Abstract
Background
The purpose of this study was to explore and evaluate national trends and factors contributing to pediatric wrist fractures.
Methods
Over a 16-year period from January 1998 to December 2013, we identified and reviewed patients aged 0–17 years old with the primary diagnosis of wrist fracture, as evaluated in US EDs and chronicled by the National Electronic Injury Surveillance System (NEISS) database of the US Consumer Product Safety Commission. We conducted descriptive epidemiologic, bivariate, and chi-square analyses. Patients were categorized into age-defined subgroups and further stratified by sex, race, location, and consumer product/activity associated with injury.
Results
There were 53,265 children evaluated in NEISS EDs (national estimate, 1,908,904) with wrist fractures from 1998 to 2013. Mean age was 10.9 years, with 64 % males and 36 % females. The most common locations of injury were place of recreation/sports, home, and school. The top five consumer-product-related injuries were associated with bicycles, football, playground activities, basketball, and soccer. The highest subgroup associations were with beds (0–12 months), stairs (13–36 months), playgrounds (3–5 and 6–10 years), and football (11–17 years). The greatest increase in fractures occurred between ages 0–12 and 13–36 months, with the second-largest increase between ages 3–5 and 6–10.
Conclusions
It is essential to develop injury prevention and safety strategies as well as identify individual risk factors for fracture, including activity, sex, and key age transitions. Surveillance is imperative to advance our understanding of these fractures, and in the future may facilitate development of research prediction tools to anticipate or prevent injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In childhood, trauma to the distal aspect of the upper extremity is frequent, and pediatric wrist fractures (including distal radius, ulna, and carpal bones) are commonly seen in the emergency department (ED). Knowledge of the epidemiology of fractures is valuable to development of safety and prevention strategies. Cheng et al. [3] studied limb fracture patterns in 3,350 children at one center from 1986 to 1990 and determined that the most common fracture was the distal radius (almost 20 %).
Researching the conditions surrounding pediatric wrist trauma is important to preventing and anticipating injuries. Epidemiologic analyses provide us with knowledge regarding which specific age groups are at higher risk for fracture. They help identify hazardous environments, unsafe activities, and other wrist injury risk factors. Once recognized, specific actions can be developed to improve health and well-being. There have been few population-based studies on pediatric wrist fractures, and those that have been performed have been limited to a few emergency department settings, non-US countries, or only analyzed trends over limited time periods [4, 6, 11]. To our knowledge, this is the first nationally representative epidemiologic study of pediatric wrist fractures in US emergency departments.
In order to gain a nationally accurate and clearer understanding of the epidemiologic dynamics behind pediatric wrist fractures, we elected to study ED visits across the USA over a recent, extended time period, in order to analyze trends for these injuries. Several factors may play a role in determining risk for fracture in children and adolescents, including environment or surroundings, age, sex, race, activity, and time of year. The purpose of this study was to explore and evaluate US epidemiologic trends and factors contributing to wrist fractures in children over the past 16 years.
Materials and Methods
National Electronic Injury Surveillance System
The United States Consumer Product Safety Commission (CPSC) maintains a national probability sample of hospitals in the US termed National Electronic Injury Surveillance System (NEISS). Each NEISS-designated hospital collects patient information for every emergency visit involving an injury. There are approximately 100 hospitals selected as a probability sample of the more than 5,000 US hospitals. Each of these hospitals has a 24-hour ED with at least six beds, with trained NEISS coordinators extracting pertinent data from ED records and transcribing them into coded form using rules described in a NEISS Coding Manual [9, 12]. Each case is assigned one or two CPSC-specific product codes [9] that designate what products or activities were involved at the time of injury. From this sampling of hospitals, the national total number of injuries treated in hospital EDs can be estimated. This is performed by totaling the number of cases from all NEISS EDs and then using a weighted multiplier based on the size of the hospital and the number of hospitals similarly sized across the country.
