Abstract
Objectives
To determine the role of adding open distal anastomosis to proximal aortic aneurysm repairs in bicuspid aortic valve (BAV) patients.
Methods
Retrospective review was performed of 1132 patients at our Aortic Center between 2005 and 2019. Inclusion criteria were all patients diagnosed with a BAV who underwent proximal aortic aneurysm repair with open or clamped distal anastomosis. Exclusion criteria were patients without a BAV, age < 18 years, aortic arch diameter ≥ 4.5 cm, type A aortic dissection, previous ascending aortic replacement, ruptured aneurysm, and endocarditis. Propensity score matching in a 2:1 ratio (220 clamped: 121 open repairs) on 18 variables was performed.
Results
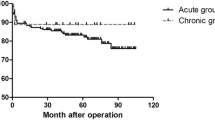
Median follow-up time was 45.6 months (range 7.2–143.4 months). In the matched groups, no significant differences were observed between the respective open and clamped distal anastomosis groups for Kaplan Meier 10-year survival (86.9% vs. 92.9%; p = 0.05) and landmark survival analysis after 1 year (90.6%; vs. 93.3%; p = 0.39). Overall incidence of aortic arch-related reintervention was low (n = 3 total events). In-hospital complications were not significantly different in the open with respect to the clamped repair group, including in-hospital mortality (2.5% vs. 0.5%; p = 0.13) and stroke (0% vs. 0.9%; p = 0.54). In multivariable analysis, open distal anastomosis repair was not associated with long-term mortality (Hazard Ratio (HR) 1.98; p = 0.06).
Conclusion
We found no significant inter-group differences in survival, reintervention, or in-hospital complication rates, with low rates of mortality, and aortic arch-related reintervention, suggesting adding open distal anastomosis may not provide benefit in BAV patients undergoing proximal aortic aneurysm repairs.



Similar content being viewed by others
References
Michelena HI, Khanna AD, Mahoney D, et al. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011;306(10):1104–12. https://doi.org/10.1001/JAMA.2011.1286.
Fazel SS, Mallidi HR, Lee RS, et al. The aortopathy of bicuspid aortic valve disease has distinctive patterns and usually involves the transverse aortic arch. J Thorac Cardiovasc Surg. 2008. https://doi.org/10.1016/J.JTCVS.2008.01.022.
Borger MA, Preston M, Ivanov J, et al. Should the ascending aorta be replaced more frequently in patients with bicuspid aortic valve disease? J Thorac Cardiovasc Surg. 2004;128(5):677–83. https://doi.org/10.1016/j.jtcvs.2004.07.009.
Borger MA, Fedak PWM, Stephens EH, et al. The American association for thoracic surgery consensus guidelines on bicuspid aortic valve-related aortopathy: full online-only version. J Thorac Cardiovasc Surg. 2018;156(2):e41–74. https://doi.org/10.1016/J.JTCVS.2018.02.115.
Etz CD, Haunschild J, Girdauskas E, et al. Surgical management of the aorta in BAV patients. Prog Cardiovasc Dis. 2020;63(4):475–81. https://doi.org/10.1016/J.PCAD.2020.06.013.
Coady MA, Rizzo JA, Hammond GL, Kopf GS, Elefteriades JA. Surgical intervention criteria for thoracic aortic aneurysms: a study of growth rates and complications. Ann Thorac Surg. 1999;67(6):1922–6. https://doi.org/10.1016/S0003-4975(99)00431-2.
Pressler V, NcNamara JJ. Aneurysm of the thoracic aorta review of 260 cases. J Thorac Cardiovasc Surg. 1985;89(1):50–4. https://doi.org/10.1016/s0022-5223(19)38847-6.
Hiratzka LF, Bakris GL, Beckman JA, et al. ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American college of cardiology foundation/American heart association task force on practice guidelines, American association for thoracic surgery, American college of radiology, American stroke association, society of cardiovascular anesthesiologists, society for cardiovascular angiography and interventions, society of interventional radiology, society of thoracic surgeons, and society for vascular medicine. Circulation. 2010. https://doi.org/10.1161/CIR.0B013E3181D4739E.
Singh R, Yamanaka K, Reece TB. Hemiarch: the real operation for ascending aortic aneurysm. Semin Cardiothorac Vasc Anesth. 2016;20(4):303–6. https://doi.org/10.1177/1089253216672438.
Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014;35(41):2873–926. https://doi.org/10.1093/eurheartj/ehu281.
Malaisrie SC, Duncan BF, Mehta CK, et al. The addition of hemiarch replacement to aortic root surgery does not affect safety. J Thorac Cardiovasc Surg. 2015;150(1):118-124.e2. https://doi.org/10.1016/j.jtcvs.2015.03.020.
Rylski B, Milewski RK, Bavaria JE, et al. Long-term results of aggressive hemiarch replacement in 534 patients with type A aortic dissection. J Thorac Cardiovasc Surg. 2014;148(6):2981–5. https://doi.org/10.1016/J.JTCVS.2014.05.093.
Greason KL, Crestanello JA, King KS, et al. Open hemiarch versus clamped ascending aorta replacement for aortopathy during initial bicuspid aortic valve replacement. J Thorac Cardiovasc Surg. 2021;161(1):12-20.e2. https://doi.org/10.1016/j.jtcvs.2019.09.028.
Moon MR, Sundt TM, Pasque MK, et al. Does the extent of proximal or distal resection influence outcome for type A dissections? Ann Thorac Surg. 2001;71(4):1244–9. https://doi.org/10.1016/S0003-4975(00)02610-2.
Svensson LG, Crawford ES, Hess KR, et al. Deep hypothermia with circulatory arrest: determinants of stroke and early mortality in 656 patients. J Thorac Cardiovasc Surg. 1993;106(1):19–31. https://doi.org/10.1016/s0022-5223(19)33737-7.
Khaladj N, Shrestha M, Meck S, et al. Hypothermic circulatory arrest with selective antegrade cerebral perfusion in ascending aortic and aortic arch surgery: a risk factor analysis for adverse outcome in 501 patients. J Thorac Cardiovasc Surg. 2008;135(4):908–14. https://doi.org/10.1016/j.jtcvs.2007.07.067.
Cooper WA, Duarte IG, Thourani VH, et al. Hypothermic circulatory arrest causes multisystem vascular endothelial dysfunction and apoptosis. Ann Thorac Surg. 2000;69(3):696–702. https://doi.org/10.1016/S0003-4975(99)01524-6.
Lai DT, Robbins RC, Mitchell; R Scott, et al. Does profound hypothermic circulatory arrest improve survival in patients with acute type A aortic dissection? Circulation. 2002. https://doi.org/10.1161/01.cir.0000032890.55215.27.
Ito T. Effect of deep hypothermia on cerebral hemodynamics during selective cerebral perfusion with systemic circulatory arrest. Jpn J Thorac Cardiovasc Surg. 2002;50:109–15. https://doi.org/10.1007/BF02913471.
Kamiya H, Hagl C, Kropivnitskaya I, et al. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: a propensity score analysis. J Thorac Cardiovasc Surg. 2007. https://doi.org/10.1016/j.jtcvs.2006.09.045.
Ergin MA, Griepp EB, Lansman SL, Galla JD, Levy M, Griepp RB. Hypothermic circulatory arrest and other methods of cerebral protection during operations on the thoracic aorta. J Card Surg. 1994;9(5):525–37. https://doi.org/10.1111/j.1540-8191.1994.tb00886.x.
Merkle J, Sabashnikov A, Deppe AC, et al. Impact of ascending aortic, hemiarch and arch repair on early and long-term outcomes in patients with Stanford A acute aortic dissection. Ther Adv Cardiovasc Dis. 2018;12(12):327–40. https://doi.org/10.1177/1753944718801568.
Pearsall C, Blitzer D, Zhao Y, et al. Long-term outcome of hemiarch replacement in a proximal aortic aneurysm repair: analysis of over 1000 patients. Eur J Cardiothorac Surg. 2022. https://doi.org/10.1093/EJCTS/EZAB571.
Bilkhu R, Youssefi P, Soppa G, et al. Fate of the aortic arch following surgery on the aortic root and ascending aorta in bicuspid aortic valve. Ann Thorac Surg. 2018;106(3):771–6. https://doi.org/10.1016/J.ATHORACSUR.2018.03.052.
Abdulkareem N, Soppa G, Jones S, Valencia O, Smelt J, Jahangiri M. Dilatation of the remaining aorta after aortic valve or aortic root replacement in patients with bicuspid aortic valve: a 5-year follow-up. Ann Thorac Surg. 2013;96(1):43–9. https://doi.org/10.1016/J.ATHORACSUR.2013.03.086.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107. https://doi.org/10.1002/sim.3697.
