Abstract
Background
Most patients undergoing esophagectomy will experience intermittent reflux of gastric and biliary content into the remnant esophagus postoperatively. The incidence of new or recurrent intestinal metaplasia following chemoradiation and surgery has not been well-described. Furthermore, post-resection guidelines do not exist regarding surveillance for metaplasia in the esophageal remnant.
Methods
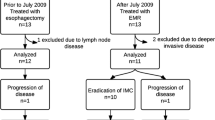
Patients undergoing Ivor Lewis esophagectomy after concurrent chemoradiation for a diagnosis of esophageal adenocarcinoma from 2006 to 2018 were identified. Pathology records were reviewed for the presence of intestinal metaplasia on pretreatment biopsies, surgical specimen, or post-resection biopsies.
Results
In total, 619 patients met inclusion criteria, including 267 (43%) who had intestinal metaplasia noted either prior to or at the time of esophagectomy. The median duration of metaplastic disease prior to resection was 4.4 months. During a median follow-up time of 28 months (interquartile range, 12–60), intestinal metaplasia was noted in the remnant esophagus in 12 (2%) patients, 7 of whom had a prior history of metaplasia. Local recurrence of adenocarcinoma was also uncommon, and occurred in 37/577 (6%) of patients with complete resections, with similar event rates among those with and without a prior history of metaplasia (14/249 [6%] vs. 23/328 [7%], p = 0.614).
Conclusions
Our findings suggest that despite several factors predisposing to mucosal damage following esophagectomy, occurrence of new intestinal metaplasia after trimodality therapy in our patient population appears to be rare, even among patient with a previous history of this pathologic finding, which may have significant implications for surveillance and cost-savings after resection.

Similar content being viewed by others
References
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371(9):836-45.
Gutschow CA, Schroder W, Holscher AH. Barrett’s esophagus: what is the poison - alkaline, biliary or acidic reflux? Dis Esophagus. 2002;15(1):5-9.
Aiyer HS, Li Y, Harper N, Myers SR, Martin RC. Molecular changes in the esophageal epithelium after a subchronic exposure to cigarette smoke in the presence of bile-acid reflux. Inhal Toxicol. 2011;23(5):304-11.
Nishijima K, Miwa K, Miyashita T, Kinami S, Ninomiya I, Fushida S, Fujimura T, Hattori T. Impact of the biliary diversion procedure on carcinogenesis in Barrett’s esophagus surgically induced by duodenoesophageal reflux in rats. Ann Surg. 2004;240(1):57-67.
Pera M, Trastek VF, Carpenter HA, Fernandez PL, Cardesa A, Mohr U, Pairolero PC.Influence of pancreatic and biliary reflux on the development of esophageal carcinoma. Ann Thorac Surg. 1993;55(6):1386-92; discussion 92-3.
Belghazi K, van Vilsteren FGI, Weusten B, Meijer SL, Bergman J, Pouw RE. Long-term follow-up results of stepwise radical endoscopic resection for Barrett’s esophagus with early neoplasia. Gastrointest Endosc. 2018;87(1):77-84.
Codipilly DC, Chandar AK, Singh S, Wani S, Shaheen NJ, Inadomi JM, Chak A, Iyer PG. The Effect of endoscopic surveillance in patients with Barrett’s esophagus: a systematic review and meta-analysis. Gastroenterology. 2018;154(8):2068-86.e5.
NCCN. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Esophageal and esophagogastric junction cancers, version 1.2020 2020 [updated March 18, 2020. Available from: https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf.
Sudo K, Taketa T, Correa AM, Campagna MC, Wadhwa R, Blum MA, Komaki R, Lee JH, Bhutani MS, Weston B, Skinner HD, Maru DM, Rice DC, Swisher SG, Hofstetter WL, Ajani JA. Locoregional failure rate after preoperative chemoradiation of esophageal adenocarcinoma and the outcomes of salvage strategies. J Clin Oncol. 2013;31(34):4306-10.
Taketa T, Sudo K, Correa AM, Wadhwa R, Shiozaki H, Elimova E, Campagna MC, Blum MA, Skinner HD, Komaki RU, Lee JH, Bhutani MS, Weston BR, Rice DC, Swisher SG, Maru DM, Hofstetter WL, Ajani JA. Post-chemoradiation surgical pathology stage can customize the surveillance strategy in patients with esophageal adenocarcinoma. J Natl Compr Canc Netw. 2014;12(8):1139-44.
Shewale JB, Nelson DB, Rice DC, Sepesi B, Hofstetter WL, Mehran RJ, Vaporciyan AA, Walsh GL, Swisher SG, Roth JA, Antonoff MB. Natural history of ground-glass lesions among patients with previous lung cancer. Ann Thorac Surg. 2018;105(6):1671-7.
