Abstract
Purpose
This study aimed to compare the oncological and functional outcomes following intersphincteric resection (ISR) with transverse coloplasty pouch (TCP) or straight coloanal anastomosis (SCAA) for low rectal cancer.
Methods
A single-center retrospective analysis was performed on patients with low rectal cancer who received ISR between January 2016 and June 2021. The primary endpoint was to compare the outcomes of bowel function within 1 year, 1 to 2 years, and 2 years after ileostomy closure in patients undergoing two different bowel reconstruction procedures (TCP or SCAA). The postoperative complications and oncological results were also compared between the two groups.
Results
A total of 235 patients were enrolled in this study (SCAA group: 166; TCP group: 69). There was no significant difference in complications, including grades A–C anastomotic leakage (9.6% vs 15.9%), 3-year local recurrence rates (6.1% vs 3.9%), disease-free survival (82.4%vs 83.8%), or overall survival (94.1% vs 94.7%) between the two groups. Two years after ileostomy closure, 52.7% of patients in the SCAA group were assessed as having major low anterior resection syndrome (LARS), which was significantly higher than the 25.9% of patients in the TCP group (P = 0.014), but no difference was found prior to 2 years. Similar differences were seen in Wexner scores 2 years after surgery (P = 0.032). Additionally, TCP was an independent protective factor for postoperative bowel function as measured by both the LARS (OR, 0.28; 95% CI, 0.10–0.82; p = 0.020) and Wexner scoring (OR, 0.28; 95% CI, 0.09–0.84; p = 0.023).
Conclusion
This study suggests that TCP is a safe technique that may decrease bowel dysfunction after ISR for low rectal cancer compared with SCAA 2 years after ileostomy closure.




Similar content being viewed by others
References
Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK: Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg 1998, 133(8):894-899.
Williams NS, Dixon MF, Johnston D: Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients' survival. Br J Surg 1983, 70(3):150-154.
Ueno H, Mochizuki H, Hashiguchi Y, Ishikawa K, Fujimoto H, Shinto E, Hase K: Preoperative parameters expanding the indication of sphincter preserving surgery in patients with advanced low rectal cancer. Ann Surg 2004, 239(1):34-42.
Schiessel R, Karner-Hanusch J, Herbst F, Teleky B, Wunderlich M: Intersphincteric resection for low rectal tumours. Br J Surg 1994, 81(9):1376-1378.
Rullier E, Zerbib F, Laurent C, Bonnel C, Caudry M, Saric J, Parneix M: Intersphincteric resection with excision of internal anal sphincter for conservative treatment of very low rectal cancer. Dis Colon Rectum 1999, 42(9):1168-1175.
Gamagami RA, Liagre A, Chiotasso P, Istvan G, Lazorthes F: Coloanal anastomosis for distal third rectal cancer: prospective study of oncologic results. Dis Colon Rectum 1999, 42(10):1272-1275.
Mulsow J, Winter DC: Sphincter preservation for distal rectal cancer--a goal worth achieving at all costs? World J Gastroenterol 2011, 17(7):855-861.
Chen TY, Wiltink LM, Nout RA, Meershoek-Klein Kranenbarg E, Laurberg S, Marijnen CA, van de Velde CJ: Bowel function 14 years after preoperative short-course radiotherapy and total mesorectal excision for rectal cancer: report of a multicenter randomized trial. Clin Colorectal Cancer 2015, 14(2):106-114.
Borstlap WAA, Westerduin E, Aukema TS, Bemelman WA, Tanis PJ: Anastomotic Leakage and Chronic Presacral Sinus Formation After Low Anterior Resection: Results From a Large Cross-sectional Study. Ann Surg 2017, 266(5):870-877.
Lazorthes F, Fages P, Chiotasso P, Lemozy J, Bloom E: Resection of the rectum with construction of a colonic reservoir and colo-anal anastomosis for carcinoma of the rectum. Br J Surg 1986, 73(2):136-138.
