Abstract
Purpose
Food addiction (FA) following bariatric surgery (BS) has received a burst of attention in recent years due to its important contribution to obesity. Therefore, this study was conducted to explore the prevalence of FA disorder and its predictors 2 years after laparoscopic sleeve gastrectomy (LSG) and assess its relationship with physical activity (PA), body composition, and weight outcomes.
Materials and Methods
Four hundred fifty individuals who had undergone LSG 2 years prior to the study were enrolled. FA was diagnosed using the Yale Food Addiction Scale (YFAS). The collected data included body composition (fat mass (FM), fat-free mass (FFM)), PA, and nutritional intakes.
Results
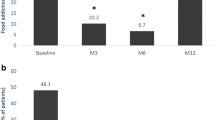
Eighty-nine subjects (about 20%) met the criteria for FA disorder. FA patients had significantly lower PA (p = 0.04) and higher weight (p < 0.001), BMI (p < 0.001), FM, and FFM (p = 0.01) compared to those without FA. Regarding weight and body composition changes, the finding reveals that FA patients (vs. non-FA) had a significantly less excess weight loss (EWL%) (p < 0.001) and total weight loss (TWL%) (p = 0.05) as well as a higher FFM loss (kg) (p = 0.04) (linear regression analysis). A younger age (p trend = 0.01), higher BMI (p trend = 0.04), and more excess weight (p trend = 0.03) were related to higher odds of FA disorder at second year after LSG (logistic regression analysis).
Conclusion
The results showed that FA was highly prevalent 2 years after LSG. In addition, FA disorder was associated with negative long-term outcomes following LSG. Younger individuals with more excess weight and higher BMI at baseline are more vulnerable to FA.
Graphical abstract


Similar content being viewed by others
References
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database of Systematic Reviews. 2014;8:1–201. https://doi.org/10.1002/14651858.CD003641.pub4.
Carlin AM, Zeni TM, English WJ, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013;257(5):791–7.
Spaniolas K, Kasten KR, Brinkley J, et al. The changing bariatric surgery landscape in the USA. Obes Surg. 2015;25(8):1544–6.
Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–25.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18(6):648–51.
Ben-Porat T, Weiss R, Sherf-Dagan S, Rottenstreich A, Kaluti D, Khalaileh A, Gazala MA, Ben-Anat TZ, Mintz Y, Sakran N, Elazary R. Food addiction and binge eating during one year following sleeve gastrectomy: prevalence and implications for postoperative outcomes. Obesity Surgery. 2021;31(2):603–611.
Yanos BR, Saules KK, Schuh LM, et al. Predictors of lowest weight and long-term weight regain among Roux-en-Y gastric bypass patients. Obes Surg. 2015;25(8):1364–70.
Ivezaj V, Wiedemann AA, Grilo CM. Food addiction and bariatric surgery: a systematic review of the literature. Obes Rev. 2017;18(12):1386–97.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52(2):430–6.
Pedram P, Sun G. Hormonal and dietary characteristics in obese human subjects with and without food addiction. Nutrients. 2015;7(1):223–38.
Meule A, Gearhardt AN. Food addiction in the light of DSM-5. Nutrients. 2014;6(9):3653–71.
Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3(1):1–7.
Sevinçer GM, Konuk N, Bozkurt S, et al. Food addiction and the outcome of bariatric surgery at 1-year: prospective observational study. Psychiatry Res. 2016;244:159–64.
Ciangura C, Bouillot JL, Lloret-Linares C, et al. Dynamics of change in total and regional body composition after gastric bypass in obese patients. Obesity. 2010;18(4):760–5.
Chaston TB, Dixon J, O'Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes. 2007;31(5):743–50.
Panahi A, Haghayegh SA. Developing the Persian version of Yale Food Addiction Scale and assessing its psychometric properties. Iran J Psychiatry Clin Psychol. 2019;25(4):8.
Clark SM, Saules KK. Validation of the Yale Food Addiction Scale among a weight-loss surgery population. Eat Behav. 2013;14(2):216–9.
Faucher P, Aron-Wisnewsky J, Ciangura C, et al. Changes in body composition, comorbidities, and nutritional status associated with lower weight loss after bariatric surgery in older subjects. Obes Surg. 2019;29(11):3589–95.
Andreu A, Moizé V, Rodríguez L, et al. Protein intake, body composition, and protein status following bariatric surgery. Obes Surg. 2010;20(11):1509–15.
Armstrong T, Bull F. Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health. 2006;14(2):66–70.
Mohebi F, Mohajer B, Yoosefi M, et al. Physical activity profile of the Iranian population: STEPS survey, 2016. BMC Public Health. 2019;19(1):1266.
Wolz I, Hilker I, Granero R, et al. “Food addiction” in patients with eating disorders is associated with negative urgency and difficulties to focus on long-term goals. Front Psychol. 2016;7:61.
Pivarunas B, Conner BT. Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14.
Ozyurek P, Cogalan S. Mental and physical health-related quality of life and food addiction after obesity surgery: The first 2-year outputs. Perspectives in Psychiatric Care. 2020;57(2):565–572.
Shah M, Snell PG, Rao S, et al. High-volume exercise program in obese bariatric surgery patients: a randomized, controlled trial. Obesity. 2011;19(9):1826–34.
