Abstract
Importance
Inappropriate antibiotic use for upper respiratory tract infections (URTIs) is an ongoing problem in primary care. There is extreme variation in the prescribing practices of individual physicians, which cannot be explained by clinical factors.
Objective
To identify factors associated with high and low prescriber status for management of URTIs in primary care practice.
Design and Participants
Exploratory sequential mixed-methods design including interviews with primary care physicians in a large health system followed by a survey. Twenty-nine physicians participated in the qualitative interviews. Interviews were followed by a survey in which 109 physicians participated.
Main Measures
Qualitative interviews were used to obtain perspectives of high and low prescribers on factors that influenced their decision making in the management of URTIs. A quantitative survey was created based on qualitative interviews and responses compared to actual prescribing rates. An assessment of self-prescribing pattern relative to their peers was also conducted.
Results
Qualitative interviews identified themes such as clinical factors (patient characteristics, symptom duration, and severity), nonclinical factors (physician-patient relationship, concern for patient satisfaction, preference and expectation, time pressure), desire to follow evidence-based medicine, and concern for adverse effects to influence prescribing. In the survey, reported concern regarding antibiotic side effects and the desire to practice evidence-based medicine were associated with lower prescribing rates whereas reported concern for patient satisfaction and patient demand were associated with high prescribing rates. High prescribers were generally unaware of their high prescribing status.
Conclusions and Relevance
Physicians report that nonclinical factors frequently influence their decision to prescribe antibiotics for URTI. Physician concerns regarding antibiotic side effects and patient satisfaction are important factors in the decision-making process. Changes in the health system addressing both physicians and patients may be necessary to attain desired prescribing levels.
Similar content being viewed by others
INTRODUCTION
Upper respiratory tract infections (URTIs) are the most common reason adults receive antibiotics.1,2 However, most URTIs are viral in nature, and at least 30% of the antibiotics prescribed to treat them are inappropriate and may lead to preventable harm from side effects.3 Inappropriate antibiotics contribute to antibiotic resistance,4 increase medical costs, and reduce the effectiveness of medical care for bacterial infections.5
Despite widespread efforts to decrease inappropriate antibiotic prescribing, including evidence-based guidelines for appropriate use of antibiotics, prescribing rates have remained high.2 Interventions to reduce inappropriate antibiotic prescribing have been multifaceted, including educating patients, auditing physicians’ prescriptions and providing feedback, and offering clinician’s financial incentives.6 Unfortunately these interventions are not uniformly successful at reducing inappropriate antibiotic prescribing.7,8,9
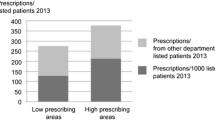
One potential solution is to focus on high prescribers, because a large proportion of antibiotics are prescribed by a minority of clinicians. In one study, antibiotic prescribing rates for URTIs at Veterans Affairs facilities ranged from 14 to 88%,10 and the top 10% of prescribers prescribed to 95% of patients with URTIs.11 Similarly, at a large academic center, individual antibiotic prescribing rates ranged from 0 to 100%, with 12% of clinicians responsible for 41% of antibiotic prescriptions.12 Despite this finding, little is known about differences in attitudes and beliefs between high and low prescribers. A deeper understanding of the beliefs and attitudes of the minority of high prescribers, who may be resistant to current efforts to reduce inappropriate prescribing, could be used to develop targeted interventions. Thus, the objective of this sequential mixed-methods study was to identify and confirm themes associated with high rates of antibiotic prescription.
METHODS
We undertook a single-center, exploratory sequential, mixed-methods study to evaluate the factors that high and low prescribers consider when deciding whether to prescribe an antibiotic for an upper respiratory tract infection in primary care.13 The Cleveland Clinic is a large nonprofit academic health system with 36 primary care practices in Northeast Ohio. Annually, approximately 600,000 patients are seen in primary care. Internal medicine and family medicine physicians from 16 practice sites were invited to participate. First, semi-structured qualitative interviews with physicians were used to identify themes associated with antibiotic prescribing. Second, themes from the interviews were used to create a survey deployed to full-time primary care physicians. Third, using electronic health record (EHR) data, contemporaneous antibiotic prescribing rates for clinicians with at least 20 URTI visits were linked to survey responses, enabling us to identify the beliefs and attitudes that were associated with higher or lower prescribing rates. The Cleveland Clinic Institutional Review Board approved this study.
