Abstract
Background
Flexor tendon repair in zone II remains a vexing problem. Repair techniques have been developed to strengthen and optimize the number of core strands crossing a repair. A polyamide looped suture doubles the number of core strands for every needle path. This simplifies repairs, but the knot remains a potential weakness. The purpose of our study was to create a biomechanical model used to evaluate the bulky knot of a looped suture as it may be weaker, resulting in greater deformation.
Methods
Using machined steel rods to hold our suture constructs, we compared four different knot configurations using looped and non-looped sutures in 3-0 and 4-0 varieties using a four-core strand technique. The constructs were tested under increased cyclic loading recording both forces applied and suture construct lengthening (“clinical gapping”) and ultimate breaking strength.
Results
During continuous periods of cyclic loading, we measured permanent deformation and ultimate breaking strength. Permanent deformation results when there is no recoverable change after force removal defined as a permanent rod separation (or gapping) of 2 mm.
Four-strand 3-0 and 4-0 looped sutures failed at 39.9 and 27.1 N faring worse than a four-strand non-looped suture which reached a rod separation of 2 mm at 60.7 and 41.3 N. The ultimate breaking strength demonstrated absolute failure (construct rupture) with the 3-0 looped suture breaking at the knot at 50.3 N and the non-looped suture at 61.5 N. For the 4-0 suture, these values were 32.4 and 41.76 N.
Conclusion
Within the constraints of this model, a looped suture fared worse than a non-looped suture especially when comparing 4-0 and 3-0 sutures. However, two-knot 3-0 looped suture constructs did resist the force generally accepted as occurring with early non-resistive tendon motion protocols, while two-knot 4-0 looped suture constructs did not.
Clinical Relevance
This paper provides a description of a model to evaluate various suture materials and knot strengths in isolation of the tendon itself. This allowed us to evaluate mechanical differences between looped and non-looped sutures for polyamide, which are commonly used in flexor tendon repair. These differences between sutures may impact choices for a suture type selected for these repairs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early motion postoperative therapy protocols have replaced immobilization following a flexor tendon repair to limit the motion restricting adhesion formation and improve function [1, 2]. Active motion improves linear tendon excursion [3] and more rapidly enhances tensile strength at the repair site with fewer adhesions [4]. These protocols place tendon repairs under biomechanical stress sooner in the healing process, thereby demanding structurally superior repair methods.
Two parameters that increase tenorrhaphy strength are the suture material size used in the core stitch and the number of core strands crossing the repair site [5–8]. Newer repair techniques utilize different suture configurations, increased number of strands (core sutures) crossing the repair site, and stronger suture material.
A looped suture has gained popularity for tendon repair since it effectively doubles the strand material per suture pass, thereby reducing the number of core passes to reach the same number of actual core strands crossing the repair site. This simplifies the repair technique and reduces the time taken to obtain an equally strong repair.
However, a relatively unstudied source of potential weakness is the knot itself. Few studies have isolated the knot as the sole variable when evaluating repair strength [9]. Polyamide multifilament sutures are manufactured in double-strand (looped) and single-strand (non-looped) forms available from the same company under similar quality control standards. This suture material can be tested for knot strength in looped and non-looped suture types.
We hypothesize that the four-tailed knot of a looped suture may be weaker, resulting in greater slippage or plastic deformation (cyclic loading to permanent gapping), than a non-looped suture. A potentially weaker knot of a looped suture may result in repaired tendons being unable to undergo postoperative motion protocols. These characteristics might differ in various suture gauges. The question is whether knot characteristics change as more suture material is added to the knot either with the looped suture or with the increasing suture gauge.
The purpose of our study is to compare the biomechanical performance of four-core strand sutures with a suture size of both 3-0 and 4-0 and with four different knot configurations: looped suture with one knot or two knots and non-looped suture with one knot or two knots. In order to isolate the mechanical effects of the repairs, without artifacts due to variations in the suture-tendon interface, we performed this study using incremental cyclic loading of the suture alone under conditions simulating the physiologic environment. This enabled us to establish a model for testing suture material and knot strength in isolation of the tendon-suture interference. It also allowed us to test the impact of looped and non-looped suture materials for polyamide, which have become an increasingly commonly used suture type for tendon repairs.