Tabesh MR, Maleklou F, Ejtehadi F, Alizadeh Z. Nutrition, physical activity, and prescription of supplements in pre-and post-bariatric surgery patients: a practical guideline. Obesity surgery. 2019;29(10):3385–3400.
Tettero OM, Aronson T, Wolf RJ, et al. Increase in physical activity after bariatric surgery demonstrates improvement in weight loss and cardiorespiratory fitness. Obes Surg. 2018;28(12):3950–7.
Shook RP, Hand GA, Drenowatz C, et al. Low levels of physical activity are associated with dysregulation of energy intake and fat mass gain over 1 year. Am J Clin Nutr. 2015;102(6):1332–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5, 5th ed. American Psychiatric Publishing, Inc.: Arlington, VA; 2013:1–992.
Vancampfort D, De Herdt A, Vanderlinden J, et al. Health related quality of life, physical fitness and physical activity participation in treatment-seeking obese persons with and without binge eating disorder. Psychiatry Res. 2014;216(1):97–102.
Roshanaei-Moghaddam B, Katon WJ, Russo J. The longitudinal effects of depression on physical activity. Gen Hosp Psychiatry. 2009;31(4):306–15.
Pedram P, Wadden D, Amini P, et al. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8(9):e74832.
Pursey KM, Gearhardt AN, Burrows TL. The relationship between “food addiction” and visceral adiposity in young females. Physiol Behav. 2016;157:9–12.
Nuijten MA, Monpellier VM, Eijsvogels TM, Janssen IM, Hazebroek EJ, Hopman MT. Rate and determinants of excessive fat-free mass loss after bariatric surgery. Obesity surgery. 2020;30(8):3119–3126.
Guida B, Cataldi M, Busetto L, et al. Predictors of fat-free mass loss 1 year after laparoscopic sleeve gastrectomy. J Endocrinol Investig. 2018;41(11):1307–15.
Faria SL, Kelly E, Faria OP. Energy expenditure and weight regain in patients submitted to Roux-en-Y gastric bypass. Obes Surg. 2009;19(7):856–9.
Rodríguez-Rivera C, Pérez-García C, Muñoz-Rodríguez JR, et al. Proteomic identification of biomarkers associated with eating control and bariatric surgery outcomes in patients with morbid obesity. World J Surg. 2019;43(3):744–50.
Friedrich N, Rosskopf D, Brabant G, et al. Associations of anthropometric parameters with serum TSH, prolactin, IGF-I, and testosterone levels: results of the study of health in Pomerania (SHIP). Exp Clin Endocrinol Diabetes. 2010;118(04):266–73.
Elera-Fitzcarrald C, Ugarte-Gil M, Gamboa-Cardenas R, et al. Prolactin levels are associated with a pro-inflammatory body mass distribution among women with systemic lupus erythematosus. Lupus. 2017;26(8):808–14.
Greenman Y, Tordjman K, Stern N. Increased body weight associated with prolactin secreting pituitary adenomas: weight loss with normalization of prolactin levels. Clin Endocrinol. 1998;48(5):547–53.
Oberbach A, Blüher M, Wirth H, et al. Combined proteomic and metabolomic profiling of serum reveals association of the complement system with obesity and identifies novel markers of body fat mass changes. J Proteome Res. 2011;10(10):4769–88.
Hauck C, Weiß A, Schulte EM, et al. Prevalence of ‘food addiction'as measured with the Yale Food Addiction Scale 2.0 in a representative German sample and its association with sex, age and weight categories. Obes Facts. 2017;10(1):12–24.
Borisenkov MF, Tserne TA, Bakutova LA. Food addiction in R ussian adolescents: a ssociations with age, sex, weight, and depression. Eur Eat Disord Rev. 2018;26(6):671–6.
Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Community Psychol. 2007;40(3-4):313–32.
Ross CE, Mirowsky J. Age and the balance of emotions. Soc Sci Med. 2008;66(12):2391–400.
Carpenter CL, Wong AM, Li Z, et al. Association of dopamine D2 receptor and leptin receptor genes with clinically severe obesity. Obesity. 2013;21(9):E467–E73.
Kim H-S, Kim S-Y. Validity of bioelectrical impedance analysis (BIA) in measurement of human body composition. Korean J Pediatr. 2005;48(7):696–700.
Funding
This research has been supported by Shahid Beheshti University of Medical Sciences (SBMU) and Health Services Grant (No: IR.SBMU.nnftri.Rec.1398.047). The authors would like to thank the nutrition clinics of two referral university hospitals: Sina Hospital-Tehran University of Medical Sciences and Shaheed Mostafa Khomeini hospital, Shahed University of Medical Sciences, and one private hospital, Ebnesina.
Author information
Authors and Affiliations
Contributions
MM, SRJ, MRT designed the research; MM, MRT, AK, MA performed the research; MM and HEZ analyzed the data; and MM wrote the manuscript. All authors critically revised the manuscript, agreed to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the Shahid Beheshti University of Medical Sciences (SBMU) and Health Services Grant (No: IR.SBMU.nnftri.Rec.1398.047) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mousavi, M., Tabesh, M.R., Khalaj, A. et al. Food Addiction Disorder 2 Years After Sleeve Gastrectomy; Association with Physical Activity, Body Composition, and Weight Loss Outcomes. OBES SURG 31, 3444–3452 (2021). https://doi.org/10.1007/s11695-021-05420-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05420-y