Abstract
Background
With advances in disease-specific treatments and improved overall survival, obesity rates are rising among patients with sickle cell disease (SCD). The primary aim of this study was to evaluate the role of bariatric surgery on clinical outcomes among hospitalized obese patients with SCD.
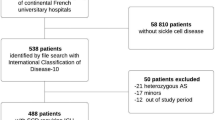
Methods
The United States Nationwide Inpatient Sample database was queried between 2004 and 2014 for discharges with co-diagnoses of morbid obesity and SCD. The primary outcome was in-hospital mortality. Secondary outcomes included vaso-occlusive crisis, acute chest syndrome, biliary-pancreatic complications, renal failure, urinary tract infection, malnutrition, sepsis, pneumonia, respiratory failure, thromboembolic events, strictures, wound infection, length of stay, and hospitalization costs. Using Poisson regression, adjusted incidence risk ratios (IRR) were derived for clinical outcomes in patients with prior-bariatric surgery compared to those without bariatric surgery.
Results
Among 2549 patients with a discharge diagnosis of SCD and morbid obesity, only 42 patients (1.7%) had bariatric surgery. On multivariable analysis, bariatric surgery did not influence mortality (P = 0.98). Bariatric surgery was not associated with increased risk for acute chest syndrome, sepsis, multi-organ failure, biliary-pancreatic, or surgery-related complications (all P > 0.05). Interestingly, bariatric surgery decreased risk of vaso-occlusive crises (IRR 0.21; 95% CI, 0.07–0.69; P = 0.01) in these patients and was associated with a shorter length of stay (P < 0.001) but higher hospitalization costs (P < 0.001).
Conclusions
Bariatric surgery may lower rates of vaso-occlusive crises in morbidly obese sickle cell patients without significantly affecting mortality and other adverse outcomes. In spite of this, these weight loss surgeries are underutilized in this select population.

Similar content being viewed by others
References
Sickle Cell Disease (SCD): Data and statistics. United States Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/sicklecell/data.html. Accessed March 31, 2018.
Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033–48.
Bain BJ. Sickle cell haemoglobin and its interactions with other variant haemoglobins and with thalassaemias. In: Haemoglobinopathy Diagnosis. 2nd ed. Oxford: Wiley-Blackwell; 2005.
Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38:S512–21.
Herrick JB. Peculiar elongated and sickle-shaped red blood corpuscles in a case of severe anemia. 1910. Yale J Biol Med. 2001;74:179–84.
Herrick JB. Peculiar elongated and sickle-shaped red blood corpuscles in a case of severe anemia. JAMA. 2014;312:1063.
Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–44.
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376:2018–31.
Hargrave DR, Wade A, Evans JP, et al. Nocturnal oxygen saturation and painful sickle cell crises in children. Blood. 2003;101:846–8.
Mitchell MJ, Carpenter GJ, Crosby LE, et al. Growth status in children and adolescents with sickle cell disease. Pediatr Hematol Oncol. 2009;26:202–15.
Modebe O, Ifenu SA. Growth retardation in homozygous sickle cell disease: role of calorie intake and possible gender-related differences. Am J Hematol. 1993;44:149–54.
Platt OS, Rosenstock W, Espeland MA. Influence of sickle hemoglobinopathies on growth and development. N Engl J Med. 1984;311:7–12.
Odonkor PO, Addae SK, et al. Basal metabolic rate and serum thyroid hormone levels in adolescent sickle cell patients. IRSC Med Sci. 1982;10:891.
Hyacinth HI, Adekeye OA, Yilgwan CS. Malnutrition in sickle cell Anemia: implications for infection, growth, and Maturation J Soc Behav Health Sci 2013;7.
Zivot A, Apollonsky N, Gracely E, et al. Body mass index and the association with vaso-occlusive crises in pediatric sickle cell disease. J Pediatr Hematol Oncol. 2017;39:314–7.
Hibbert JM, Hsu LL, Bhathena SJ, et al. Proinflammatory cytokines and the hypermetabolism of children with sickle cell disease. Exp Biol Med (Maywood). 2005;230:68–74.
Yanni E, Grosse SD, Yang Q, et al. Trends in pediatric sickle cell disease-related mortality in the United States, 1983-2002. J Pediatr. 2009;154:541–5.
Le PQ, Gulbis B, Dedeken L, et al. Survival among children and adults with sickle cell disease in Belgium: benefit from hydroxyurea treatment. Pediatr Blood Cancer. 2015;62:1956–61.
Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med. 2017;376:1561–73.
Gardner K, Douiri A, Drasar E, et al. Survival in adults with sickle cell disease in a high-income setting. Blood. 2016;128:1436–8.