Qualitative Study
Interview Participants
We sampled physicians based on their antibiotic prescribing rates that were determined from a previous study.12 All physicians who had prescribed antibiotics at a rate that was statistically higher or lower than the average (p value < 0.05) across all primary care physicians were eligible to participate, which allowed for comparisons between high and low prescribers. Interviews were conducted between August 2015 and April 2016. Recruitment was conducted via e-mail. The e-mail did not identify the physician as a high or low prescriber and the recruiter was blinded as to the prescriber’s status.
Qualitative Data Collection
A semi-structured interview guide was developed and pilot tested. The interview questions focused on domains relevant to clinical practice (see Appendix). Questions relating to clinical factors that might influence antibiotic prescribing were based on existing guidelines for antibiotics.2,14 Based on prior studies,15,16,17 we included questions that addressed nonclinical factors such as patients requesting antibiotics, concern for patient satisfaction, and time pressure. We also included questions probing self-reflection of prescribing patterns relative to their peers because interventions that provide physician with audit and feedback6 have been shown to decrease inappropriate prescribing. Verbal informed consent was obtained from all participants. Interviews lasted approximately 30 min and were conducted via phone or in person, and all interviews were audio recorded. The interviewers (A.C. and A.P.) were blinded as to the physician’s prescriber status at the time of the interview. There was no incentive for participation. Audio data was transcribed verbatim prior to analysis.
Qualitative Analysis
Using an inductive qualitative content analysis approach, two physicians (A.M.H. and A.P.) concurrently analyzed 5 transcripts adding descriptive codes. After the preliminary code list was developed, A.P. analyzed the remainder of the transcripts and assigned codes. Codes were then sorted into pertinent themes. Any discrepancies in coding were resolved through discussion until a consensus was reached. After completing an initial analysis, the researchers were unblinded to prescriber status. All the transcripts were re-analyzed to look for variation in themes factoring in the prescriber status.
Quantitative Study
Survey Data
Using the findings from the qualitative interviews and previously published surveys,15,16,17 we created an online survey (see Appendix). The survey included questions about the importance of patient satisfaction, complications, side effects, patient trust, patient insistence, and feeling rushed; response options ranged on a 4-point scale from “not important” to “extremely important.” Standard demographic information was also collected. The survey was pilot tested on a convenience sample of resident physicians at Cleveland Clinic for face validity and clarity, and the questions were iteratively refined. We then surveyed all internal medicine and family medicine physicians at the 16 practice sites. The survey was sent out electronically three times during the 1st quarter of 2017 at 1-week intervals. No incentive was offered for participation. Based on our qualitative interviews, we hypothesized that the following factors would be associated with higher prescribing rates: duration and severity of symptoms, color of sputum, concern for patient satisfaction, time pressure, and the desire to meet patient expectations and address patient convenience. We hypothesized the remaining factors (e.g., concern about antibiotic side effects and the desire to practice evidence-based medicine) would be associated with lower prescribing rates.
Antibiotic Prescribing Data
We collected contemporaneous antibiotic prescribing data from our EHR for acute URTI visits that occurred between October 2016 and September 2017 (6 months on either side of the survey). Visits for acute URTI were identified based on ICD diagnosis codes for upper respiratory tract infection, rhinosinusitis, pharyngitis, sore throat, otalgia, otitis media, sinusitis, cough, and bronchitis. For the purpose of comparing rates of antibiotic prescribing, we combined all the respiratory tract infection diagnoses to avoid biases relating to individual coding patterns.12, 18 Patients with history of COPD, immunocompromised status, or current use of immunosuppressant medications, for whom antibiotics may be appropriate, were excluded.
Quantitative Data Analysis
Physicians’ survey responses were linked to their antibiotic prescribing rates. Based on the distribution of the survey results, survey responses were dichotomized into “not” or “somewhat” important versus “very” or “extremely” important. In order to maximize power, we kept prescribing rate as a continuous outcome and used Student’s t test to compare the mean rate for physicians who selected not/somewhat versus very/extremely important.19 A two-sided p value < 0.05 was considered significant. Because we had a priori hypotheses for each variable based on our qualitative interviews, we did not adjust for multiple comparisons.