Utilization of NEISS
The NEISS database [13] was queried for all pediatric wrist fractures (with body part designated as wrist, diagnosis as fracture, and age 1 month to 17 years) from January 1, 1998 to December 31, 2013. We did not incorporate data prior to 1998 as CPSC updated the NEISS sample to reflect the current distribution of US hospitals in 1997. In addition, earlier years did not contain expanded information, including injuries where no product was mentioned (for example, a fall on the ground) and injuries related to products not collected (such as motor vehicle collisions). In the current distribution, four fifths of these hospitals represent hospital EDs of differing sizes, and one fifth represent EDs from children’s hospitals. The NEISS data set provided patient age, sex, race/ethnicity, incident locale (school, place of recreation, home, public property, or street or highway), disposition, product code associated with injury, and a brief narrative description of the incident. Data from all NEISS hospitals were included. With the goal of analyzing wrist fractures in the pediatric population, we excluded all patients who did not fulfill our aforementioned criteria.
We categorized patients into age-defined subgroups (0–12 months, 13–36 months, 3–5 years, 6–10 years, and 11–17 years), and further stratified the groups with regard to sex, race, location, and consumer product/activity associated with injury. As the ages per group varied, we standardized the cases by dividing the total number of wrist fractures per age group by the total number of different ages per subgroup (e.g., 0–12 months divided by 1, 13–36 months divided by 2, 3–5 years divided by 3). We then calculated national estimates of pediatric wrist fractures by multiplying the number of cases by an averaged conversion factor (provided by NEISS) that was associated with each subgroup. We also used provided dates of injury (data only available for 2013) to group patients into months in order to determine if there was any seasonal variation in incidence. We defined spring as beginning on March 1, summer on June 1, autumn on September 1, and winter on December 1. Subsequently, we also calculated national estimates for the number of fractures per season.
Data Analysis
We performed descriptive statistical analysis, facilitated by the use of conventional mathematical software. We obtained Pearson’s correlation coefficient to quantify the correlation between each individual age group to the entire cohort frequency trended throughout the 16-year period. We used a chi-squared test to determine if there is a significant difference in frequency distribution between sexes of each age subgroup.
Results
There were 53,265 children evaluated in NEISS EDs (national estimate, 1,908,904) with wrist fractures during the 16-year timespan from 1998 to 2013. Mean age was 10.9 (SD 3.8) years, with 64 % males and 36 % females. The top consumer-product-related injuries were associated with bicycles (10 %), football (8 %), playground activities (8 %), basketball (6 %), and soccer (5 %) (Table 1). The highest number of total wrist fractures took place in the years 2000 (7.2 %), 2001 (7.2 %), and 2002 (7.2 %), and the lowest in 2013 (4.5 %) and 2012 (4.7 %). The race distribution and most common locations of injury were as described in Tables 2 and 3, respectively. Concerning disposition, 97 % of pediatric patients were treated and released, or examined and released without treatment. One percent were treated and transferred to other hospitals, and 2 % were treated and admitted for hospitalization.
The highest associations by age subgroup were as described in Table 4. In the 0–12-months group, 69 % of injuries were located at home, with another 27 % with location not recorded. In contrast, only 15 % of injuries in the age 11–17-years group were located at home, with 35 % occurring at place of recreation or sports, 14 % at school, and 27 % at an unspecified location. Race appeared consistent throughout the stratified groups; however, it was often unrecorded.
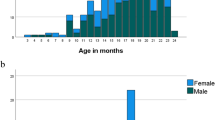
When examining 16-year trends for the top five product codes (Fig. 1), there has been a decline in the number of bicycle- and basketball-related wrist fractures, while there has been a rise in soccer-related wrist fractures. Football-related wrist fractures displayed an upwards trend, with a decline in recent years. Playground-related wrist fractures have remained relatively unchanged overall. With each increase in subgroup age, up to 6–10 years, there is an increase in the number of fractures, irrespective of the year (Fig. 2). There was not a statistically significant difference in number of wrist fractures between the 6–10- and 11–17-years subgroups.
The greatest increase in fractures occurred between ages 0–12 and 13–36 months (1:3.8), with the second-largest increase between ages 3–5 and 6–10 years (1:2.2). There was a disproportionately higher number of females sustaining fractures in all groups under age 11, with a higher number of males in the 11–17 group (18 %, p < 0.05). Only the 2013 NEISS data contained specific dates of injury, and we used this information to calculate national estimates for each season. We noted that seasonal variations in frequency did occur, with the fewest pediatric wrist fractures in the winter months (Table 5).
