Abstract
Purpose
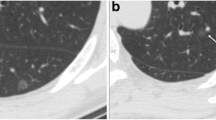
To investigate the differentiating computed tomographic (CT) features between adenocarcinoma in situ (AIS) with alveolar collapse and minimally invasive adenocarcinoma (MIA) or invasive adenocarcinoma (IA) appearing as part-solid nodules.
Methods
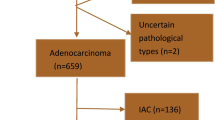
A total of 147 consecutive patients with 157 pathology-confirmed part-solid ground-glass nodules (GGNs) ≤ 20 mm without other pathological condition such as inflammation and fibrosis who underwent chest CT were included.
Results
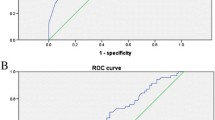
The 157 part-solid GGNs included 33 (21.02%) pathologically confirmed AISs with alveolar collapse. Multivariate analysis revealed that smaller lesion size (odds ratio [OR] 0.671), and well-defined border (OR 5.544), concentrated distribution (OR 7.994), and homogeneity of the solid portion (OR 4.365) were significant independent predictors for differentiating AIS with alveolar collapse from MIA (P < 0.05) with excellent accuracy (area under receiver operating characteristic [ROC] curve, 0.902). Multivariate analysis revealed that smaller lesion size (OR 0.782), and size (OR 0.821), well-defined border (OR 5.752), and homogeneity of solid portion (OR 6.182) were significant independent predictors differentiating AIS with alveolar collapse from IA (P < 0.05) with excellent accuracy (area under ROC curve 0.910).
Conclusion
Among part-solid GGNs, AIS with alveolar collapse can be accurately differentiated from MIA on the basis of smaller lesion size, well-defined border, concentrated distribution, and homogeneity of solid portion, and from IA according to smaller lesion size, and smaller size, well-defined border, and homogeneity of solid portion.



Similar content being viewed by others
Abbreviations
- AIS:
-
Adenocarcinoma in situ
- ATS:
-
American Thoracic Society
- AUC:
-
Area under the curve
- CT:
-
Computed tomography
- ERS:
-
European Respiratory Society
- GGN:
-
Ground-glass nodule
- GGN:
-
Ground-glass nodules
- HU:
-
Hounsfield Units
- IA:
-
Invasive adenocarcinoma
- IASLC:
-
International Association for the Study of Lung Cancer
- ICC:
-
Intra-class correlation coefficient
- IPA:
-
Invasive pulmonary adenocarcinoma
- MIA:
-
Minimally invasive adenocarcinoma
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
References
Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc. 2011;8:381–5.
Van Schil PE, Asamura H, Rusch VW, et al. Surgical implications of the new IASLC/ATS/ERS adenocarcinoma classification. Eur Respir J. 2012;39:478–86.
Watanable S, Watanable T, Arai K, Kasai T, Haratake J, Urayama H. Results of wedege resection for focal bronchioloalveolar carcinoma showing pure ground-glass attenuation on computed tomography. Ann Thorac Surg. 2002;73:1071–5.
Koike T, Togashi K, Shirato T, et al. Limited resection for noninvasive bronchioloalveolar carcinoma diagnosed by intraoperative pathologic examination. Ann Thorac Surg. 2009;88:1106–11.
Austin JH, Garg K, Aberle D, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013;266:62–71.
Naidich DP, Bankier AA, Macmahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266:304–17.
Lee HJ, Goo JM, Lee CH, Yoo CG, Kim YT, Im JG. Nodular ground-glass opacities on thin-section CT: size change during follow-up and pathological results. Korean J Radiol. 2007;8:22–31.
Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology. 2013;268:265–73.
Park CM, Goo JM, Lee HJ, Lee CH, Chun EJ, Im JG. Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up. Radiographics. 2007;27:391–408.
Noguchi M, Morikawa A, Kawasaki M, et al. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer. 1995;75:2844–52.
Hwanq EJ, Park CM, Ryu Y, et al. Pulmonary adenocarcinomas appearing as part-solid ground-glass nodules: is measuring solid component size a better prognostic indicator? Eur Radiol. 2015;25:558–67.
Chae HD, Park CM, Park SJ, Lee SM, Kim KG, Goo JM. Computerized texture analysis of persistent part-solid ground-glass nodules: differentiation of preinvasive lesions from invasive pulmonary adenocarcinomas. Radiology. 2014;273:285–93.
