Abstract
Background
The aim of this study was to compare postoperative immobilization techniques of the thumb metacarpophalangeal (MP) ulnar collateral ligament (UCL) in a cadaver model of a noncompliant patient.
Methods
A cadaveric model with fresh-frozen forearms was used to simulate pinch under two immobilization conditions: (1) forearm-based thumb spica splint alone and (2) forearm-based thumb spica splint with supplemental transarticular MP Kirschner wire fixation. Pinch was simulated by thumb valgus loading and flexor pollicis longus (FPL) loading. Ulnar collateral ligament displacements were measured and strain values calculated. Statistical analysis was performed using a repeated measures analysis of variance model.
Results
With valgus thumb loading, we noted a significantly lower UCL strain in the splint and pin group compared to splint immobilization alone. Increased load was associated with a statistically significant increase in UCL strain within each immobilization condition. FPL loading resulted in negative displacement, or paradoxical shortening, of the UCL in both immobilization groups.
Conclusions
While immobilized, valgus thumb force, as opposed to MP flexion, is a likely contributor to UCL strain during simulated pinch representing noncompliance during the postoperative period. Supplemental thumb MP pin fixation more effectively protects the UCL from valgus strain. UCL shortening with FPL loading likely represents paradoxical MP extension due to flexion of the distal phalanx against the distal splint, suggesting attempted thumb flexion with splint immobilization alone does not jeopardize UCL repair.
Clinical Relevance
This study provides a foundation to aid clinical decision-making after UCL repair. It reinforces the practice of surgeons who routinely pin their MP joints, but also brings to attention that the use of temporary MP pin fixation may be considered in difficult cases, such as those with potential noncompliance or tenuous repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute injuries to the thumb metacarpophalangeal (MP) ulnar collateral ligament (UCL) are common. The mechanism of injury often involves excessive radially directed force on an abducted thumb. Without adequate treatment, the management of complete tears may result in chronic valgus instability of the thumb, leading to difficulty with grasp and pinch activities. Partial injuries of the proper ulnar collateral ligament and complete injuries in situ may be treated nonoperatively with immobilization [8]. Complete disruptions, especially those involving the Stener lesion [11], or displaced bony avulsions, usually warrant acute surgical repair. Operative techniques include but are not limited to transosseous suture repair, midsubstance repair, and more recently, suture anchor repair [8].
Postoperative immobilization is variable among surgeons, without a consensus in the literature on the appropriate method to prevent stress on the repair. Some surgeons prefer splint immobilization alone [6], some apply a cast postoperatively [3], and others advocate supplemental transarticular Kirschner wire pinning of the MP joint [2, 9]. The proposed advantage of temporary pin fixation is increased stability of the MP joint, further protecting the UCL repair during the early phase of healing. Studies testing the biomechanical validity of these postoperative methods of immobilization are lacking.
The goal of this study was to test whether UCL strain is affected by postoperative immobilization techniques in a model of patient noncompliance. During simulated pinch, we hypothesized the UCL would experience significantly lower amounts of strain with supplemental transarticular MP pinning and thumb spica splinting when compared to splinting alone. Without consensus in the literature on how to model pinch in a cadaver model, we simulated pinch through two conditions: (1) valgus force application directly to the thumb and (2) flexor pollicis longus (FPL) loading.
Materials and Methods
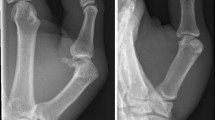
Twelve fresh-frozen human cadaveric specimens were thawed and kept moist with lactated Ringer’s solution at room temperature. Prior to testing, the proximal forearm was mounted to a custom apparatus made of an aluminum bracket and methyl methacrylate polymer. Specimens included the entire hand, extending to the forearm 15 cm proximal to the wrist. Each thawed specimen was examined clinically to ensure no thumb MP UCL instability or prior surgical intervention. Posteroanterior and lateral thumb metacarpophalangeal radiographs demonstrated no significant MP arthrosis. Average specimen age was 51 years (range 35–69 years) with six male and six female specimens.