Materials and Methods
Suture Material
Polyamide multifilament single-strand and looped nylon, non-absorbable suture materials were used, utilizing 3-0 and 4-0 Supramid Extra® II (S. Jackson, Inc., Alexandria, VA) for each knot configuration. Our suture was certified and obtained in a long roll directly from the manufacturer; 3-0 Supramid Extra® II had a nominal diameter of 0.20 mm with a diameter range of 0.200–0.249 mm, and 4-0 Supramid Extra® II had a smaller nominal diameter of 0.15 mm with a diameter range of 0.150–0.199 mm. Both came from the same manufacturing lot ensuring consistency. This was not a company-sponsored research project.
Knot Configurations and Study Groups
Four knot and suture configurations were evaluated using both 3-0 and 4-0 sutures, each having the equivalent of four-core strand sutures crossing the testing gap. These comprised a double-strand looped suture with either one knot or two knots and a single-strand non-looped suture with either one knot or two knots (Fig. 1). The single-strand knots composed of two tails, one each at separate ends. The double-strand knots were created by tying two pairs of separate ends to form a knot composed of four tails.
Illustration of the four different suture constructs. a A looped suture was tied around the two rods and knotted together to form a knot with four tails from two pairs of separate ends. b A single-strand suture was passed around the rods twice and joined from two separate ends. c A looped suture was passed around one rod and tied to another two-strand suture looped around the opposite rod. The knots composed of a pair from one looped suture and a pair from the other looped suture. d A single-strand suture was passed around both rods and tied together. A second single-strand suture was also passed around both rods and then tied together
Experimental Setup
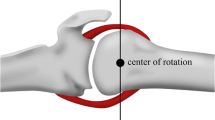
Each construct was produced by tying sutures around the two stainless steel rods (diameter 12.7 mm) separated by two shaft clamps (inner diameter 12.7 mm, outer diameter 25.5 mm), creating a loop of approximately 60.1 mm in length (Fig. 2). “V”-shaped grooves (diameter 9.4 mm) machined into the mid-length of each rod helped secure the suture, preventing lateral migration during testing. Eight pairs of rods were machined. The grooves of each paired rod were aligned and coupled together using elastic bands. All paired rods were then clamped in a vice for knot tying. All knots were tied by an experienced surgeon using four square throws.
Biomechanical tests were performed using a servo-hydraulic testing machine (MTS, Eden Prairie, MN). There were ten in each group of the four constructs and for each of the 3-0 and 4-0 suture sizes (total of 80). All knots were tied and tested on the same day.
The upper rod was attached to the actuator, and the rods were then lowered into a 37 °C saline bath. The lower rod was secured to a custom-made fixture to the base of the bath. The entire bath was fastened to an X-Y table to maintain the alignment of each suture construct during loading. An initial tensile load of 5 N was applied to the coupled rods; the elastic bands were cut, and the rod separation was recorded. The construct was then cyclically loaded at 1 N/s to a peak value of 7 N, which then increased in increments of 2 N in each subsequent loading cycle. After each cycle peak load was reached, the suture construct was unloaded to the 5 N preload and then held for a period of 20 s to allow for recovery. The incremental loading procedure was continued until construct failure occurred, defined as breaking strength. Figure 3 demonstrates a typical testing plot of the load using the MTS crosshead as a function of time. During the loading cycle, relative separation between the two rods and the load creating the rod separation was acquired at sampling of 100 Hz. The plot of the rod separation (or displacement) in response to each load cycle is presented in Fig. 4.
Definition of Terms and Data Analysis
Four different performance criteria were assessed and expressed in terms of the following metrics:
-
1.
