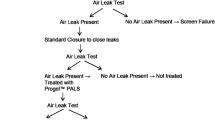
We included 51 patients (age: 20–89 years) who underwent lung resection. Patients who presented with alveolar air leak during the intraoperative water sealing test were randomly assigned to the TissuePatch™ or combination covering method groups. The chest tube was removed when there was no air leak over a period of 6 h, and no active bleeding under continuous monitoring using a digital drainage system. The chest tube duration was assessed, and various perioperative factors (such as the index of prolonged air leak score) were evaluated.
Results
Twenty (39.2%) patients developed intraoperative air leak; ten patients received TissuePatch™; and one patient who was receiving TissuePatch™ switched to the combination covering method because of broken TissuePatch™. The chest tube duration, index of prolonged air leak score, prolonged air leak, other complications, and postoperative hospitalization in both groups were similar. No TissuePatch™-related adverse events were reported.
Conclusions
Results from the use of TissuePatch™ were almost similar to those associated with the use of combination covering method in preventing prolonged postoperative air leak after pulmonary resection. Randomized, double-arm studies are required to confirm the efficacy of TissuePatch™ observed during this study.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request after approval from the Ethical Committee of Toyama University Hospital. The period ends 3 months to 3 years after publication.
References
Seely AJE, Ivanovic J, Threader J, Al-Hussaini A, Al-Shehab D, Ramsay T, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg. 2010;90:936–42. https://doi.org/10.1016/j.athoracsur.2010.05.014.
Dugan KC, Laxmanan B, Murgu S, Hogarth DK. Management of persistent air leaks. Chest. 2017;152:417–23. https://doi.org/10.1016/j.chest.2017.02.020.
Varela G, Jiménez MF, Novoa N, Aranda JL. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg. 2005;27:329–33. https://doi.org/10.1016/j.ejcts.2004.11.005.
Sakata KK, Reisenauer JS, Kern RM, Mullon JJ. Persistent air leak—Review. Respir Med. 2018;137:213–8. https://doi.org/10.1016/j.rmed.2018.03.017.
Rivera C, Bernard A, Falcoz PE, Thomas P, Schmidt A, Bénard S, et al. Characterization and prediction of prolonged air leak after pulmonary resection: a nationwide study setting up the index of prolonged air leak. Ann Thorac Surg. 2011;92:1062–8. https://doi.org/10.1016/j.athoracsur.2011.04.033.
Brunelli A, Monteverde M, Borri A, Salati M, Marasco RD, Fianchini A. Predictors of prolonged air leak after pulmonary lobectomy. Ann Thorac Surg. 2004;77:1205–10. https://doi.org/10.1016/j.athoracsur.2003.10.082.
Kim WH, Lee HC, Ryu HG, Yoon HK, Jung CW. Intraoperative ventilatory leak predicts prolonged air leak after lung resection: a retrospective observational study. PLoS ONE. 2017;12:e0187598. https://doi.org/10.1371/journal.pone.0187598.
Liang S, Ivanovic J, Gilbert S, Maziak DE, Shamji FM, Sundaresan RS, et al. Quantifying the incidence and impact of postoperative prolonged alveolar air leak after pulmonary resection. J Thorac Cardiovasc Surg. 2013;145:948–54. https://doi.org/10.1016/j.jtcvs.2012.08.044.
Malapert G, Hanna HA, Pages PB, Bernard A. Surgical sealant for the prevention of prolonged air leak after lung resection: meta-analysis. Ann Thorac Surg. 2010;90:1779–85. https://doi.org/10.1016/j.athoracsur.2010.07.033.
Kawai H, Harada K, Ohta H, Tokushima T, Oka S. Prevention of alveolar air leakage after video-assisted thoracic surgery: comparison of the efficacy of methods involving the use of fibrin glue. Thorac Cardiovasc Surg. 2012;60:351–5. https://doi.org/10.1055/s-0031-1293599.