Dissection was performed along the ulnar aspect of the thumb MP joint. The adductor pollicis aponeurosis was exposed and divided longitudinally to expose the proper UCL. Excess adductor pollicis musculature was debrided to avoid soft tissue impingement with the instrumentation. A micro differential variable reluctance transducer (Microstrain Inc.; Williston, VT) was applied across the central part of the proximal and distal UCL proper (Fig. 1). The native UCL was used in this model to minimize variation introduced with UCL detachment and repair.
The forearm was mounted onto a custom testing frame, and finger traps were applied to the long and ring fingers to maintain the posture of the hand (Fig. 2). The FPL tendon was secured using braided suture (number 2 FiberWire; Arthrex, Inc.; Naples, FL) in a Krackow fashion to a pneumatic loading device, and preconditioning was performed with 15 repetitions of FPL loading corresponding to 2-lb thumb tip pinch force.
With the MP joint held in 10° of flexion, a transarticular 0.045-inch Kirschner wire was applied across the thumb MP joint in a distal radial to proximal ulnar orientation (Fig. 3). The Kirschner wire remained long distally to allow for removal without disturbing the splint. A volar/radial forearm-based plaster (Specialist; BSN Medical, Inc.; Charlotte, NC) thumb spica splint was then applied in the standard postoperative fashion per the senior author, with a varus force applied to the distal thumb. The distal aspect of the splint ended at the base of the thumb nail with a small window in the padding (Webril; Covidien, Inc.; Mansfield, MA) along the ulnar MP joint to allow visualization of the differential variable reluctance transducer (DVRT) device (Fig. 4). No plaster was removed to create the window. Pinch was simulated through two methods: (1) direct valgus load application to the thumb distal phalanx and (2) FPL tendon load application. After splint curing, simulated pinch testing was performed under the two conditions stated in the hypothesis.
Thumb Spica Splint + MP Pin Condition (TSS + Pin)
The initial length of the DVRT device was measured in an unloaded condition. Initial load application through FPL loading versus direct valgus loading was randomized. Forces corresponding to 2, 4, and 6 lb of tip pinch were then applied across the FPL, and each displacement measurement was recorded. Each force was applied four times prior to increasing FPL load. Next, a load cell (S-beam LCCD-25; Omega Engineering Inc.; Stamford, CT) was used to measure up to 2 lb of applied direct valgus force across the ulnar aspect of the distal phalanx. Corresponding displacements at 1 and 2 lb were recorded, and each force was applied four times.
Thumb Spica Splint Condition
Once testing in the TSS + pin condition was complete, the Kirschner wire was removed with the splint intact. The initial length of the DVRT device was reconfirmed, and all load applications were repeated as stated previously.
Prior to testing, a power analysis was performed. A sample size of n = 12 was determined to have an 80 % chance of detecting an effect size of 0.022 strain when controlling type I error at the 0.05 level of significance and using a two-sided test. The effect size selected was based on values reported by Firoozbakhsh et al. [4] in a comparable study of the thumb MP UCL.
Strain values were calculated following data collection. They were analyzed using a repeated measures ANOVA model containing two main effects (splint only vs. pin and splint and load condition). Models with interaction terms were also fit, but the interaction terms were not found to be statistically significant. Therefore, the results presented are based on models with main effects only. When a significant main effect was found for the splint condition, one-way repeated measures ANOVA models were fit for each loading condition. Separate models were fit for FPL and valgus loading. Model assumptions were assessed by evaluating model residuals for normality and plotting them against fitted values. Type I error was controlled at the 0.05 level of significance.
Results
Valgus Load Testing
With direct valgus load application, we noted a significantly lower (p < 0.001) UCL strain in the splint and pin group compared to splint immobilization alone (Table 1). This difference was significant for both the 1- and 2-lb loading conditions (p < 0.05).
