Abstract
Background
Gastroesophageal reflux disease (GERD) is a common condition, resulting from the loss of the anti-reflux barrier. Laparoscopic fundoplication is the surgical procedure of choice for treatment of GERD; however, there remains a debate on the exact mechanism through which it prevents reflux.
Objectives
Our aim was to understand the relationship between reflux, fundoplication, and the angle of His on an experimental model.
Methods
The study was conducted on four groups of fresh explanted swine stomachs: control group, myotomy, myotomy with Nissen fundoplication, and myotomy with Toupet fundoplication. The stomachs were placed in a specially designated container on an inclinable platform which would increase the hydrostatic pressure on the esophago-gastric junction. Measurements of the angle of His using fluoroscopy and the esophago-gastric orifice area using endoscopy were performed, and the occurrence of reflux was documented.
Results
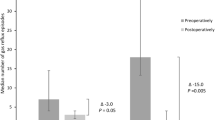
Each group of the study contained nine swine stomachs. In the control and myotomy groups, the angle became wider as the incline level increased the pressure and was significantly different between the groups (p < .001). Both groups demonstrated an increase in the orifice area as the incline level increased the pressure. There was a significant correlation between the angle of His and the area of the esophago-gastric orifice (p < .001). In the control group, the reflux began at the 0°. In the myotomy group, it began at the + 15° incline (less pressure). Reflux rarely occurred in the Nissen and Toupet groups, with the breaking point being mostly defined as “beyond − 30°”. A significant difference was noted in the occurrence of reflux between fundoplication and the non-fundoplication groups (p < 0.001), while there was no significant difference between the Toupet and Nissen groups (p = 0.134). Analysis showed a significant independent correlation between both the angle of His and the orifice area with the presence of reflux (p = .002 and p = .024 respectively).
Conclusions
In this study, we developed an experimental model to enable careful evaluation of the elements of the anti-reflux mechanism, of which, the angle of His has a measurable element. We demonstrated that as the angle of His becomes wider the esophago-gastric orifice area becomes larger. Additionally, a wider angle of His and a larger esophago-gastric orifice area were correlated independently with more reflux. This suggests that the fundoplication creates an acute angle of His which is correlated with a smaller area of the esophago-gastric orifice and eventually with a lower incidence of reflux.








Similar content being viewed by others
Data Availability
The data that supports the findings of this article are available upon request.
References
Vakil N, Van Zanten S V, Kahrilas P, Dent J, Jones R. The Montreal Definition and Classification of Gastroesophageal Reflux Disease: A Global Evidence-Based Consensus CME. Am J Gastroenterol. 2006;101:1900-1920. https://doi.org/10.1111/j.1572-0241.2006.00630.x
Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122(5):1500-1511. https://doi.org/10.1053/GAST.2002.32978
Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001;111(8):174-177. https://doi.org/10.1016/S0002-9343(01)00828-2
Devault KR, Castell DO. Updated Guidelines for the Diagnosis and Treatment of Gastroesophageal Reflux Disease. https://doi.org/10.1111/j.1572-0241.2005.41217.x
Anvari M, Allen C, Borm A. Laparoscopic Nissen fundoplication is a satisfactory alternative to long-term omeprazole therapy. Br J Surg. 1995;82(7):938-942. https://doi.org/10.1002/bjs.1800820728
Slater BJ, Dirks RC, Mckinley SK, et al. SAGES GUIDELINES SAGES guidelines for the surgical treatment of gastroesophageal reflux (GERD). 2021;35:4903-4917. https://doi.org/10.1007/s00464-021-08625-5
Richter JE. Gastroesophageal Reflux Disease Treatment: Side Effects and Complications of Fundoplication. YJCGH. 2013;11:465-471. https://doi.org/10.1016/j.cgh.2012.12.006
Zornig C, Strate U, Fibbe C, Emmermann A, Layer P. Nissen vs Toupet laparoscopic fundoplication A prospective randomized study of 200 patients with and without preoperative esophageal motility disorders. Surg Endosc. 2002;16:758-766. https://doi.org/10.1007/s00464-001-9092-8
Fernando HC, Luketieh JD, Christie NA, Ikramuddin S, Schauer PR. Outcomes of laparoscopic Toupet compared to laparoscopic Nissen fundoplication. Surg Endosc. 2002;16:905-908. https://doi.org/10.1007/s004640080007
Ellis FH. The Nissen fundoplication. Ann Thorac Surg. 1992;54(6):1231-1235. https://doi.org/10.1016/0003-4975(92)90112-H
Gill RC, Bowes KL, Murphy PD, Jsingma YJ. Esophageal Motor Abnormalities in Gastroesophageal Reflux and the Effects of Fundoplication. Vol 91.; 1986. https://www.gastrojournal.org/article/0016-5085(86)90570-6/pdf. Accessed June 20, 2019.
Friedland GW. Historical Review of the Changing Concepts of Lower Esophageal Anatomy: 430 B.C.-1977.; 1978. http://www.ajronline.org. Accessed June 4, 2019.
