Abstract
Background
Bariatric surgery patients who report physical or sexual abuse form a sizeable cohort that stands out due to psychological comorbidity. Their possible vulnerability to suboptimal weight loss remains of interest. Their risk for malnutrition due to inadequate oral intake following surgery is underexplored.
Objectives
Study aims were to determine the effect of self-reported physical or sexual abuse in patients undergoing open biliopancreatic diversion with duodenal switch (BPD/DS) on (a) 3-year weight loss trajectories and (b) timing of feeding jejunostomy tube (J tube) removal. Delayed J tube removal served as an indicator for inadequate oral intake.
Methods
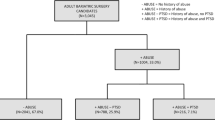
In this retrospective cohort study, the sample (N = 189) consisted of all patients who underwent primary BPD/DS by the same surgeon during 2009 and 2010 at a Midwestern health system. All patients had a J tube placed during surgery. Longitudinal mixed models were used for testing differences in weight loss trajectories by abuse status.
Results
There were no significant differences in weight loss trajectories by abuse status. The abused group had the J tube in place a mean of 61.9 days (SD = 39.5) compared to 44.8 days (SD = 32.8) for the not abused group, a significant difference.
Conclusions
Our use of the best available statistical methods lends validity to previous findings that suggest physical or sexual abuse does not affect weight loss after bariatric surgery. Increased likelihood of persistent inadequate oral intake in the abused group suggests the need for early multidisciplinary interventions that include mental health and nutrition experts.


Similar content being viewed by others
References
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Colquitt JL, Picot J, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641.
Hatoum IJ, Blackstone R, Hunter TD, et al. Clinical factors associated with remission of obesity-related comorbidities after bariatric surgery. JAMA Surg. 2016;151(2):130–7.
Wood GC, Benotti PN, Lee CJ, et al. Evaluation of the association between preoperative clinical factors and long-term weight loss after Roux-en-Y gastric bypass. JAMA Surg. 2016;151(11):1056–62.
Bessler M, Daud A, DiGiorgi MF, et al. Frequency distribution of weight loss percentage after gastric bypass and adjustable gastric banding. Surg Obes Relat Dis. 2008;4(4):486–91.
Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA Surg. 2017; https://doi.org/10.1001/jamasurg.2017.5025.
Stein J, Stier C, Raab H, et al. Review article: the nutritional and pharmacological consequences of obesity surgery. Aliment Pharmacol Ther. 2014;40(6):582–609.
Thibault R, Pichard C. Overview on nutritional issues in bariatric surgery. Curr Opin Clin Nutr Metab Care. 2016;19(6):484–90.
Alvarez J, Pavao J, Baumrind N, et al. The relationship between child abuse and adult obesity among California women. Am J Prev Med. 2007;33(1):28–33.
Bosch J, Weaver TL, Arnold LD, et al. The impact of intimate partner violence on women's physical health: findings from the Missouri behavioral risk factor surveillance system. J Interpers Violence. 2017;32(22):3402–19.
Gustafson TB, Sarwer DB. Childhood sexual abuse and obesity. Obes Rev. 2004;5(3):129–35.
Noll JG, Zeller MH, Trickett PK, et al. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics. 2007;120(1):e61–7.
Williamson DF, Thompson TJ, Anda RF, et al. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26(8):1075–82.
Caslini M, Bartoli F, Crocamo C, et al. Disentangling the association between child abuse and eating disorders: a systematic review and meta-analysis. Psychosom Med. 2016;78(1):79–90.
Fergusson DM, Horwood LJ, Ridder EM. Partner violence and mental health outcomes in a New Zealand birth cohort. J Marriage Fam. 2005;67(5):1103–19.
Fergusson DM, McLeod GFH, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30-year longitudinal study in New Zealand. Child Abuse Negl. 2013;37(9):664–74.
Lindert J, von Ehrenstein OS, Grashow R, et al. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. 2014;59(2):359–72.
Blaine B. Does depression cause obesity?: a meta-analysis of longitudinal studies of depression and weight control. Health Psychol. 2008;13(8):1190–7.
Brumpton B, Langhammer A, Romundstad P, et al. The associations of anxiety and depression symptoms with weight change and incident obesity: the HUNT study. Int J Obes. 2013;37(9):1268–74.
Marek RJ, Ben-Porath YS, Heinberg LJ. Understanding the role of psychopathology in bariatric surgery outcomes. Obes Rev. 2016;17(2):126–41.
Striegel-Moore RH, Cachelin FM, Dohm F, et al. Comparison of binge eating disorder and bulimia nervosa in a community sample. Int J Eat Disord. 2001;29(2):157–65.
Sarwer DB, Cohn NI, Gibbons LM, et al. Psychiatric diagnoses and psychiatric treatment among bariatric surgery candidates. Obes Surg. 2004;14(9):1148–56.
Imperatori C, Innamorati M, Lamis DA, et al. Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl. 2016;58:180–90.
Ramirez JC, Milan S. Childhood sexual abuse moderates the relationship between obesity and mental health in low-income women. Child Maltreat. 2016;21(1):85–9.
Salwen JK, Hymowitz GF, Vivian D, et al. Childhood abuse, adult interpersonal abuse, and depression in individuals with extreme obesity. Child Abuse Negl. 2014;38(3):425–33.
Steinig J, Wagner B, Shang E, et al. Sexual abuse in bariatric surgery candidates—impact on weight loss after surgery: a systematic review. Obes Rev. 2012;13(10):892–901.
Hulme PA, McBride CL, Kupzyk KA, et al. Pilot study on childhood sexual abuse, diurnal cortisol secretion, and weight loss in bariatric surgery patients. J Child Sex Abus. 2015;24(4):385–400.