Flexor Pollicis Longus Loading Testing
We observed negative displacement for all load conditions with FPL loading, representing shortening of the UCL (Table 2). In addition, the TSS + pin condition resulted in a statistically significant (p < 0.002) greater magnitude of negative strain—there was more UCL shortening with supplemental pin immobilization. Load condition was not found to have a statistically significant effect on UCL strain (p > 0.05).
Discussion
There are no published studies investigating the role of supplemental metacarpophalangeal transarticular pin immobilization after thumb UCL repair. Sollerman et al. [10] compared clinical results of a small group of postoperative patients who received either functional splinting or plaster cast immobilization, concluding equally good results for both groups. Transarticular fixation was not used. Heyman [7] described transarticular pin fixation only in cases with preoperative palmar subluxation or with failed reduction after soft tissue repair. However, many authors describe using transarticular fixation routinely [2, 9]. While transarticular fixation is used in these protocols, this method is anecdotal and has not been verified biomechanically or clinically to help protect UCL repairs.
While we expect most patients to be compliant with postoperative instructions, our study goal was to recreate a situation of noncompliance that may compromise UCL repair. Firoozbakhsh et al. [4] measured native UCL strain with a miniature differential variable reluctance transducer during simulated pinch and grip. Using eight specimens, they found a statistically significant difference between UCL strain values at different levels of tip pinch force at 2, 4, and 6 lb. They concluded that pinch activity should be avoided postoperatively, as it may induce a substantial valgus stress on the ulnar collateral ligament. Adams and Muller [1] investigated UCL strain in different thumb MP positions using a video capture system, concluding that increased flexion leads to greater UCL strain.
Based on these biomechanical studies, we designed our “noncompliant patient” simulated pinch model to induce strain on the UCL in the immobilized thumb. We do recognize the adductor pollicis as an important intrinsic contributor to pinch force. Due to the limitations of intrinsic muscle recruitment in cadaveric specimens, this model consisted of two independent components:
-
1.
Valgus force application: this component of simulated pinch confirmed our hypothesis of decreased UCL strain with supplemental MP pin fixation. As this force applies direct stress across the UCL and is the most common mechanism of UCL injury, it is likely most clinically relevant for evaluating the stress on postoperative immobilization.
-
2.
Flexor pollicis longus loading: based on Adams and Muller’s study [1] demonstrating increased strain with MP flexion, we would expect FPL recruitment to result in greater UCL strain. However, while immobilized, FPL loading paradoxically resulted in negative strain values (shortening of the UCL). During testing, we noted extension of the MP joint during FPL recruitment. As the thumb interphalangeal joint flexed, the distal phalanx would lever against the volar aspect of the splint, causing relative MP extension. This could account for the observed UCL shortening. There was more UCL shortening in the TSS + pin group compared to the group with only TSS. A rotational moment about the oblique orientation of the transarticular pin may result in increased thumb pronation with FPL loading. Another possibility is increased compression across the MP joint with FPL flexion. Both mechanisms could result in relative shortening of the ligament. Clinical relevance is limited by variations in splinting techniques (not immobilizing the IP joint) and the lack of recruitment of intrinsic hand musculature. Regardless of etiology, FPL loading did not jeopardize the UCL in either testing condition.
It is important to note the rationale for testing the TSS + pin group prior to the TSS group. This allowed us to minimize variation in splint application, which could have obscured the observed effect of the supplemental pin. While testing the TSS group second could theoretically result in spuriously elevated displacement values due to splint fatigue, we felt the effect would be nominal when compared to manipulation required for splint removal followed by a second splint application. Additionally, we recalibrated the strain gauges prior to testing the TSS group. Another possible solution was the use of a custom removable thermoplastic splint, but many providers, including the senior authors, do not routinely employ these in the acute postoperative period—representing the most clinically common practice [12]. Using similar logic, we tested native proper ulnar collateral ligaments to avoid variability in repair techniques. A limitation that resulted from using intact ulnar collateral ligaments was the inability to test repaired ligaments to failure. The strain across the ligament and forces applied to the thumb in our study did not approach previously published values of repaired ligament failure [5]. Therefore, while this study demonstrates a statistically significant difference in UCL strain between immobilization methods, it does not address force to failure between immobilization methods. Rather than a single load to failure, another concern is that of fatigue failure of the repair. Future studies could include comparison of strain, load to failure, and the effect of cyclic loading on repaired ligaments between immobilization groups.