We calculated each physician’s prescribing rate and their standard deviation to determine the 95% confidence intervals. To assess the accuracy of physicians’ self-perceptions, physicians were grouped into low, average, and high prescribers. We did this by comparing each physician’s prescribing rate to the overall mean, using the 95% confidence interval around the physician’s rate. Those that did not overlap the mean were considered higher or lower, while those that did overlap were considered average. Based on their response to the question “Do you believe you prescribe antibiotics more, less or about the same as your colleagues” and their prescribing status (i.e., low, average, or high), physicians’ perceptions were classified as “accurate” or “inaccurate.” We then compared the proportion of accurate perceptions by prescribing level using Fisher’s exact test. All quantitative analysis was conducted using Stata 14.0.
RESULTS
Qualitative Results
Twenty-nine physicians from 16 practice sites agreed to participate in the qualitative interviews, including 9 high prescribers and 20 low prescribers. Major themes that emerged included clinical factors (e.g., patient characteristics, symptom duration, and severity), nonclinical factors (e.g., physician-patient relationship, concern for patient satisfaction, patient expectations and preferences, and time pressure), desire to follow evidence-based medicine, clinician perception of adverse effects, and self-reflection on peer comparison (Table 1).
High and low prescribers often identified the same themes but approached them from different perspectives. For clinical factors such as patient characteristics, high prescribers’ decisions were based on a general impression of a patient “looking sick” whereas low prescribers focused on specific findings such as rales on exam. Both high and low prescribers considered their treatment choices to be evidence based. However, high prescribers discussed guidelines for pharyngitis and sinusitis, for which antibiotics are often appropriate, whereas low prescribers were more likely to state that the evidence is against prescribing antibiotics in general, and even more so, for bronchitis and viral URTI.
Regarding nonclinical factors, both high and low prescribers agreed that prescribing antibiotics improved patient satisfaction, but high prescribers stated that they allowed their desire to achieve high patient satisfaction scores to influence their actions, while low prescribers were willing to sacrifice patient satisfaction to provide what they saw as appropriate care. High prescribers cited patient demand as a reason for prescribing antibiotics. In contrast, low prescribers perceived that such demand was decreasing over the years. When asked “Do you prescribe antibiotics depending on how busy your clinic flow might be?” high prescribers noted that prescribing an antibiotic was easier and faster, whereas the majority of the low prescribers responded “No” or “Never” and elaborated on the importance of patient education.
In response to the question, “Do you believe you prescribe antibiotics more, less or same as your colleagues?,” the majority of low prescribers (75%) accurately identified themselves as prescribing less than their peers, whereas the majority of high prescribers (89%) failed to recognize that they were outliers. On further questioning as to “why they believe their prescribing patterns are high, low or similar to their peers,” the low prescribers appeared to be more aware of the practice of their peers.
Quantitative Results
In total, 109 of 222 physicians completed the survey and had enough antibiotic prescribing opportunities (response rate 49%). The majority identified their specialty as internal medicine (59% n = 64), practiced medicine more than 15 years (58%, n = 63), and were male (57%, n = 58) (Table 2). On average, physicians prescribed antibiotics 46% of the time. Based on their 95% CIs, 42% of physicians (n = 46) were low prescribers, 39% (n = 42) were average, and 19% (n = 21) were high prescribers (Fig. 1).
Antibiotic prescribing rate of physicians who responded to the survey (mean and 95% confidence interval). Dots represent 109 individual physicians. Those in red have rates significantly above, and those in green significantly below, the overall mean prescribing rate of 0.46. Physicians in blue are not significantly different from the mean.