Buser A, Dymek-Valentine M, Hilburger J, et al. Outcome following gastric bypass surgery: impact of past sexual abuse. Obes Surg. 2004;14(2):170–4.
Buser AT, Lam CS, Poplawski SC. A long-term cross-sectional study on gastric bypass surgery: impact of self-reported past sexual abuse. Obes Surg. 2009;19(4):422–6.
Clark MM, Hanna BK, Mai JL, et al. Sexual abuse survivors and psychiatric hospitalization after bariatric surgery. Obes Surg. 2007;17(4):465–9.
Fujioka K, Yan E, Wang HJ, et al. Evaluating preoperative weight loss, binge eating disorder, and sexual abuse history on Roux-en-Y gastric bypass outcome. Surg Obes Relat Dis. 2008;4(2):137–43.
Grilo CM, White MA, Masheb RM, et al. Relation of childhood sexual abuse and other forms of maltreatment to 12-month postoperative outcomes in extremely obese gastric bypass patients. Obes Surg. 2006;16(4):454–60.
Larsen JK, Geenen R. Childhood sexual abuse is not associated with a poor outcome after gastric banding for severe obesity. Obes Surg. 2005;15(4):534–7.
Oppong BA, Nickels MW, Sax HC. The impact of a history of sexual abuse on weight loss in gastric bypass patients. Psychosomatics. 2006;47(2):108–11.
Ray EC, Nickels MW, Sayeed S, et al. Predicting success after gastric bypass: the role of psychosocial and behavioral factors. Surgery. 2003;134(4):555–63.
Hensel JM, Grosman Kaplan K, Anvari M, et al. The impact of history of exposure to abuse on outcomes after bariatric surgery: data from the Ontario Bariatric Registry. Surg Obes Relat Dis. 2016;12(8):1441–6.
Lodhia N, Rosas U, Moore M, et al. Do adverse childhood experiences affect surgical weight loss outcomes? J Gastrointest Surg. 2015;19(6):993–8.
Wedin S, Madan A, Correll J, et al. Emotional eating, marital status and history of physical abuse predict 2-year weight loss in weight loss surgery patients. Eat Behav. 2014;15(4):619–24.
McVay MA, Friedman KE, Applegate KL, et al. Patient predictors of follow-up care attendance in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis. 2013;9(6):956–62.
Rusch MD, Andris D, Wallace JR. Reasons for failed weight loss surgery. Clin Nutr Insight. 2009;35(1):1–4.
Thibault R, Huber O, Azagury DE, et al. Twelve key nutritional issues in bariatric surgery. Clin Nutr. 2016;35(1):12–7.
Heber D, Greenway FL, Kaplan LM, et al. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010;95(11):4823–43.
Keshishian A, Zahriya K, Hartoonian T, et al. Duodenal switch is a safe operation for patients who have failed other bariatric operations. Obes Surg. 2004;14(9):1187–92.
Anthone GJ, Lord RV, DeMeester TR, et al. The duodenal switch operation for the treatment of morbid obesity. Ann Surg. 2003;238(4):618–27.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Dawes AJ, Maggard-Gibbons M, Maher AR, et al. Mental health conditions among patients seeking and undergoing bariatric surgery: a meta-analysis. JAMA. 2016;315(2):150–63.
Ashton D, Favretti F, Segato G. Preoperative psychological testing—another form of prejudice. Obes Surg. 2008;18(10):1330–7.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89.
Strain GW, Torghabeh MH, Gagner M, et al. Nutrient status 9 years after biliopancreatic diversion with duodenal switch (BPD/DS): an observational study. Obes Surg. 2017;27(7):1709–18.
Godoy CM, Caetano AL, Viana KR, et al. Food tolerance in patients submitted to gastric bypass: the importance of using an integrated and interdisciplinary approach. Obes Surg. 2012;22(1):124–30.
Suter M, Calmes JM, Paroz A, et al. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17(1):2–8.
Higa KD, Himpens J. The reality of long-term follow-up of bariatric/metabolic surgery patients—a conundrum. JAMA Surg. 2017; https://doi.org/10.1001/jamasurg.2017.5010.
Saczynski JS, McManus DD, Goldberg RJ. Commonly used data-collection approaches in clinical research. Am J Med. 2013;126(11):946–50.
Stefaniak T, Babinska D, Trus M, et al. The impact of history of sexual abuse on weight loss in gastric bypass patients. Psychosomatics. 2007;48(3):270–1.
Acknowledgements
The authors would like to thank clinic managers Christine Heavey and Lorrie Dohn for their assistance with this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
For this retrospective study, informed consent was not obtained from participants. Please see the Statement of Human and Animal Rights section for more information.
Ethics Statement
This original manuscript has not been submitted elsewhere. The manuscript has not been published previously, in part or in full. Each of the authors contributed to maintaining the integrity of the study and this report. The first author provided consistent oversight of the work. The surgeon whose patients were used for this research played no role in data collection. No data were fabricated or manipulated. Consent to submit the manuscript was obtained from all authors of the work, as well as the institute where the study took place.
Statement of Human/Animal Rights
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Permission was obtained for the study from the Institutional Review Boards of (a) the university at which the first author was affiliated at the time, and (b) the health system at which the study took place. The university classified the study as Expedited Category of Review: 45CFR46.110; 21CFR56.110, Category 5. For this type of study, formal consent is not required. All authors were CITI certified.
Rights and permissions
About this article
Cite this article
Hulme, P.A., Kupzyk, K.A., Anthone, G.J. et al. Weight Loss and Timing of J Tube Removal in Biliopancreatic Diversion with Duodenal Switch Patients Who Report Physical or Sexual Abuse. OBES SURG 28, 2361–2367 (2018). https://doi.org/10.1007/s11695-018-3166-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3166-3