Dehni N, Tiret E, Singland JD, Cunningham C, Schlegel RD, Guiguet M, Parc R: Long-term functional outcome after low anterior resection: comparison of low colorectal anastomosis and colonic J-pouch-anal anastomosis. Dis Colon Rectum 1998, 41(7):817-822; discussion 822-813.
Huber FT, Herter B, Siewert JR: Colonic pouch vs. side-to-end anastomosis in low anterior resection. Dis Colon Rectum 1999, 42(7):896-902.
Machado M, Nygren J, Goldman S, Ljungqvist O: Similar outcome after colonic pouch and side-to-end anastomosis in low anterior resection for rectal cancer: a prospective randomized trial. Ann Surg 2003, 238(2):214-220.
Z'Graggen K, Maurer CA, Büchler MW: Transverse coloplasty pouch. A novel neorectal reservoir. Dig Surg 1999, 16(5):363-366.
Brown CJ, Fenech DS, McLeod RS: Reconstructive techniques after rectal resection for rectal cancer. Cochrane Database Syst Rev 2008, 2008(2):Cd006040.
Hüttner FJ, Tenckhoff S, Jensen K, Uhlmann L, Kulu Y, Büchler MW, Diener MK, Ulrich A: Meta-analysis of reconstruction techniques after low anterior resection for rectal cancer. Br J Surg 2015, 102(7):735-745.
Hida J, Yasutomi M, Maruyama T, Tokoro T, Wakano T, Uchida T: Enlargement of colonic pouch after proctectomy and coloanal anastomosis: potential cause for evacuation difficulty. Dis Colon Rectum 1999, 42(9):1181-1188.
Harris GJC, Lavery IJ, Fazio VW: Reasons for failure to construct the colonic J-pouch. What can be done to improve the size of the neorectal reservoir should it occur? Dis Colon Rectum 2002, 45(10):1304-1308. https://doi.org/10.1007/s10350-004-6414-7
Doeksen A, Bakx R, Vincent A, van Tets WF, Sprangers MA, Gerhards MF, Bemelman WA, van Lanschot JJ: J-pouch vs side-to-end coloanal anastomosis after preoperative radiotherapy and total mesorectal excision for rectal cancer: a multicentre randomized trial. Colorectal Dis 2012, 14(6):705-713.
Rubin F, Douard R, Wind P: The functional outcomes of coloanal and low colorectal anastomoses with reservoirs after low rectal cancer resections. Am Surg 2014, 80(12):1222-1229.
Ribi K, Marti WR, Bernhard J, Grieder F, Graf M, Gloor B, Curti G, Zuber M, Demartines N, Andrieu C et al: Quality of Life After Total Mesorectal Excision and Rectal Replacement: Comparing Side-to-End, Colon J-Pouch and Straight Colorectal Reconstruction in a Randomized, Phase III Trial (SAKK 40/04). Ann Surg Oncol 2019, 26(11):3568-3576.
Gavaruzzi T, Pace U, Giandomenico F, Pucciarelli S, Bianco F, Selvaggi F, Restivo A, Asteria CR, Morpurgo E, Cuicchi D et al: Colonic J-Pouch or Straight Colorectal Reconstruction After Low Anterior Resection For Rectal Cancer: Impact on Quality of Life and Bowel Function: A Multicenter Prospective Randomized Study. Dis Colon Rectum 2020, 63(11):1511-1523.
Biondo S, Frago R, Codina Cazador A, Farres R, Olivet F, Golda T, Miguel B, Kreisler E: Long-term functional results from a randomized clinical study of transverse coloplasty compared with colon J-pouch after low anterior resection for rectal cancer. Surgery 2013, 153(3):383-392.
Harris GJ, Lavery IJ, Fazio VW: Reasons for failure to construct the colonic J-pouch. What can be done to improve the size of the neorectal reservoir should it occur? Dis Colon Rectum 2002, 45(10):1304-1308.
Köninger JS, Butters M, Redecke JD, Z'Graggen K: Transverse coloplasty pouch after total mesorectal excision: functional assessment of evacuation. Dis Colon Rectum 2004, 47(10):1586-1593.