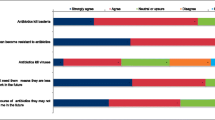
Associations between survey responses and prescribing rates appear in Table 3. All associations occurred in the hypothesized direction, but not all factors were significantly associated with prescribing rate. Nonclinical factors were strongly associated with prescribing. Concern for patient satisfaction and for patient requests for antibiotics was associated with a higher prescribing rate, whereas valuing the ability to educate patients was associated with a lower prescribing rate. Concern for clinical factors, such as severity or duration of symptoms, was associated with a higher prescribing rate, while concern about the antibiotic side effects and desire to practice evidence-based guidelines was associated with a lower prescribing rate. Based on the qualitative analyses, we expected factors such as time pressure and sputum color to be associated with a higher prescribing rate but this association was not statistically significant.
Physicians generally had limited knowledge of their performance relative to peers. Overall, 56% of physicians accurately identified themselves as low, medium, or high prescribers (Fig. 2). Low prescribers tended to have the most accurate self-assessment. Most high prescribers thought they were average, and 15% of high prescribers believed they were lower than their peers.
DISCUSSION
In this mixed-methods study of primary care physicians and their antibiotic prescribing for URTIs, we employed qualitative analysis to identify potential factors that might influence decision making, including clinical factors and nonclinical factors. Then, in a survey of more than a hundred practicing physicians, we found that only 2 clinical factors—reported duration and severity of symptoms—were associated with antibiotic prescribing rates (i.e., physicians who took these factors into account when prescribing had higher rates than those who did not consider them important). High prescribing rates were more strongly associated with reported nonclinical factors, such as patients asking for antibiotics and concern for patient satisfaction. Conversely, concern regarding antibiotic side effects and the desire to practice evidence-based medicine were associated with lower prescribing rates. Another important finding was that physicians who prescribe significantly more than average were generally unaware of their outlier status. In fact, 15% of these high prescribers believed they prescribed less than their peers.
Antibiotic prescribing for viral respiratory infections has remained an intractable problem in primary care. Recent studies11, 12 have demonstrated wide variation in antibiotic prescribing at the individual clinician level, allowing for the possibility of targeted interventions based on clinicians’ attitudes and beliefs. One comprehensive qualitative study20 found that, in general, physicians considered nonclinical factors such as patient expectations, patient preference, time pressure, and patient satisfaction in their treatment decisions. However, they did not assess the differences between high and low prescribers regarding these issues. Prior surveys,15,16,17 which were not based on qualitative interviews, also did not consider the prescribing rates of the respondents. One study of emergency physicians found that high prescribers tended to see antibiotic prescribing as an opportunity to shorten infection at no cost, whereas low prescribers appreciated the potential harms of antibiotics.21
We also found a number of ways that high and low prescribers differed in their approaches, thus informing potential interventions to address these discrepancies. Similar to the study in the ED, we found that low prescribers prioritized antibiotic side effects and the desire to practice evidence-based medicine. Antibiotics have well known short-term and long-term consequences, including rising antibiotic resistance and damage to the microbiome.22 Raising physician and patient awareness about these adverse effects might decrease demand from patients and prescribing by physicians.
At the same time, we found a number of ways in which the prescribing patterns for high and low prescribers did not differ. For example, the perceived importance of sputum color, patient age, and feeling rushed was not associated with mean antibiotic prescribing rate. Our finding concerning sputum color differed from the results of a multinational cohort, which suggested that having discolored sputum was associated with antibiotic prescriptions.23 The lack of association with time pressure is of particular note because one recent study confirmed some of our respondents’ belief that it takes longer not to prescribe an antibiotic than to prescribe one.24 The difference in time, however, was less than a minute, and in our survey, even for busy clinicians, this appears not to be an important issue.
More important was the idea that patients who receive antibiotics are more satisfied. Overall, studies in support of this concept are mixed.25, 26 In a recent study of 7747 telemedicine patients with URTIs, a prescription for an antibiotic was the strongest predictor of patient satisfaction, and no physician in the top decile of satisfaction scores prescribed antibiotics to less than 75% of patients.27 In our qualitative study, both high and low prescribers endorsed this belief, but the low prescribers were willing to forego patient satisfaction to practice evidence-based medicine, while high prescribers were not. Because physician reimbursement is often tied to patient satisfaction scores, interventions to overcome this bias may require broader education of patients about the importance of not taking antibiotics for viral infections or not counting satisfaction scores for URTI visits to relieve physicians of this pressure.