Permanent deformation corresponds to the amount of permanent, non-recoverable stretch (or gap) of the suture loop present after relaxation to 5 N. Results corresponding to a permanent deformation of 0.5, 1, 2, and 3 mm were determined for each knot configuration. “Clinical failure” may correspond to a rod separation of 2 mm or a permanent deformation (or gap) of 2 mm. We selected “failure” as an unrecoverable stretch of 2 mm in the construct, since we know that the gap formation at the tendon repair site which is greater than 2 mm is likely to result in motion restricting adhesion formation in the clinical situation.
-
2.
Elongation resistance is the load required to generate a permanent deformation of 0.5, 1, 2, and 3 mm.
-
3.
Ultimate load to failure of a construct is defined as its functional range of stretching from the initial 5 N load to the mechanical failure or rupture of the construct.
Figure 5 shows these graphical metric representations of a typical testing result and illustrates elongation, ultimate load to failure, and permanent deformation (or gapping).
Statistical Analysis
Mean values and standard deviations were calculated for each state. Statistical analyses of the experimental data were performed in SAS (SAS Institute, Chicago, IL) using a one-way analysis of variance (ANOVA). Statistical significance was set at P < 0.05. If the results of the ANOVA test revealed a statistically significant difference between the groups, a post hoc analysis of the data was performed using Fisher’s least significant difference to determine significance.
Results
With regard to clinical failure, we selected a permanent elongation of 2 mm. This results when the properties allowing for recovery of the suture construct have been eliminated, leaving the construct greater than 2 mm of its original length. We attempt to parallel a “gap formation” of 2 mm in the suture constructs to clinical failure following actual tendon repair.
In terms of resistance of each construct to permanent deformation during cyclic loading, the 3-0 suture required larger loads to elongate to 2 mm compared to the 4-0 constructs. The construct with the poorest outcome was a looped suture with two knots for both 3-0 and 4-0 sutures requiring the least force to reach a permanent deformation of 2 mm. On average, this was 39.9 N for the 3-0 suture and 27.1 N for the 4-0 suture. The construct able to withstand the most force before reaching a permanent deformation of 2 mm was produced with one continuous suture strand (non-looped) and one knot for a total of four strands between the rods. With this construct, the average force was 60.7 N for the 3-0 suture and 41.3 N for the 4-0 suture. The differences between each of these two suture constructs for 4-0 and 3-0 were significant with a P value of <0.05 (Fig. 6). A non-looped suture with two knots required only a marginally smaller force to produce a permanent deformation of 2 mm than a non-looped suture with one knot configuration, being 56.9 N for 3-0 and 39.6 N for 4-0. For both 3-0 and 4-0 suture materials, all the non-looped suture constructs required a significantly greater force to produce an elongation of 2 mm than the looped suture constructs.
This is demonstrated graphically in Fig. 7. This is a typical testing run for a 3-0 suture material, comparing all four constructs. Looped suture constructs required lower applied load to reach the clinical failure with a gap of 2 mm or permanent deformation compared to both non-looped constructs. Across all runs, differences between the non-looped constructs were significant when compared against the looped constructs (P < 0.05).
We also evaluated the ultimate breaking strength of suture constructs. Constructs were cyclically advanced until they ruptured, which always occurred at the knot. A looped suture with two knots was the weakest of all, and a looped suture with one knot was the next weakest. By contrast, a non-looped suture with one knot was the strongest and a non-looped suture with two knots was the next strongest (Fig. 8). With the 3-0 suture, the force required to rupture was 50.3 N for a looped suture with two knots and 61.5 N for a non-looped suture with one knot, and it was significantly different (P < 0.0002). The ultimate breaking strength of a 4-0 suture material to rupture was much less for a looped suture with a two-knot construct being only 32.4 N, while for a non-looped suture with one knot, it was 41.8 N (P < 0.0003).