Pucciarelli S, Del Bianco P, Pace U, Bianco F, Restivo A, Maretto I, Selvaggi F, Zorcolo L, De Franciscis S, Asteria C et al: Multicentre randomized clinical trial of colonic J pouch or straight stapled colorectal reconstruction after low anterior resection for rectal cancer. Br J Surg 2019, 106(9):1147-1155.
Brown S, Margolin DA, Altom LK, Green H, Beck DE, Kann BR, Whitlow CB, Vargas HD: Morbidity Following Coloanal Anastomosis: A Comparison of Colonic J-Pouch vs Straight Anastomosis. Dis Colon Rectum 2018, 61(2):156-161.
Liao C, Gao F, Cao Y, Tan A, Li X, Wu D: Meta-analysis of the colon J-pouch vs transverse coloplasty pouch after anterior resection for rectal cancer. Colorectal Dis 2010, 12(7):624-631.
Fritz S, Hennig R, Kantas C, Killguss H, Schaudt A, Feilhauer K, Köninger J: The transverse coloplasty pouch is technically easy and safe and improves functional outcomes after low rectal cancer resection-a single center experience with 397 patients. Langenbecks Arch Surg 2021, 406(3):833-841.
Pimentel JM, Duarte A, Gregório C, Souto P, Patrício J: Transverse coloplasty pouch and colonic J-pouch for rectal cancer--a comparative study. Colorectal Dis 2003, 5(5):465-470.
Fürst A, Suttner S, Agha A, Beham A, Jauch KW: Colonic J-pouch vs. coloplasty following resection of distal rectal cancer: early results of a prospective, randomized, pilot study. Dis Colon Rectum 2003, 46(9):1161-1166.
Ihn MH, Kang SB, Kim DW, Oh HK, Lee SY, Hong SM: Risk factors for bowel dysfunction after sphincter-preserving rectal cancer surgery: a prospective study using the Memorial Sloan Kettering Cancer Center bowel function instrument. Dis Colon Rectum 2014, 57(8):958-966.
Park YY, Yang SY, Han YD, Cho MS, Hur H, Min BS, Lee KY, Kim NK: Predictive Factors for Bowel Dysfunction After Sphincter-Preserving Surgery for Rectal Cancer: A Single-Center Cross-sectional Study. Dis Colon Rectum 2019, 62(8):925-933.
Darwich I, Rustanto D, Friedberg R, Willeke F: Spectrophotometric assessment of bowel perfusion during low anterior resection: a prospective study. Updates Surg 2019, 71(4):677-686.
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y et al: Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 2010, 147(3):339-351.
Emmertsen KJ, Laurberg S: Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 2012, 255(5):922-928.
Jorge JM, Wexner SD: Etiology and management of fecal incontinence. Dis Colon Rectum 1993, 36(1):77-97.
Battersby NJ, Juul T, Christensen P, Janjua AZ, Branagan G, Emmertsen KJ, Norton C, Hughes R, Laurberg S, Moran BJ: Predicting the Risk of Bowel-Related Quality-of-Life Impairment After Restorative Resection for Rectal Cancer: A Multicenter Cross-Sectional Study. Dis Colon Rectum 2016, 59(4):270-280.
Hohenberger W, Merkel S, Matzel K, Bittorf B, Papadopoulos T, Göhl J: The influence of abdomino-peranal (intersphincteric) resection of lower third rectal carcinoma on the rates of sphincter preservation and locoregional recurrence. Colorectal Dis 2006, 8(1):23-33.
Chi P, Huang SH, Lin HM, Lu XR, Huang Y, Jiang WZ, Xu ZB, Chen ZF, Sun YW, Ye DX: Laparoscopic transabdominal approach partial intersphincteric resection for low rectal cancer: surgical feasibility and intermediate-term outcome. Ann Surg Oncol 2015, 22(3):944-951.
