Abstract
Purpose
This study aimed to assess bariatric surgery (BS) effect on fall risk factors.
Materials and methods
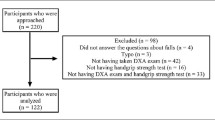
Fifteen patients undergoing BS (intervention group, IG) and 10 non-surgical obese patients (control group, CG) were recruited. IG was assessed at pre-surgery and 6 months after BS, while CG was assessed at baseline and reassessed after 6 months. At both time-points, anthropometry, lower limbs muscle strength (isokinetic dynamometer), balance in bipedal stance (force platform), daily physical activity (accelerometry), and health-related quality of life (SF-36 questionnaire) were assessed.
Results
At baseline, there were no differences between CG and IG for all parameters analyzed. Compared to CG, 6 months post-BS, the IG decreased weight, body mass index, waist and hip circumference. Balance showed limited improvements, with gains observed only on antero-posterior and total center of pressure velocity. Muscle strength displayed a divergent evolution 6 months after BS, with a decrease in absolute strength but an increase in relative strength. Although BS did not induce significant changes in time spent in different physical activity intensities, it decreased time in sedentary behavior and increased number of daily steps. Post-BS patients reported substantial improvements in quality-of-life, especially in physical function.
Conclusion
Patients seem to overestimate their actual physical fitness improvements attained after BS, which combined with increases in physical activity, might increase the likelihood of engaging in risky daily tasks to what they are physically not prepared to, consequently increasing fall risk.
Graphical abstract




Similar content being viewed by others
References
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. Jama. 2014;312(9):934–42.
Zhang Q, Chen Y, Li J, et al. A meta-analysis of the effects of bariatric surgery on fracture risk. Obes Rev. 2018;19(5):728–36.
Carlsson LMS, Sjoholm K, Ahlin S, et al. Long-term incidence of serious fall-related injuries after bariatric surgery in Swedish obese subjects. Int J Obes. 2019;43(4):933–7.
Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–9.
Herring LY, Stevinson C, Davies MJ, et al. Changes in physical activity behaviour and physical function after bariatric surgery: a systematic review and meta-analysis. Obes Rev. 2016;17(3):250–61.
Neunhaeuserer D, Gasperetti A, Savalla F, et al. Functional evaluation in obese patients before and after sleeve gastrectomy. Obes Surg. 2017;27(12):3230–9.
Kelley GA, Kelley KS, Kohrt WM. Exercise and bone mineral density in premenopausal women: a meta-analysis of randomized controlled trials. Int J Endocrinol. 2013;2013:741639.
Orwoll ES, Fino NF, Gill TM, et al. The relationships between physical performance, activity levels, and falls in older men. J Gerontol A Biol Sci Med Sci. 2019;74(9):1475–83.
Butler AA, Lord SR, Taylor JL, et al. Ability versus hazard: risk-taking and falls in older people. J Gerontol A Biol Sci Med Sci. 2015;70(5):628–34.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–72.
World Health Organisation. Waist Circumference and Wais-hip Ratio: Report of a WHO Expert consultation, Geneva, 8-11 December 2008, World Health Organization. 2011. 2020. https://www.who.int/nutrition/publications/obesity/WHO_report_waistcircumference_and_waisthip_ratio/en/. Accessed. Geneva 2008.
Duarte M, Freitas SM. Revision of posturography based on force plate for balance evaluation. Rev Bras Fis. 2010;14(3):183–92.
Aguilar-Farias N, Brown WJ, Peeters GM. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J Sci Med Sport. 2014;17(3):293–9.
Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. J Sci Med Sport. 2011;14(5):411–6.
Ferreira PL. Development of the Portuguese version of MOS SF-36. Part I. Cultural and linguistic adaptation. Acta Medica Port. 2000;13(1-2):55–66.
Ferreira PL. Development of the Portuguese version of MOS SF-36. Part II — Validation tests. Acta Medica Port. 2000;13(3):119–27.
Coulman KD, Abdelrahman T, Owen-Smith A, et al. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14(9):707–20.
Ferreira PL, Ferreira LN, Pereira LN. Physical and mental summary measures of health state for the Portuguese population. Rev Port Sau Pub. 2012;30:163–71.
Feys J. Nonparametric tests for the interaction in two-way factorial designs using R. The R Journal. 2016;8(1):367–78.
verasls. verasls/BaSEIB_BS_balance: How does bariatric surgery affect fall risk factors? (Version v1.0.0). Zenodo. 2020. https://doi.org/10.5281/zenodo.3840115.
Benetti FA, Bacha IL, Garrido Junior AB, et al. Analyses of balance and flexibility of obese patients undergoing bariatric surgery. Clinics (Sao Paulo). 2016;71(2):78–81.
Teasdale N, Hue O, Marcotte J, et al. Reducing weight increases postural stability in obese and morbid obese men. Int J Obes. 2007;31(1):153–60.
Maffiuletti NA, Jubeau M, Munzinger U, et al. Differences in quadriceps muscle strength and fatigue between lean and obese subjects. Eur J Appl Physiol. 2007;101(1):51–9.
Horlings CG, van Engelen BG, Allum JH, et al. A weak balance: the contribution of muscle weakness to postural instability and falls. Nat Clin Pract Neurol. 2008;4(9):504–15.
Adil MT, Jain V, Rashid F, et al. Meta-analysis of the effect of bariatric surgery on physical function. Br J Surg. 2018;105(9):1107–18.
Clemson L, Fiatarone Singh MA, Bundy A, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. Bmj. 2012;345:e4547.
Ellmers TJ, Paraskevopoulos IT, Williams AM, et al. Recalibrating disparities in perceived and actual balance abilities in older adults: a mixed-methods evaluation of a novel exergaming intervention. J Neuroeng Rehabil. 2018;15(1):26.
Acknowledgements
The authors would like to thank the participants who took part in this research and all that have collaborated in the project.
Funding
This study was funded by the Foundation for Science and Technology of Portugal (FCT) (grant PTDC/DTP-DES/0968/2014) and by the European Regional Development Fund (ERDF) through the Operational Competitiveness Programme (COMPETE) (grant POCI-01-0145-FEDER-016707). Florêncio Diniz-Sousa was supported by the FCT (grant SFRH/BD/117622/2016), Giorjines Boppre was supported by the FCT (grant SFRH/BD/146976/2019) and Lucas Veras was supported by the FCT (grant UI/BD/150673/2020). The study was developed in the Research Centre in Physical Activity, Health and Leisure (CIAFEL) funded by ERDF through the COMPETE and by the FCT (grant UIDB/00617/2020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Diniz-Sousa, F., Veras, L., Boppre, G. et al. How Does Bariatric Surgery Affect Fall Risk Factors?. OBES SURG 31, 3506–3513 (2021). https://doi.org/10.1007/s11695-021-05400-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05400-2