Abstract
Background
A randomized trial of lobectomy versus segmentectomy for small-sized (≤ 20 mm) non-small cell lung cancer (NSCLC) showed that patients who had undergone segmentectomy had a significantly longer overall survival (OS) than those who had lobectomy. More attention is needed regarding the required extent of thoracic lymphadenectomy in patients with small-sized NSCLC who undergo sublobar resection.
Methods
The National Cancer Database was queried for patients with clinically node-negative NSCLC ≤ 20 mm who had undergone sublobar resection between 2004 and 2017. OS of NSCLC patients by the number of lymph node dissections (LNDs) was analyzed using log-rank tests and Cox proportional hazards model. The cutoff value of the LNDs was set to 10 according to the Commission on Cancer’s recommendation.
Results
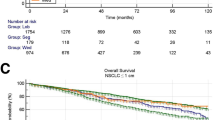
This study included 4379 segmentectomy and 23,138 wedge resection cases. The sequential improvement in the HRs by the number of LNDs was evident, and the HR was the lowest if the number of LNDs exceeded 10. Patients with ≤ 9 LNDs had a significantly shorter OS than those with ≥ 10 LNDs (hazard ratio [HR] 1.50, 95% confidence interval [CI] 1.40–1.61, P < 0.0001). Multivariable analysis revealed that performing ≤ 9 LNDs was an independent factor for predicting OS (HR for death: 1.34, 95% CI 1.24–1.44, P < 0.0001). These results remained significant in subgroup analyses by the type of sublobar resection (segmentectomy, wedge resection).
Conclusions
Performing ≥ 10 LNDs has a prognostic role in patients with small-sized NSCLC even if the resection is sublobar.


Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
National comprehensive cancer network. Non-small cell lung cancer (version 3.2020-February 11, 2020) available at: https://www2.Tri-kobe.Org/nccn/guideline/lung/english/non_small.Pdf. Accessed Sep 28 2022
Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (jcog0802/wjog4607l): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607–17.
Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with n0 or n1 (less than hilar) non-small cell carcinoma: results of the american college of surgery oncology group z0030 trial. J Thorac Cardiovasc Surg. 2011;141(3):662–70.
Lardinois D, Suter H, Hakki H, Rousson V, Betticher D, Ris HB. Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg. 2005;80(1):268–74 (Discussion 74-5).
Wu Y, Huang ZF, Wang SY, Yang XN, Ou W. A randomized trial of systematic nodal dissection in resectable non-small cell lung cancer. Lung Cancer. 2002;36(1):1–6.
Hishida T, Saji H, Watanabe SI, et al. A randomized phase iii trial of lobe-specific vs. systematic nodal dissection for clinical stage i–ii non-small cell lung cancer (jcog1413). Jpn J Clin Oncol. 2018;48(2):190–4.
Wang Y-N, Yao S, Wang C-L, et al. Clinical significance of 4l lymph node dissection in left lung cancer. J Clin Oncol. 2018;36(29):2935–42.
American college of surgeons coc quality of care measures 2020 surveys. Available at: https://www.Facs.Org/quality-programs/cancer/ncdb/qualitymeasurescocweb. Accessed Sep 28 2022
Howington JA, Blum MG, Chang AC, Balekian AA, Murthy SC. Treatment of stage i and ii non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e278S-e313S.
Okada M, Koike T, Higashiyama M, Yamato Y, Kodama K, Tsubota N. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg. 2006;132(4):769–75.
Le Pechoux CNP, Barlesi F, Faivre-Finn C, Lerouge D, Zalcman G, Antoni D, Lamezec B, Nestle U, Boisselier P, Thillays F, Paumier A, Dansin E, Peignaux K, Madelaine J, Pichon E, Larrouy A, Riesterer O, Lavole A, Bardet A. An international randomized trial, comparing post-operative conformal radiotherapy (port) to no port, in patients with completely resected non-small cell lung cancer (nsclc) and mediastinal n2 involvement: primary end-point analysis of lungart (ifct-0503, uk ncri, sakk). Ann Oncol. 2020;31(suppl_4):S1142–215. https://doi.org/10.1016/annonc/annonc325.
Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399(10335):1607–17.
Nakamura K, Saji H, Nakajima R, et al. A phase iii randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (jcog0802/wjog4607l). Jpn J Clin Oncol. 2010;40(3):271–4.
Yendamuri S, Dhillon SS, Groman A, et al. Effect of the number of lymph nodes examined on the survival of patients with stage i non-small cell lung cancer who undergo sublobar resection. J Thorac Cardiovasc Surg. 2018;156(1):394–402.
Osarogiagbon RU, Allen JW, Farooq A, Wu JT. Objective review of mediastinal lymph node examination in a lung cancer resection cohort. J Thorac Oncol. 2012;7(2):390–6.
Osarogiagbon RU, Miller LE, Ramirez RA, et al. Use of a surgical specimen-collection kit to improve mediastinal lymph-node examination of resectable lung cancer. J Thorac Oncol. 2012;7(8):1276–82.
Osarogiagbon RU, Ramirez RA, Wang CG, et al. Dual intervention to improve pathologic staging of resectable lung cancer. Ann Thorac Surg. 2013;96(6):1975–81.
Osarogiagbon RU, Sareen S, Eke R, et al. Audit of lymphadenectomy in lung cancer resections using a specimen collection kit and checklist. Ann Thorac Surg. 2015;99(2):421–7.
Lee JG, Lee CY, Park IK, et al. Number of metastatic lymph nodes in resected non-small cell lung cancer predicts patient survival. Ann Thorac Surg. 2008;85(1):211–5.
Nwogu CE, Groman A, Fahey D, et al. Number of lymph nodes and metastatic lymph node ratio are associated with survival in lung cancer. Ann Thorac Surg. 2012;93(5):1614–9.
Whitson BA, Groth SS, Maddaus MA. Surgical assessment and intraoperative management of mediastinal lymph nodes in non-small cell lung cancer. Ann Thorac Surg. 2007;84(3):1059–65.
Acknowledgements
We thank Mindy Flannagan for statistical assistance.
Funding
There are no sources of funding to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takefumi Komiya received travel fee from Merck and honoraria from Boehringer Ingelheim. All the authors declare no conflicts of interest in association with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11748_2022_1876_MOESM1_ESM.tiff
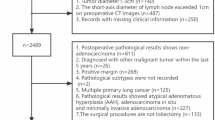
Supplementary file1 Supplemental Fig. 1. Study flow diagram of case eligibility. NSCLC, non-small cell lung cancer; NCDB, National Cancer Database. (TIFF 30956 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takamori, S., Komiya, T., Shimokawa, M. et al. Lymph node dissections and survival in sublobar resection of non-small cell lung cancer ≤ 20 mm. Gen Thorac Cardiovasc Surg 71, 189–197 (2023). https://doi.org/10.1007/s11748-022-01876-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01876-6