Huang S, Chen M, Deng Y, Wang X, Lu X, Jiang W, Huang Y, Chi P: Mesorectal fat area and mesorectal area affect the surgical difficulty of robotic-assisted mesorectal excision and intersphincteric resection respectively in different ways. Colorectal Dis 2020, 22(9):1130-1138.
Weiser MR, Quah HM, Shia J, Guillem JG, Paty PB, Temple LK, Goodman KA, Minsky BD, Wong WD: Sphincter preservation in low rectal cancer is facilitated by preoperative chemoradiation and intersphincteric dissection. Ann Surg 2009, 249(2):236-242.
Tilney HS, Tekkis PP: Extending the horizons of restorative rectal surgery: intersphincteric resection for low rectal cancer. Colorectal Dis 2008, 10(1):3-15; discussion 15-16.
Furnee EJB, Aukema TS, Oosterling SJ, Borstlap WAA, Bemelman WA, Tanis PJ, Dutch Snapshot Research G: Influence of Conversion and Anastomotic Leakage on Survival in Rectal Cancer Surgery; Retrospective Cross-sectional Study; J Gastrointest Surg 2019, 23(10):2007-2018.
Shirouzu K, Murakami N, Akagi Y: Intersphincteric resection for very low rectal cancer: A review of the updated literature. Ann Gastroenterol Surg 2017, 1(1):24-32.
Rullier E, Denost Q, Vendrely V, Rullier A, Laurent C: Low rectal cancer: classification and standardization of surgery. Dis Colon Rectum 2013, 56(5):560-567.
Denost Q, Moreau JB, Vendrely V, Celerier B, Rullier A, Assenat V, Rullier E: Intersphincteric resection for low rectal cancer: the risk is functional rather than oncological. A 25-year experience from Bordeaux. Colorectal Dis 2020, 22(11):1603-1613.
Lorenzi B, Brading AF, Martellucci J, Cetta F, Mortensen NJ: Short-term effects of neoadjuvant chemoradiotherapy on internal anal sphincter function: a human in vitro study. Dis Colon Rectum 2012, 55(4):465-472.
Acknowledgments
The authors thank all the staff at the Department of Colorectal Surgery, Fujian Medical University Union Hospital (FMUUH, Fuzhou, China).
Funding
Joint funds for the innovation of science and technology in Fujian province (2017Y9038, 2019Y9101, 2020Y9071); Fujian Provincial Health Technology Project (2020GGB022, 2020CXA025); Natural Science Foundation of Fujian Province (2020J011030, 2022J01753); Medical Science Research Foundation of Beijing Medical and Health Foundation(B20062DS); Bethune Charitable Foundation(X-J-2018-004).
Author information
Authors and Affiliations
Contributions
HP, ZZha, SH, YH, and PC conceived and designed the project. HP and YD collected the data. ZZha and ZZhe analyzed and interpreted the data. HP and SH drafted the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Esm 1:
Supplemental Figure 1. Flow chart of the study. (TIF 2423 kb)
Esm 2:
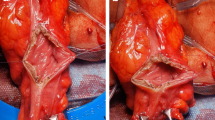
Supplemental Figure 2. Construction of the transverse coloplasty pouch (TCP). For creation of the TCP, a 5cm longitudinal incision was made 5cm proximally to the colon resection margin(a), and transverse suture was performed (b). (TIF 2007 kb)
Esm 3:
Supplemental Figure 3 Postoperative gastrografin enema for patients who underwent intersphincteric resection with transverse coloplasty pouch (TCP). (TIFF 1056 kb)
Esm 4
Table S1. Postoperative complications after intersphincteric resection with SCAA or TCP. (DOCX 14 kb)
Esm 5
Table S2. Functional outcomes of SCAA and TCP. (DOCX 14 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, H., Zhao, Z., Deng, Y. et al. Transverse Coloplasty Pouch versus Straight Coloanal Anastomosis Following Intersphincteric Resection for Low Rectal Cancer: the Functional Benefits May Emerge After Two Years. J Gastrointest Surg 27, 2526–2537 (2023). https://doi.org/10.1007/s11605-022-05565-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05565-w