Discussion
Kleinert et al. demonstrated that it was clinically possible to primarily repair flexor tendons in zone II with reasonable outcomes in a region previously called “no man’s land” [10]. They accomplished this by allowing linear excursion of a freshly repaired tendon within the flexor tendon sheath. The motion was controlled, placing minimal tension across the repair site; however, it has been shown experimentally that active mobilization following tendon repair increases the tensile strength of the repair site and further reduces the motion restricting adhesions than the protected motion regimen advocated by Kleinert [1, 2]. Schuind felt that flexor tendon repair techniques were not strong enough to resist disruption during active mobilization postoperatively [11].
Numerous studies have compared the performance of different surgical repair techniques used in flexor tendon repairs [7, 8, 12]. The two important variables that affect the strength of tendon repair are the diameter of the suture and the number of “core strands” crossing the repair site.
Four-strand repairs have been shown to be adequate for zone II flexor tendon repair when utilizing active non-resistive postoperative therapy protocols [1, 2, 7]. In zone II, more complex multistrand repairs become more difficult to accomplish and are bulkier with resultant increased friction and work of flexion within the confines of the flexor tendon sheath [9, 13]. A looped suture is advantageous in that it increases the number of core strands for each suture pass; however, few studies have assessed the strength of the knot, both for gapping at the repair site and absolute breaking strength [6].
For simplicity, yet still simulating what might happen at the tendon repair site, we selected a four-strand suture model. We desired to eliminate the variability that would arise if tendon was present as an added component and so created a biomechanical model in which only the suture material and the knot/knots would be tested. While this model can be used as a generic model to test different types of sutures against each other as well as their knot strength, we selected four-strand constructs and assessed the knot strength of looped and non-looped polyamide sutures with a size of 3-0 and 4-0.
We defined what would determine the equivalent of clinical failure in our model. Clinical and experimental studies have shown in vivo that poor outcomes occur with a gap of 2 mm or greater at the flexor tendon repair site [1, 2, 7, 14, 15]. Our model allowed continuous observation of the gap length responding to cyclic forces applied to suture constructs. This study demonstrated a permanent deformation (or gapping) of each suture loop. Elongation of the suture construct potentially occurred due to a combination of the following three phenomena: elongation of the suture material, knot compaction, and unraveling of the knot. It is difficult to state exactly where the elongation occurred, but in every case, the only variable was the knot. Thus, we conclude that elongation had to result from differences between the knots. Cyclic loading mimics the movement of flexor tendons during rehabilitation. We defined clinical failure as the force required with cyclical loading to achieve an irreversible elongation of 2 mm.
We also determined the load at rupture of each construct. All constructs ruptured at the knot following elongation. Rupture occurred at the knot, at the site where it was twisted for tying and not necessarily due to unraveling. Suture rupture never occurred at a site remote from the knot. The mean force across zone II flexor tendon with normal non-resisted active finger flexion is reported to be about 20 N; following tendon repair, this increases by about 50 % (or 30 N) due to increased friction of the repair and swelling [16, 17]. Others have found that a repair must withstand 35 N when attempting active rehabilitation protocols to prevent failure of the reconstruction [11, 18]. Thus, for the purposes of the discussion, clinical failure might be equated to failure at approximately 30 N.
Our experiments concluded that looped sutures had the weakest knot construct in regard to both failure to resist a gap formation of 2 mm and ultimate breaking strength. If there were two knots in the looped suture, then this was the weakest of all the four constructs. With a 4-0 suture material, a permanent elongation of 2 mm resulted from a force of 27.1 N using a looped suture with two knots, and with a 3-0 suture material, it resulted from a force of 39.9 N using the same construct. However, even with the strongest construct (four non-looped strands with one knot), the 4-0 gapping strength of 2 mm was 41.3 N that is only marginally stronger than the mean tension across a repaired flexor tendon postoperatively with non-resistive active finger flexion. In contrast, for a 3-0 suture with four “repair” strands across the space between the rods but with a non-looped suture and only one knot, the strength was 60.7 N before a 2 mm gap of permanent deformation was attained.