Daru J, Zamora J, Fernández-Félix BM, et al. Risk of maternal mortality in women with severe anaemia during pregnancy and post partum: a multilevel analysis. Lancet Glob Heal. 2018;6(5):e548–54. https://doi.org/10.1016/S2214-109X(18)30078-0.
Volinsky CT, Raftery AE. Bayesian information criterion for censored survival models. Biometrics. 2000;56(1):256–62. https://doi.org/10.1111/j.0006-341X.2000.00256.x.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496. https://doi.org/10.2307/2670170.
Kuk D, Varadhan R. Model selection in competing risks regression. Stat Med. 2013;32(18):3077–88. https://doi.org/10.1002/sim.5762.
Kozlov BN, Panfilov DS, Sonduev EL, Lukinov VL. Ascending aortic aneurysm: propensity score matching analysis of hemiarch and non-hemiarch replacement. Russ J Cardiol. 2020;25(10):179–86. https://doi.org/10.15829/1560-4071-2020-3887.
Sultan I, Bianco V, Yazji I, et al. Hemiarch reconstruction versus clamped aortic anastomosis for concomitant ascending aortic aneurysm. Ann Thorac Surg. 2018;106(3):750–6. https://doi.org/10.1016/j.athoracsur.2018.03.078.
Youssefi P, Gomez A, He T, et al. Patient-specific computational fluid dynamics-assessment of aortic hemodynamics in a spectrum of aortic valve pathologies. J Thorac Cardiovasc Surg. 2017;153(1):8-20.e3. https://doi.org/10.1016/J.JTCVS.2016.09.040.
Della Corte A, Quarto C, Bancone C, et al. Spatiotemporal patterns of smooth muscle cell changes in ascending aortic dilatation with bicuspid and tricuspid aortic valve stenosis: focus on cell-matrix signaling. J Thorac Cardiovasc Surg. 2008. https://doi.org/10.1016/j.jtcvs.2007.09.009.
Guzzardi DG, Barker AJ, Van Ooij P, et al. Valve-related hemodynamics mediate human bicuspid aortopathy: insights from wall shear stress mapping. J Am Coll Cardiol. 2015;66(8):892. https://doi.org/10.1016/J.JACC.2015.06.1310.
Park CB, Greason KL, Suri RM, Michelena HI, Schaff HV, Sundt TM. Should the proximal arch be routinely replaced in patients with bicuspid aortic valve disease and ascending aortic aneurysm? J Thorac Cardiovasc Surg. 2011;142(3):602–7. https://doi.org/10.1016/j.jtcvs.2010.08.086.
Anzai I, Kriegel J, Kim I, et al. Should all patients with aortic aneurysm and bicuspid aortic valve also undergo hemiarch? JTCVS Open. 2021;5:39–43. https://doi.org/10.1016/j.xjon.2020.12.021.
Iribarne A, Keenan J, Benrashid E, et al. Imaging surveillance after proximal aortic operations: is it necessary? Ann Thorac Surg. 2017;103(3):734. https://doi.org/10.1016/J.ATHORACSUR.2016.06.085.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Isaac George has received Institutional funding to Columbia University from Edwards Lifesciences, Medtronic, Abbott Vascular, Boston Scientific, JenaValve. Dr. Isaac George has received speaker honoraria from Zimmer Biomet, Atricure, Neosurgery, Neptune Medical, Abbvie, Johnson & Johnson, Boston Scientific and owns stock in Valcare Medical, Durvena, CardioMech, Vdyne, MitreMedical, MITRx. Dr. Isaac George is a member of Edwards Surgical, Medtronic Surgical, Trisol Medical, Abbvie, Johnson & Johnson, Foldax Medical, Zimmer Biomet, Neosurgery, Abbvie, and Boston Scientific advisory boards. The remaining authors declare that they have no conflicts of interest.
Institutional review board (IRB) approval
This study was approved March 31st, 2020 by the IRB at Columbia University (AAAR2949).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pearsall, C., Allen, P.M., Zhao, Y. et al. The effect of adding an open distal anastomosis to proximal aneurysm repairs in bicuspid aortopathy. Gen Thorac Cardiovasc Surg 71, 455–463 (2023). https://doi.org/10.1007/s11748-023-01907-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-023-01907-w