Henschke CI, Yankelevitz DF, Mirtcheva R, et al. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002;178:1053–7.
Kim H, Park CM, Koh JM, Lee SM, Goo JM. Pulmonary subsolid nodules: what radiologists need to know about the imaging features and management strategy. Diagn Interv Radiol. 2014;20:47–57.
Matsuguma H, Mori K, Nakahara R, et al. Characteristics of subsolid pulmonary nodules showing growth during follow-up with CT scanning. Chest. 2013;143:436–43.
Sim HJ, Choi SH, Chae EJ, et al. Surgical management of pulmonary adenocarcinoma presenting as a pure ground-glass nodule. Eur J Cardiothorac Surg. 2014;46:632–6.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e93S-e120S.
Krochmal R, Arias S, Yarmus L, Feller-Kopman D, Lee H. Diagnosis and management of pulmonary nodules. Expert Rev Respir Med. 2014;8:677–91.
Honda T, Kondo T, Murakami S, et al. Radiographic and pathological analysis of small lung adenocarcinoma using the new IASLC classification. Clin Radiol. 2013;68:e21–6.
Yamato Y, Tsuchida M, Wantanbe T, et al. Early results of a prospective study of limited resection for bronchioloalveolar adenocarcinoma of the lung. Ann Thorac Surg. 2001;71:971–4.
Yoshida J, Naga K, Yokose T, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg. 2005;129:991–6.
Tsutani Y, Miyata Y, Mimae T, et al. The prognostic role of pathologic invasive component size, excluding lepidic growth, in stage I lung adenocarcinoma. J Thorac Cardiovasc Surg. 2013;146:580–5.
Son JY, Lee KS, Kim JH, et al. Quantitative analysis of pulmonary ground-glass opacity nodules for the distinction of invasive adenocarcinoma from pre-invasive or minimally invasive adenocarcinoma. PLoS ONE. 2014;9:e104066.
Eguchi T, Yoshizawa A, Kawakami S, et al. Tumor size and computed tomography attenuation of pulmonary pure ground-glass nodules are useful for predicting pathological invasiveness. PLoS ONE. 2014;9:e97867.
Lindell RM, Hartman TE, Swensen SJ, Jett JR, Midthun DE, Mandrekar JN. 5-year lung cancer screening experience: growth curves of 18 lung cancers compared to histologic type, CT attenuation, stage, survival, and size. Chest. 2009;136:1586–95.
Lee SW, Leem CS, Kim TJ, et al. The long-term course of ground-glass opacities detected on thin-section computed tomography. Respir Med. 2013;107:904–10.
Ohde Y, Nagai K, Yoshida J, et al. The pro-portion of consolidation to ground-glass opacity on high resolution CT is a good predictor for distinguishing the population of non-invasive peripheral adenocarcinoma. Lung Cancer. 2003;42:303–10.
Suzuki K, Koike T, Asakawa T, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011;6:751–6.
Tsutani Y, Miyata Y, Nakayama H, et al. Prognostic significance of using solid versus whole tumor size on high-resolution computed tomography for predicting pathologic malignant grade of tumors in clinical stage IA lung adenocarcinoma: a multicenter study. J Thorac Cardiovasc Surg. 2012;143:607–12.
Lee KH, Goo JH, Park SJ, et al. Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol. 2014;9:74–82.
Acknowledgements
This work was supported by grants from the Scientific Research Foundation of Ministry of Public Health of China/Major Science and Technology Program of Medicine and Health of Zhejiang Province of China (grant no. WKJ2014-2-021), Heath and Family Planning Commission of Zhejiang Province (grant no. 2015ZDA032) and Public Project of Science Technology Department of Zhejiang Province of China (grant no. 2015C33254).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LX, SL and YZ. The first draft of the manuscript was written by LX and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LX, SL and YZ declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Xu, L., Lin, S. & Zhang, Y. Differentiation of adenocarcinoma in situ with alveolar collapse from minimally invasive adenocarcinoma or invasive adenocarcinoma appearing as part-solid ground-glass nodules (≤ 2 cm) using computed tomography. Jpn J Radiol 40, 29–37 (2022). https://doi.org/10.1007/s11604-021-01183-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-021-01183-9