While supplemental MP pin fixation does decrease strain across the UCL, possible disadvantages of pin fixation include the following: (1) residual stiffness after pin removal, (2) the risk of pin tract infections or breakage, and (3) articular cartilage damage, particularly in cases with multiple attempted passes. With valgus force application, the thumb MP UCL experiences less strain in the setting of forearm-based thumb spica splinting and transarticular pin fixation, compared to splinting alone. This conclusion provides a foundation to aid clinical decision-making after UCL repair. It reinforces the practice of surgeons who routinely pin their MP joints, but also supports consideration of temporary MP pin fixation in difficult cases, such as those with potential noncompliance or tenuous repair.
References
Adams BD, Muller DL. Assessment of thumb positioning in the treatment of ulnar collateral ligament injuries. A laboratory study. Am J Sports Med. 1996;24(5):672–5.
Baskies MA, Lee SK. Evaluation and treatment of injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Bull NYU Hosp Jt Dis. 2009;67(1):68–74.
Downey DJ, Moneim MS, Omer Jr GE. Acute gamekeeper’s thumb. Quantitative outcome of surgical repair. Am J Sports Med. 1995;23(2):222–6.
Firoozbakhsh K, Yi IS, Moneim MS, et al. A study of ulnar collateral ligament of the thumb metacarpophalangeal joint. Clin Orthop Relat Res. 2002;403:240–7.
Harley BJ, Werner FW, Green JK. A biomechanical modeling of injury, repair, and rehabilitation of ulnar collateral ligament injuries of the thumb. J Hand Surg. 2004;29(5):915–20.
Helm RH. Hand function after injuries to the collateral ligaments of the metacarpophalangeal joint of the thumb. J Hand Surg (Br). 1987;12(2):252–5.
Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5(4):224–9.
Rhee PC, Jones DB, Kakar S. Management of thumb metacarpophalangeal ulnar collateral ligament injuries. J Bone Joint Surg Am. 2012;94(21):2005–12.
Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clin J Sport Med. 2010;20(2):106–12.
Sollerman C, Abrahamsson SO, Lundborg G, et al. Functional splinting versus plaster cast for ruptures of the ulnar collateral ligament of the thumb. A prospective randomized study of 63 cases. Acta Orthop Scand. 1991;62(6):524–6.
Stener B. Displacement of the ruptured ulnar collateral ligament of the metacarpo-phalangeal joint of the thumb. J Bone Joint Surg (Br). 1962;44-B:869–79.
Utz CJ, Lawton JN. Skier’s thumb: repair of acute thumb metacarpophalangeal joint ulnar collateral ligament injury. In: Chung KC, editor. Operative techniques: hand and wrist surgery. 2nd ed. Philadelphia: Elsevier Saunders; 2012.
Conflict of Interest
Jeffrey N. Lawton has received compensation for instrument design consulting for Innomed, Savannah, GA, unrelated to this study, and honoraria from AO North America, also unrelated to this study.
John R. Lien reports no potential conflicts of interest.
Alexander Brunfeldt reports no potential conflicts of interest.
Abhishek Julka reports no potential conflicts of interest.
Richard E. Hughes reports no potential conflicts of interest.
Kagan Ozer reports no potential conflicts of interest.
Statement of Human and Animal Rights
N/A (cadaveric study).
Statement of Informed Consent
N/A (cadaveric study).
Grants or Other External Support
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lien, J.R., Brunfeldt, A., Julka, A. et al. Ulnar collateral ligament strain of the thumb metacarpophalangeal joint: biomechanical comparison of two postoperative immobilization techniques. HAND 10, 721–725 (2015). https://doi.org/10.1007/s11552-015-9747-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-015-9747-x