Regarding the ultimate breaking strength for a 4-0 suture material, all constructs using four strands across the space between the rods ranged between 32.4 and 41.8 N, with only the non-looped construct (one knot or two knots) being greater than 40 N. Ultimately, though all constructs with a 3-0 suture material could be loaded to greater than 50 N before breaking, non-looped suture constructs were always stronger than looped constructs.
In conclusion, when four strands cross the gap between the two rods (equivalent to the repair site in a tendon), a 4-0 suture material, irrespective of knot constructs, would probably be unsatisfactory or only marginally able to sustain forces generated for non-resistive active digital motion following tendon repair, both for gapping with cyclical loading and ultimate breaking strength. The two looped suture constructs were less than 35 N for ultimate breaking strength, although both the non-looped constructs exceeded 40 N and so may be able to sustain the forces necessary to avoid breaking during non-resistive active finger flexion at the tendon repair. All the 3-0 suture constructs using four-strands spanning between the rods exceeded an ultimate load of 50 N, but the strength of non-looped sutures exceeded that of looped sutures. With regard to 2 mm gapping, only the two 3-0 non-looped four-strand constructs surpassed 40 N and would probably safely resist the 2 mm gapping during early active finger flexion protocols, being 56.9 and 60.7 N, respectively.
One can speculate as to why the more bulky looped knot and two-knot configurations imparted relative weakness to the overall construct. Since all constructs broke at the knot, one might assume that both the geometry of the knot and the compression of the suture within the knot itself affect the inherent strength of the suture strands. One might also speculate that the more bulky knot of looped sutures may adversely impact in vivo tendon healing by placing more foreign material mass within the space and inhibit collagen healing.
This experiment did not involve repairing tendon ends. There remain other variables to consider, such as the potential effects of suture pullout from the tendon due to the close proximity of the two strands of a looped suture, and this still needs to be evaluated. Within the constraints of this suture testing model, when using a four-strand tendon repair (acknowledging that we do not have the additive benefit of a running peripheral epitendinous suture that would normally be present in an actual tendon repair), one would caution against relying on a 4-0 suture material and would advise caution even with a 3-0 suture material when using a looped suture, especially regarding the potential for gap formation (permanent laxity). The interaction between these suture materials and knot configurations with actual tendon repairs is still in need of further study.
We chose to evaluate the polyamide suture material in our model since it is becoming more commonly used for flexor tendon repairs and because it is available in both looped and non-looped suture types, giving potentially very different knot characteristics. Furthermore, we selected four strands across the repair site (gap between the machined rods) since four core strands have been shown to provide the minimum required strength for tendon repair postoperative motion protocols and it also enabled us to test one- and two-knot constructs. Two-knot constructs are frequently used in tendon repair with one suture strand being placed at the end of each tendon rather than a continuous locking core stitch. Thus, this model and the tested constructs have a number of potential implications including the choice of suture size, the number of knots in the construct, and the looped versus non-looped polyamide suture materials.
References
Savage R, Risitano G. Flexor tendon repair using a “six strand” method of repair and early active mobilisation. J Hand Surg Br Eur. 1989;14(4):396–9.
Trumble TE. Zone-II flexor tendon repair: a randomized prospective trial of active place-and-hold therapy compared with passive motion therapy. J Bone Joint Surg Am. 2010;92(6):1381.
Yalcin L. Biomechanical assessment of suture techniques used for tendon repair. Acta Orthop Traumatol Turc. 2011;45(6):453–7.
Bhatia D, Tanner KE, Bonfield W, Citron ND. Factors affecting the strength of flexor tendon repair. J Hand Surg Br Eur. 1992;17B(5):550–2.
Dogramaci Y, Kalaci A, Sevinç TT, Esen E, Komurcu M, Yanat AN. Does strand configuration and number of purchase points affect the biomechanical behavior of a tendon repair? A biomechanical evaluation using different Kessler methods of flexor tendon repair. Hand. 2008;3(3):266–70.