Another novel finding of our study was that physicians were often unaware of their outlier status. High prescribers were particularly unaware of how they compared to peers. Providing feedback to physicians on their antibiotic prescribing rate relative to their peers has been shown to reduce prescribing, although in the long term, physicians tend to revert to old habits if the intervention is not sustained.6 Because high prescribers are responsible for a majority of all prescriptions, targeting them may have the greatest impact.
Our study has some limitations. Our sample is from one health system and may not be representative of clinicians at large. Appropriateness of prescriptions was based on diagnosis codes, which were derived from retrospective data. Our study measured prescriptions, not fills, and so does not account for delayed prescribing strategies. For the qualitative portion, we had a higher proportion of low prescribers who agreed to participate in the study compared to high prescribers. Our survey response rate was 49%. Although this rate might be considered low for a representative sample, the purpose of our survey was to evaluate the association between prescribing rate and survey responses, not to provide a summary assessment of physician views on the matter. Because we collected data only for physicians who completed the survey, we could not compare respondents and nonrespondents on prescribing rates or other characteristics.
In this mixed-methods study of primary care physicians, we identified themes associated with high rates of antibiotic prescribing for URTIs. We found that concern about antibiotic side effects and the desire to practice evidence-based medicine were important determinants of low prescribing rates, whereas high prescribers reported more concern about patient satisfaction. To date, multiple systematic efforts to decrease antibiotic prescribing have targeted physicians, but our work suggests that in most cases, physician concern about patient desires is an important factor in the decision-making process. Changes in the health system addressing both physicians and patients may be necessary to attain desired prescribing levels.
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- COPD:
-
chronic obstructive pulmonary disease
- EHR:
-
electronic health record
- ICD:
-
International Classification of Diseases
- URTI:
-
upper respiratory tract infection
References
Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47(6):735–743. https://doi.org/10.1086/591126
Harris AM, Hicks LA, Qaseem A. Appropriate antibiotic use for acute respiratory tract infection in adults: Advice for high-value care from the American college of physicians and the centers for disease control and prevention. Ann Intern Med. 2016;164(6):425–434. https://doi.org/10.7326/M15-1840
Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among us ambulatory care visits, 2010-2011. JAMA - J Am Med Assoc. 2016;315(17):1864–1873. https://doi.org/10.1001/jama.2016.4151
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/. Accessed 26 Nov 2018.
Smith R, Coast J. The true cost of antimicrobial resistance. BMJ. 2013;346(mar11 3):f1493-f1493. https://doi.org/10.1136/bmj.f1493
Meeker D, Linder JA, Fox CR, et al. Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices. JAMA. 2016;315(6):562. https://doi.org/10.1001/jama.2016.0275
Van Der Velden AW, Pijpers EJ, Kuyvenhoven MM, Tonkin-Crine SKG, Little P, Verheij TJM. Effectiveness of physician-targeted interventions to improve antibiotic use for respiratory tract infections. Br J Gen Pract. 2012;62(605). https://doi.org/10.3399/bjgp12X659268
Arnold S, Straus S. Interventions to improve antibiotic prescribing practices in ambulatory care. Evidence-Based Child Heal A Cochrane Rev J. 2006. https://doi.org/10.1002/ebch.23
Hemkens LG, Saccilotto R, Reyes SL, et al. Personalized prescription feedback to reduce antibiotic overuse in primary care: Rationale and design of a nationwide pragmatic randomized trial. BMC Infect Dis. 2016;16(1). https://doi.org/10.1186/s12879-016-1739-0
Aspinall SL, Berlin JA, Zhang Y, Metlay JP. Facility-level variation in antibiotic prescriptions for veterans with upper respiratory infections. Clin Ther. 2005;27(2):258–262. https://doi.org/10.1016/j.clinthera.2005.02.002
Jones BE, Sauer B, Jones MM, et al. Variation in outpatient antibiotic prescribing for acute respiratory infections in the Veteran population a cross-sectional study. Ann Intern Med. 2015;163(2):73–80. https://doi.org/10.7326/M14-1933
Manne M, Deshpande A, Hu B, et al. Provider variation in antibiotic prescribing and outcomes of respiratory tract infections. South Med J. 2018. https://doi.org/10.14423/SMJ.0000000000000795
Cresswell JW. Qualitative, Quantitative. and Mixed Methods Approaches. In: Research Design, 2nd Ed, 2003. https://doi.org/10.3109/08941939.2012.723954.
