Abstract
Background
The aim of this study was to evaluate the predictive value of measuring indocyanine green (ICG) clearance during intraoperative partial occlusion of liver lobes to be resected on postoperative liver function following major anatomic liver resection.
Methods
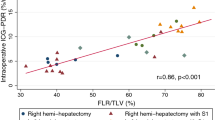
We prospectively included 46 patients, and 35 patients ultimately underwent anatomic major liver resection. ICG clearance was measured preoperatively and intraoperatively. Intraoperative ICG clearance was measured immediately after selective occlusion of hepatic arterial, portal, and hepatic venous blood flow to the liver lobes to be resected. The albumin-bilirubin (ALBI) grade, albumin-indocyanine green evaluation (ALICE) grade, platelet count, remnant liver volume per kilogram of weight (RLV/kg), and future liver remnant plasma clearance rate of ICG (ICGK-FLR) were measured preoperatively.
Results
An intraoperative ICG retention at 15 min (I-R15) greater than 13.8% indicates transient posthepatectomy liver failure (PHLF) and Clavien-Dindo > grade I complications. Receiver operating characteristic (ROC) curve analysis revealed that the area under the curve (AUC) for predicting PHLF and Clavien-Dindo > grade I complications was 0.797 and 0.734, respectively (p = 0.001 and 0.014). Furthermore, an I-R15 greater than 22.7% indicates mid-term PHLF, and the AUC was 0.911 (p < 0.0001). The I-R15 is a better predictor of PHLF than the ALBI grade, ALICE grade, platelet count, RLV/kg, and ICGK-FLR.
Conclusions
Intraoperative ICG clearance measurements during partial occlusion of blood flow accurately predict postoperative liver function and could be new criteria for determining the feasibility and safety of anatomic major liver resection.




Similar content being viewed by others
References
Katsube T, Okada M, Kumano S, Hori M, Imaoka I, Ishii K, et al. Estimation of liver function using T1 mapping on Gd-EOB-DTPAenhanced magnetic resonance imaging. Invest Radiol 2011;46:277–283. doi: https://doi.org/10.1097/RLI.0b013e318200f67d.
Pawlik TM, Schulick RD, Choti MA. Expanding criteria for resectability of colorectal liver metastases. Oncologist 2008;13:51–64. doi: https://doi.org/10.1634/theoncologist.2007-0142.
Kishi Y, Abdalla EK, Chun YS, Zorzi D, Madoff DC, Wallace MJ, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg 2009;250:540–548. doi: https://doi.org/10.1097/SLA.0b013e3181b674df.
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 2005;242:824–829.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011;149:713–724. doi: https://doi.org/10.1016/j.surg.2010.10.001.
Kamath PS, Kim WR. The model of end-stage liver disease (MELD). Hepatology 2007;45:797–805. doi: https://doi.org/10.1002/hep.21563.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–845.
Yokoyama Y, Nishio H, Ebata T, Igami T, Sugawara G, Nagino M. Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 2010;97:1260–1268. doi: https://doi.org/10.1002/bjs.7084.
Thomas MN, Weninger E, Angele M, Bösch F, Pratschke S, Andrassy J, et al. Intraoperative simulation of remnant liver function during anatomic liver resection with indocyanine green clearance (LiMON) measurements. HPB (Oxford) 2015;17:471–476. doi: https://doi.org/10.1111/hpb.12380.
de Graaf W, Bennink RJ, Veteläinen R, van Gulik TM. Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med 2010;51:742–752. doi: https://doi.org/10.2967/jnumed.109.069435.
Bennink RJ, Tulchinsky M, de Graaf W, Kadry Z, van Gulik TM. Liver function testing with nuclear medicine techniques is coming of age. Semin Nucl Med 2012;42:124–137. doi: https://doi.org/10.1053/j.semnuclmed.2011.10.003.
Financial Support
This work was jointly supported by Wu Jieping Medical Foundation (320.2710.1857), National Natural Science Foundation of China (81874182, 81874056), National Key Project of China (2017ZX10203204-007-004), Public Health Bureau Foundation of Shanghai (201840019), and Research Talent Foundation of Fudan University Shanghai Cancer Center (YJRC1604).
Author information
Authors and Affiliations
Contributions
Longrong Wang, Li Xie, and Ning Zhang contributed equally to this study. All authors had access to the study data and had reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
Longrong Wang Activities related to the present article: disclosed no relevant relationship. Activities not related to the present article: author received grants from Wu Jieping Medical Foundation, China. Other relationships: none to disclose. Weiping Zhu Activities related to the present article: disclosed no relevant relationship. Activities not related to the present article: author received grants from National Natural Science Foundation of China and Public Health Bureau Foundation of Shanghai, China. Other relationships: none to disclose. Lu Wang Activities related to the present article: disclosed no relevant relationship. Activities not related to the present article: author received grants from National Natural Science Foundation of China, National Key Project of China and Research Talent Foundation of Fudan University Shanghai Cancer Center, China. Other relationships: none to disclose. Yiming Zhao, Li Xie, Ning Zhang, Jiamin Zhou, Qi Pan, Anrong Mao and Zhenhai Lin Activities to the present article: none to disclose. Activities not related to the present article: none to disclose. Other relationships: none to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Supplementary Table 1
(XLSX 37 kb)
Supplementary Table 2
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Wang, L., Xie, L., Zhang, N. et al. Predictive Value of Intraoperative Indocyanine Green Clearance Measurement on Postoperative Liver Function After Anatomic Major Liver Resection. J Gastrointest Surg 24, 1342–1351 (2020). https://doi.org/10.1007/s11605-019-04262-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04262-5