Rees L, Matthews A, Masouros SD, Bull AMJ, Haywood R. Comparison of 1- and 2-knot, 4-strand, double-modified Kessler tendon repairs in a porcine model. J Hand Surg. 2009;34(4):705–9.
Timothy Thurman R, Trumble TE, Hanel DP, Tencer AF, Kiser PK. Two-, four-, and six-strand zone II flexor tendon repairs: an in situ biomechanical comparison using a cadaver model. J Hand Surg. 1998;23(2):261–5.
Wagner Jr WF, Carroll IV C, Strickland JW, Heck DA, Toombs JP. A biomechanical comparison of techniques of flexor tendon repair. J Hand Surg. 1994;19(6):979–83.
McClellan WT, Schessler MJ, Ruch DS, Levin LS, Goldner RD. A knotless flexor tendon repair technique using a bidirectional barbed suture: an ex vivo comparison of three methods. Plast Reconstr Surg. 2011;128(4):322e–7.
Kleinert H, Kutz J, Ashbell T, Martinez E. Primary repair of lacerated flexor tendons in “no man’s land” (abstract). J Bone Joint Surg. 1967;49A:577.
Schuind F, Garcia-Elias M, Cooney III WP, An K-N. Flexor tendon forces: in vivo measurements. J Hand Surg. 1992;17(2):291–8.
Lee SK. Modern tendon repair techniques. Hand Clin. 2012;28(4):565–70.
Moriya T, Larson MC, Zhao C, An K-N, Amadio PC. The effect of core suture flexor tendon repair techniques on gliding resistance during static cycle motion and load to failure: a human cadaver study. J Hand Surg Eur. 2012;37(4):316–22.
Cao Y, Zhu B, Xie RG, Tang JB. Influence of core suture purchase length on strength of four-strand tendon repairs. J Hand Surg. 2006;31(1):107–12.
Dinopoulos HT, Boyer MI, Burns ME, Gelberman RH, Silva MJ. The resistance of a four- and eight-strand suture technique to gap formation during tensile testing: an experimental study of repaired canine flexor tendons after 10 days of in vivo healing. J Hand Surg. 2000;25(3):489–98.
Strickland J. Flexor tendon injuries. I. Foundations of treatment. J Am Acad Orthop Surg. 1995;3:44–54.
Williamson D, Richards R. Flexor tendon injuries & reconstruction. In: Mathes S, Hentz V, editors. Plastic surgery, the hand & upper limb, vol. 8. 2nd ed. Philadelphia: Saunders/Elsevier; 2006. p. 351–99.
Peltz TS, Haddad R, Scougall PJ, Nicklin S, Gianoutsos MP, Walsh WR. Influence of locking stitch size in a four-strand cross-locked cruciate flexor tendon repair. J Hand Surg. 2011;36(3):450–5.
Conflict of Interest
David T. Netscher declares that he has no conflict of interest to disclose in regards to this paper.
Justin J. Badal declares that he has no conflict of interest to disclose in regards to this paper.
Jonathan Yang declares that he has no conflict of interest to disclose in regards to this paper.
Yoav Kaufman declares that he has no conflict of interest to disclose in regards to this paper.
Jerry Alexander declares that he has no conflict of interest to disclose in regards to this paper.
Philip Noble declares that he has no conflict of interest to disclose in regards to this paper.
Statement of Human and Animal Rights
We, undersign, certify that the procedures and the experiments performed respect the ethical standards in the Helsinki Declaration of 1975, as revised in 2000 [5], as well as the national law.
Statement of Informed Consent
As there were no human subjects involved in this study, no informed consent was obtained or necessary.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Netscher, D.T., Badal, J.J., Yang, J. et al. Biomechanical evaluation of double-strand (looped) and single-strand polyamide multifilament suture: influence of knot and suture size. HAND 10, 417–424 (2015). https://doi.org/10.1007/s11552-014-9723-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9723-x