Adult Treatment Recommendations | Community | Antibiotic Use | CDC. https://www.cdc.gov/antibiotic-use/community/for-hcp/outpatient-hcp/adult-treatment-rec.html. Accessed 24 October 2018.
Gidengil CA, Mehrotra A, Beach S, Setodji C, Hunter G, Linder JA. What Drives Variation in Antibiotic Prescribing for Acute Respiratory Infections? J Gen Intern Med. 2016. https://doi.org/10.1007/s11606-016-3643-0
López-Vázquez P, Vázquez-Lago JM, Gonzalez-Gonzalez C, et al. Development and validation of the knowledge and attitudes regarding antibiotics and resistance (KAAR-11) questionnaire for primary care physicians. J Antimicrob Chemother. 2016. https://doi.org/10.1093/jac/dkw238
Teixeira Rodrigues A, Ferreira M, Roque F, et al. Physicians’ attitudes and knowledge concerning antibiotic prescription and resistance: Questionnaire development and reliability. BMC Infect Dis. 2016. https://doi.org/10.1186/s12879-015-1332-y
Martinez KA, Rood M, Rothberg MB. Coding Bias in Respiratory Tract Infections May Obscure Inappropriate Antibiotic Use. J Gen Intern Med. 2019. https://doi.org/10.1007/s11606-018-4823-x
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006. https://doi.org/10.1136/bmj.332.7549.1080
Dempsey PP, Businger AC, Whaley LE, Gagne JJ, Linder JA. Primary care clinicians perceptions about antibiotic prescribing for acute bronchitis: A qualitative study. BMC Fam Pract. 2014. https://doi.org/10.1186/s12875-014-0194-5
Klein EY, Martinez EM, May L, Saheed M, Reyna V, Broniatowski DA. Categorical Risk Perception Drives Variability in Antibiotic Prescribing in the Emergency Department: A Mixed Methods Observational Study. J Gen Intern Med. 2017. https://doi.org/10.1007/s11606-017-4099-6
Blaser MJ. Antibiotic use and its consequences for the normal microbiome. Science (80-). 2016. https://doi.org/10.1126/science.aad9358
Butler CC, Kelly MJ, Hood K, et al. Antibiotic prescribing for discoloured sputum in acute cough/lower respiratory tract infection. Eur Respir J. 2011. https://doi.org/10.1183/09031936.00133910
Rood KA, Jhangiani N, Boissy A, Rothberg MB, M MN. Prescription of antibiotics in a primary care telemedicine service: Association with patient satisfaction and visit length. J Gen Intern Med. 2017.
Jerant A, Fenton JJ, Kravitz RL, et al. Association of clinician denial of patient requests with patient satisfaction. In: JAMA Internal Medicine. 2018. https://doi.org/10.1001/jamainternmed.2017.6611
Sharp AL, Shen E, Kanter MH, Berman LJ, Gould MK. Low-value antibiotic prescribing and clinical factors influencing patient satisfaction. Am J Manag Care. 2017.
Martinez KA, Rood M, Jhangiani N, Kou L, Boissy A, Rothberg MB. Association between Antibiotic Prescribing for Respiratory Tract Infections and Patient Satisfaction in Direct-to-Consumer Telemedicine. JAMA Intern Med. 2018. https://doi.org/10.1001/jamainternmed.2018.4318
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Misra-Hebert is supported by a career development award from the Agency for Healthcare Research and Quality (K08HS024128).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 46 kb)
Rights and permissions
About this article
Cite this article
Patel, A., Pfoh, E.R., Misra Hebert, A.D. et al. Attitudes of High Versus Low Antibiotic Prescribers in the Management of Upper Respiratory Tract Infections: a Mixed Methods Study. J GEN INTERN MED 35, 1182–1188 (2020). https://doi.org/10.1007/s11606-019-05433-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05433-5