Zhou N, Corsini EM, Jin S, Barbosa GR, Kell T, Antonoff MH, Antonoff MB. Advanced data analytics for clinical research part I: what are the tools? Innovations (Phila). 2020:1556984520902783.
Zhou N, Corsini EM, Jin S, Barbosa GR, Kell T, Antonoff MH, Antonoff MB. Advanced data analytics for clinical research part II: application to cardiothoracic surgery. Innovations (Phila). 2020:1556984520902824.
Meyer W, Vollmar F, Bar W. Barrett-esophagus following total gastrectomy. A contribution to it’s pathogenesis. Endoscopy. 1979;11(2):121-6.
Anders M, Bahr C, El-Masry MA, Marx AH, Koch M, Seewald S, Schachschal G, Adler A, Soehendra N, Izbicki J, Neuhaus P, Pohl H, Rosch T. Long-term recurrence of neoplasia and Barrett’s epithelium after complete endoscopic resection. Gut. 2014;63(10):1535-43.
Hong J, Behar J, Wands J, Resnick M, Wang LJ, Delellis RA, Lambeth D, Cao W. Bile acid reflux contributes to development of esophageal adenocarcinoma via activation of phosphatidylinositol-specific phospholipase Cgamma2 and NADPH oxidase NOX5-S. Cancer Res. 2010;70(3):1247-55.
Salama TMS, Hassan MI. Incidence of biliary reflux esophagitis after laparoscopic omega loop gastric bypass in morbidly obese patients. J Laparoendosc Adv Surg Tech A. 2017;27(6):618-22.
Taha AS, Angerson WJ, Morran CG. Reflux and Barrett’s oesophagitis after gastric surgery--long-term follow-up and implications for the roles of gastric acid and bile in oesophagitis. Aliment Pharmacol Ther. 2003;17(4):547-52.
Avidan B, Sonnenberg A, Schnell TG, Sontag SJ. Gastric surgery is not a risk for Barrett’s esophagus or esophageal adenocarcinoma. Gastroenterology. 2001;121(6):1281-5.
Akiyama T, Inamori M, Akimoto K, Iida H, Endo H, Hosono K, Ikeda T, Sakamoto Y, Fujita K, Yoneda M, Koide T, Takahashi H, Tokoro C, Goto A, Abe Y, Kobayashi N, Kubota K, Saito S, Moriya A, Rino Y, Imada T, Nakajima A. Gastric surgery is not a risk factor for erosive esophagitis or Barrett’s esophagus. Scand J Gastroenterol. 2010;45(4):403-8.
Parrilla P, Liron R, Martinez de Haro LF, Ortiz A, Molina J, De Andres B. Gastric surgery does not increase the risk of developing Barrett’s esophagus. Am J Gastroenterol. 1997;92(6):960-3.
Chang LC, Oelschlager BK, Quiroga E, Parra JD, Mulligan M, Wood DE, Pellegrini CA. Long-term outcome of esophagectomy for high-grade dysplasia or cancer found during surveillance for Barrett's esophagus. J Gastrointest Surg. 2006;10(3):341-6.
Pacifico RJ, Wang KK, Wongkeesong LM, Buttar NS, Lutzke LS. Combined endoscopic mucosal resection and photodynamic therapy versus esophagectomy for management of early adenocarcinoma in Barrett's esophagus. Clin Gastroenterol Hepatol. 2003;1(4):252-7.
Lord RV, Wickramasinghe K, Johansson JJ, Demeester SR, Brabender J, Demeester TR. Cardiac mucosa in the remnant esophagus after esophagectomy is an acquired epithelium with Barrett's-like features. Surgery. 2004;136(3):633-40.
Dunn LJ, Burt AD, Hayes N, Griffin SM. Columnar metaplasia in the esophageal remnant after esophagectomy: a common occurrence and a valuable insight into the development of Barrett esophagus. Ann Surg. 2016;264(6):1016-21.
Acknowledgements
The authors are indebted to Jeff Jin and the University of Texas MD Anderson Institutional Analytics and Informatics Support Team, who were instrumental in identifying the patients for our study.
Funding
This work was supported by generous philanthropic donations by the Mason Family Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare no conflict of interest/competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Corsini, E.M., Mitchell, K.G., Zhou, N. et al. Intestinal Metaplasia in the Esophageal Remnant Is Rare After Ivor Lewis Esophagectomy. J Gastrointest Surg 25, 2185–2191 (2021). https://doi.org/10.1007/s11605-021-04909-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-04909-2