Discussion
It is essential to develop injury prevention and safety strategies as well as identify individual risk factors for fracture, including activity, sex, and key age transitions. Based on population trends, it appears that as children age they are at higher risk for sustaining wrist fractures, until approximately age 10. The age 11–17 subgroup displayed similar numbers of wrist fractures when standardized and compared with the age 6–10 subgroup. There are similarities with respect to the types of activities resulting in wrist fracture for the 6–10 and 11–17 age subgroups, with 6 of the top 10 product/activity codes being the same (see Tables 6 and 7).
Previous population-based assessments have shown that the incidence of pediatric upper extremity fractures is increasing. It has been suggested that the increase is due to increasing sports participation and/or body weight [6, 15]. In 2003, Khosla et al. [6] conducted a population study in Rochester, Minnesota, and found a statistically significant increase in the incidence of distal forearm fractures in children and adolescents over the past 30 years. In 2010, Ryan et al. [11] studied the epidemiology of pediatric forearm fractures in Washington, D.C., by evaluating patients seen at an urban pediatric ED, and implicated falls from monkey bars and minor trauma in the majority of fractures. A 2011 study in the Netherlands by de Putter et al. [4] examined trends in children and adolescents from 1997 to 2009, utilizing ED visit data from the Dutch Injury Surveillance System (15 geographically distributed hospitals). They found a considerable number of pediatric wrist fractures attributable to sports (soccer and gymnastics at school), with the strongest increase in the age group 10 to 14 years.
Earlier studies have proposed that the differences in fractures across pediatric age groups are due to variable individual and lifestyle factors. One study [14] indicated that with increasing age, the male/female ratio and time spent in sports participation increased, while calcium intake and time spent in sedentary behaviors decreased. There are many variables to consider when determining what factors contribute to pediatric wrist fractures, including elements influencing bone strength as well as the susceptibility of the bone to outside mechanical stresses.
Previous studies [1, 7, 8] have found that the incidence of distal forearm fractures in children reaches a peak at or about the time of the pubertal growth spurt. One explanation for this observation is a transient increase in cortical porosity, resulting from increased bone turnover due to increased calcium demands at the time of greatest longitudinal bone growth [10]. Peak bone mass accumulation lags behind peak bone length. The dissociation of these growth curves may present an interval of susceptibility to the mechanical challenges of activities such as high impact sports.
High impact sports (such as football, soccer) appear nationally to be highly associated with pediatric wrist fractures. With increasing involvement in these sports, it is essential to develop injury prevention and safety strategies as well as to identify individual risk factors for fracture. Bicycle-related wrist fractures have declined, which may be secondary to public education and legislative efforts to promote protective equipment such as helmets and extremity pads/guards. Another reason could be declining popularity in the sport of bicycling.
The decrease in basketball- and football-related wrist fractures likely result from a combination of advances in education and training/injury prevention techniques, innovative protective equipment, and sporting rule changes designed to reduce injury. It is unclear why soccer-related wrist fractures are rising. Hedström, et al. [5] noted an increase in overall fractures due to soccer in Swedish males and females aged 10 years or more, and believed that the increase is due to higher participation in organized soccer. The increase may be due to rising popularity of the sport in the USA. Information is not available regarding how many of these children play the goalkeeper position and may have sustained wrist fractures in the act of “saving the ball,” as has been reported in literature [2].
The increase seen at age 5 may be attributable to transitioning to school, while the increase at 12 months may be ascribed to learning to ambulate. Conceivably, those age groups may benefit from increased supervision. The sex difference in the oldest age group may be associated with popularity of high impact sports with males, and similar differences were seen in epidemiologic studies based in non-US countries. It is unknown why there is a disproportionate difference in females sustaining wrist fractures in all subgroups under age 11. Due to the number of confounding variables, further investigation is necessary to identify the underlying causes. These include differences in patterns of physical activity, nutrition, calcium and vitamin D intake, or genetic disparities. Perhaps there is a role for sex-specific injury prevention strategy. Finally, the difference in fractures between summer and winter months (2013 data) may be a consequence of time off from school to participate in activities or the weather itself being an impediment to outdoor play.