Ikeda T, Sasaki M, Yamada N, Takamori A, Tanabe S, Okada A, et al. Controlling air leaks using free pericardial fat pads as surgical sealant in pulmonary resection. Ann Thorac Surg. 2015;99:1170–5. https://doi.org/10.1016/j.athoracsur.2014.11.040.
Hugen N, Hekma EJ, Claessens NJM, Smit HJM, Reijnen MMPJ. Efficacy of an autologous blood patch for prolonged air leak: a systematic review. Ann Thorac Surg. 2022;114:1064–71. https://doi.org/10.1016/j.athoracsur.2021.05.047.
Gilbert S, McGuire AL, Maghera S, Sundaresan SR, Seely AJ, Maziak DE, et al. Randomized trial of digital versus analog pleural drainage in patients with or without a pulmonary air leak after lung resection. J Thorac Cardiovasc Surg. 2015;150:1243–9. https://doi.org/10.1016/j.jtcvs.2015.08.051.
Zhang R, Bures M, Höffler HK, Zinne N, Länger F, Bisdas T, et al. TissuePatch™ as a novel synthetic sealant for repair of superficial lung defect: in vitro tests results. Ann Surg Innov Res. 2012;6:12. https://doi.org/10.1186/1750-1164-6-12.
Thompson I. A review of the composition and constituent materials of TissuePatchTM. https://www.tissuemed.com/wp-content/uploads/2015/06/TB2001.pdf. Accessed 2022
Ambridge A. Burst pressure comparison of TissuePatchTM with three different surgical sealants used in Thoracic Surgery. https://www.tissuemed.com/wp-content/uploads/2015/06/TB26-Burst-Pressure-Performance-TPT.pdf. Accessed 2022
Mandley D. The fate of TissuePatchTM: tissue response and in vivo degradation. https://www.tissuemed.com/wp-content/uploads/2015/06/CS6401-The-fate-of-TissuePatch.pdf. Accessed 2022
Homma T, Shimada Y, Tanabe K. Decreased postoperative complications, neuropathic pain and epidural anesthesia-free effect of uniportal video-assisted thoracoscopic anatomical lung resection: a single-center initial experience of 100 cases. J Thorac Dis. 2022;14:3154–66. https://doi.org/10.21037/jtd-22-6.
Homma T, Kitamura N, Ojima T, Akemoto Y, Hida Y, Yoshimura N. Initial experiences of robot-assisted thoracic surgery: safety approach and comparison with video-assisted thoracoscopic surgery. Jpn J Chest Surg. 2019;33:113–21. https://doi.org/10.2995/jacsurg.33.113.
Honma T, Shinno H, Miyazawa H, Noto H. Therapeutic strategy for intractable pneumothorax–combined use of bronchial occlusion therapy and high-negative pressure pleurodesis-. Jpn J Chest Surg. 2009;23:114–9. https://doi.org/10.2995/jacsurg.23.114.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
National Cancer Institute. Cancer therapy evaluation program. Common terminology criteria for adverse events (CTCAE). v.4.0. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50. Accessed 2022
Homma T, Ojima T, Yamamoto Y, Shimada Y, Akemoto Y, Kitamura N, et al. Utility of the sliding lung sign for the prediction of preoperative intrathoracic adhesions. J Thorac Dis. 2020;12:4224–32. https://doi.org/10.21037/jtd-20-886.
NITE chemical risk information platform. https://www.nite.go.jp/chem/chrip/chrip_search/systemTop. Accessed 2022
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Funding
This study was funded by the Toyama Prefecture Citizens’ Personal Development Foundation (TomiHito #52).
Author information
Authors and Affiliations
Contributions
Conception and design, administrative support, provision of study materials or access to patients, collection and assembly of data, data analysis and interpretation, manuscript writing, and final approval of the manuscript: TH.
Corresponding author
Ethics declarations
Conflict of interest
The author has no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 53230 KB)
Supplementary file2 (MP4 89405 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Homma, T. A series of experiences with TissuePatch™ for alveolar air leak after pulmonary resection. Gen Thorac Cardiovasc Surg 71, 570–576 (2023). https://doi.org/10.1007/s11748-023-01921-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-023-01921-y