His W. Studien an gehärteten Leichen über Form und Lagerung des menschlichen Magens. Arch Anat Physiol. 1903.
Cunningham DJ. II.—The Varying Form of the Stomach in Man and the Anthropoid Ape. Trans R Soc Edinburgh. 1906;45(1):9-47. https://doi.org/10.1017/S0080456800011625
Kim GH, Kang DH, Song GA, et al. Gastroesophageal flap valve is associated with gastroesophageal and gastropharyngeal reflux. J Gastroenterol. 2006;41(7):654-661. https://doi.org/10.1007/s00535-006-1819-9
Fujiwara Y, Higuchi K, Shiba M, et al. Association between gastroesophageal flap valve, reflux esophagitis, Barrett’s epithelium, and atrophic gastritis assessed by endoscopy in Japanese patients. J Gastroenterol. 2003;38(6):533-539. https://doi.org/10.1007/s00535-002-1100-9
Hansdotter I, Björ O, Andreasson A, et al. Hill classification is superior to the axial length of a hiatal hernia for assessment of the mechanical anti-reflux barrier at the gastroesophageal junction. 2016. https://doi.org/10.1055/s-0042-101021
Namikawa T, Kitagawa H, Okabayashi T, Sugimoto T, Kobayashi M, Hanazaki K. Roux-en-Y Reconstruction is Superior to Billroth I Reconstruction in Reducing Reflux Esophagitis After Distal Gastrectomy: Special Relationship with the Angle of His. World J Surg. 2010;34(5):1022-1027. https://doi.org/10.1007/s00268-010-0452-1
Namikawa T, Kitagawa H, Okabayashi T, Sugimoto T, Kobayashi M, Hanazaki K. Double tract reconstruction after distal gastrectomy for gastric cancer is effective in reducing reflux esophagitis and remnant gastritis with duodenal passage preservation. https://doi.org/10.1007/s00423-011-0777-8
Matikainen M, Kaukinen L. The mechanism of Nissen fundoplication. Acta Chir Scand. 1984;150(8):653–655. http://www.ncbi.nlm.nih.gov/pubmed/6532037. Accessed June 25, 2019.
O’Hanrahan T, Marples M, Bancewicz J. Recurrent reflux and wrap disruption after Nissen fundoplication: Detection, incidence and timing. Br J Surg. 1990;77(5):545-547. https://doi.org/10.1002/bjs.1800770526
Ismail T, Bancewicz J, Barlow J. Yield pressure, anatomy of the cardia and gastro‐oesophageal reflux. Br J Surg. 1995;82(7):943-947. https://doi.org/10.1002/BJS.1800820729
Revicki DA, Wood M, Maton PN, Sorensen S. The Impact of Gastroesophageal Reflux Disease on Health-related Quality of Life.
Ireland AC, Holloway RH, Toouli J, Dent J. Mechanisms underlying the antireflux action of fundoplication. Gut. 1993;34(3):303-308. https://doi.org/10.1136/gut.34.3.303
Thompson SK, David •, Watson I, Thompson SK, Watson DI. What is the Best Anti-Reflux Operation? All Fundoplications are Not Created Equal. World J Surg. 2015;39:997-999. https://doi.org/10.1007/s00268-015-3015-7
Gupta P, Parshad · Rajinder, Pavithra Balakrishna ·, et al. Angle of His Accentuation Is a Viable Alternative to Dor Fundoplication as an Adjunct to Laparoscopic Heller Cardiomyotomy: Results of a Randomized Clinical Study. Dig Dis Sci. 2018;63:2395-2404. https://doi.org/10.1007/s10620-018-5130-4
Watson DI, Mathew G, Pike GK, Jamieson GG. Comparison of anterior, posterior and total fundoplication using a viscera model. Dis Esophagus. 1997;10(2):110-114. https://doi.org/10.1093/dote/10.2.110
Watson A. Laparoscopic “physiological” antireflux procedure: preliminary results of a prospective symptomatic and objective study. Br J Surg. 1995;82:651-656. https://doi.org/10.1002/bjs.1800820527
Daud WNW, Thompson SK, Jamieson GG, Devitt PG, Martin IJG, Watson DI. Randomized controlled trial of laparoscopic anterior 180° partial versus posterior 270° partial fundoplication. ANZ J Surg. 2015;85(9):668-672. https://doi.org/10.1111/ANS.12476
Acknowledgements
The Experimental Surgery Laboratory Team.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Statement
This manuscript does not involve any experimentation on live animals. Hence, no ethics committee approval was required for this study.
Conflict of Interest
The authors declare no competing interests.
Disclaimer
This research was conducted with utmost integrity, transparency, and objectivity to ensure the credibility and reliability of the presented results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Michael, S., Marom, G., Brodie, R. et al. The Angle of His as a Measurable Element of the Anti-reflux Mechanism. J Gastrointest Surg 27, 2279–2286 (2023). https://doi.org/10.1007/s11605-023-05808-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05808-4