Ashley-Koch A, Yang Q, Olney RS. Sickle hemoglobin (HbS) allele and sickle cell disease: a HuGE review. Am J Epidemiol. 2000;151:839–45.
Farooqui MW, Hussain N, et al. Prevalence of obesity in sickle cell patients. Blood, 2014:124(21), 4932. Retrieved from http://www.bloodjournal.org/content/124/21/4932. Accessed March 31, 2018. .
Ballas SK. The sixth vital sign: body mass index in patients with sickle cell disease. J Clin Med Res. 2017;9:889–90.
Chawla A, Sprinz PG, Welch J, et al. Weight status of children with sickle cell disease. Pediatrics. 2013;131:e1168–73.
Woods KF, Ramsey LT, Callahan LA, et al. Body composition in women with sickle cell disease. Ethn Dis. 2001;11:30–5.
Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality (AHRQ): advancing excellence in health care. https://www.ahrq.gov/research/data/hcup/index.html. Accessed January 6, 2018.
Okam MM, Shaykevich S, Ebert BL, et al. National trends in hospitalizations for sickle cell disease in the United States following the FDA approval of hydroxyurea, 1998-2008. Med Care. 2014;52:612–8.
McCarty TR, Echouffo-Tcheugui JB, Lange A, et al. Impact of bariatric surgery on outcomes of patients with nonalcoholic fatty liver disease: a nationwide inpatient sample analysis, 2004-2012. Surg Obes Relat Dis. 2018;14:74–80.
Sharma P, McCarty TR, Njei B. Impact of bariatric surgery on outcomes of patients with inflammatory bowel disease: a Nationwide inpatient sample analysis, 2004-2014. Obes Surg. 2017;
Population Estimates. United States Census Bureau. https://www.census.gov/popest/data/intercensal/national/nat2010.html. Accessed March 31, 2018.
Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. National vital statistics report: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 1998;47:1–16, 20.
Pells JJ, Presnell KE, Edwards CL, et al. Moderate chronic pain, weight and dietary intake in African-American adult patients with sickle cell disease. J Natl Med Assoc. 2005;97:1622–9.
Hackney AC, Hezier W, Gulledge TP, et al. Effects of hydroxyurea administration on the body weight, body composition and exercise performance of patients with sickle-cell anaemia. Clin Sci (Lond). 1997;92:481–6.
Santanelli J, Zempsky W, et al. (228) Obesity worsens pain impact in individuals with sickle cell disease. J Pain. 2014;15(4):S33.
Tauman R, Gozal D. Obesity and obstructive sleep apnea in children. Paediatr Respir Rev. 2006;7:247–59.
Narang I, McCrindle BW, Manlhiot C, et al. Intermittent nocturnal hypoxia and metabolic risk in obese adolescents with obstructive sleep apnea. Sleep Breath. 2018;22:1037–44.
Colquitt JL, Picot J, Loveman E, et al. Surgery for obesity. Cochrane Database Syst Rev. 2009:CD003641.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Buck J, Davies SC. Surgery in sickle cell disease. Hematol Oncol Clin North Am. 2005;19:897–902. vii
Neumayr L, Koshy M, Haberkern C, et al. Surgery in patients with hemoglobin SC disease. Preoperative transfusion in sickle cell disease study group. Am J Hematol. 1998;57:101–8.
Klebanoff MJ, Chhatwal J, Nudel JD, et al. Cost-effectiveness of bariatric surgery in adolescents with obesity. JAMA Surg. 2017;152:136–41.
Panca M, Viner RM, White B, et al. Cost-effectiveness of bariatric surgery in adolescents with severe obesity in the UK. Clin Obes. 2018;8:105–13.
Financial Support
This study was supported by NIH 5 T32 DK 7356-37 (BN).
This article has not been published and is not under consideration elsewhere.
Author information
Authors and Affiliations
Contributions
Study concept and design—Sharma P, McCarty TR, and Njei B. Paper preparation—Sharma P and McCarty TR. Statistical analysis—Njei B. Critical revisions—McCarty TR, Yadav S, Ngu JN, and Njei B. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent Statement
Informed consent statement does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prabin Sharma and Thomas R. McCarty are co-first authors
Electronic Supplementary Material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Sharma, P., McCarty, T.R., Yadav, S. et al. Impact of Bariatric Surgery on Outcomes of Patients with Sickle Cell Disease: a Nationwide Inpatient Sample Analysis, 2004–2014. OBES SURG 29, 1789–1796 (2019). https://doi.org/10.1007/s11695-019-03780-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03780-0