Limitations of the study include limitations of the database itself. The foundation of the national database is contingent upon ED surveillance data, which is dependent on NEISS hospital coordinator reviews of ED records and selection of those that meet inclusion criteria. In the database, all wrist fracture diagnoses are bundled together. We do not know how many of these were distal radius fractures and how many were scaphoid or other carpal bone fractures. The fractures are not classified, and level of injury is not indicated (e.g., high-energy fractures requiring reduction versus nondisplaced fractures immobilized in a splint or cast). Another limitation is that this study only analyzed those pediatric patients who presented to the ED with wrist fractures. This excludes patients who may have visited an urgent care facility or visited directly with their primary care providers or hand and wrist specialists. In addition, the NEISS database does not include any specific geographic data regarding these fractures. Having this information would help contribute to our knowledge database and potentially target prevention strategies to high-risk regions of the country. The NEISS database only began to collect specific dates of injury in 2013. We cannot definitively generalize our conclusions regarding the seasonal variation in fractures until more years of data are collected. Additionally, we do not have data available regarding bone mineral density or calcium/vitamin D intake. These factors play a role in the strength of the bone and resistance to plastic deformation or fracture.
Future investigations are needed to independently corroborate our findings and minimize information bias. A future study would benefit from incorporation of data from other national databases. Despite the limitations, the NEISS data set provides a nationally representative stratified probability sample of pediatric wrist fractures in the USA. The results of the study have outlined many of the risk factors in the overall pediatric population. They have also identified differences in subgroups based on age, sex, and activity. Now that we have characterized the disparities, specific investigative studies can be performed as to the underlying causes for these wrist fractures. In addition, with new yearly data, the trends can be monitored for further patterns and the success of prevention techniques can be analyzed. Surveillance is imperative to advance our understanding of the epidemiologic basis for wrist fractures in children, and in the future may facilitate development of research prediction tools to help anticipate or prevent injury.
References
Bailey DA, Wedge JH, McCulloch RG, et al. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71(8):1225–31.
Boyd KT, Brownson P, Hunter JB. Distal radial fractures in young goalkeepers: a case for an appropriately sized soccer ball. Br J Sports Med. 2001;35(6):409–11.
Cheng JCY, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma. 1993;7(1):15–22.
De Putter CE, van Beeck EF, Looman CWN, et al. Trends in wrist fractures in children and adolescents, 1997–2009. J Hand Surg [Am]. 2011;36(11):1810–5. doi:10.1016/j.jhsa.2011.08.006.
Hedström EM, Svensson O, Bergström U, et al. Epidemiology of fractures in children and adolescents: Increased incidence over the past decade: a population-based study from northern Sweden. Acta Orthop. 2010;81(1):148–53.
Khosla S, Melton III LJ, Dekutoski MB, et al. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290(11):1479–85.
Kramhoft M, Bodtker S. Epidemiology of distal forearm fractures in Danish children. Acta Orthop. 1988;59(5):557–9.
Landin LA. Fracture patterns in children: analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop. 1983;54(S202):3–109.
NEISS Coding Manual. U.S. Consumer Product Safety Commission. January 2014. http://www.cpsc.gov/Neiss/completemanual.pdf. Accessed June 24, 2014.
Parfitt AM. The two faces of growth: benefits and risks to bone integrity. Osteoporos Int. 1994;4(6):382–98.
Ryan LM, Teach SJ, Searcy K, et al. Epidemiology of pediatric forearm fractures in Washington, DC. J Trauma Acute Care Surg. 2010;69(4):S200–5.
Schroeder T, Ault K. The NEISS sample (design and implementation) 1997 to present. Bethesda: Division of Hazard and Injury Data Systems, US Consumer Product Safety Commission; 2001.
U.S. Consumer Product Safety Commission NEISS Estimates Query Builder Web Site. https://www.cpsc.gov/cgibin/NEISSQuery/home.aspx. Accessed May 20, 2014.
Valerio G, Gallè F, Mancusi C, et al. Pattern of fractures across pediatric age groups: analysis of individual and lifestyle factors. BMC Public Health. 2010;10(1):656.
Williams AA, Lochner HV. Pediatric hand and wrist injuries. Curr Rev Musculoskelet Med. 2013;6(1):18–25.
Conflict of Interest
Neil S. Shah has no conflict of interest.
David Buzas has no conflict of interest.
Ephraim M. Zinberg has no conflict of interest.
Statement of Human and Animal Rights
This article does not contain experimental studies with human or animal subjects.
Statement of Informed Consent
All data from the study were de-identified to ensure anonymity.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shah, N.S., Buzas, D. & Zinberg, E.M. Epidemiologic dynamics contributing to pediatric wrist fractures in the United States. HAND 10, 266–271 (2015). https://doi.org/10.1007/s11552-014-9710-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9710-2