Abstract
Background
With progressive lunate collapse, salvage procedures in advanced Kienbock disease attempt to provide pain relief and maintain motion. Scaphocapitate arthrodesis may provide a durable option with comparable outcomes to proximal row carpectomy in the well-selected patient.
Methods
We performed a retrospective chart review of all consecutive patients with Lichtman stage IIIA or IIIB Kienbock’s disease who underwent either scaphocapitate or scaphotrapeziotrapezoid-capitate arthrodesis from January 2004 to December 2013.
Results
Twelve patients were included with a mean age of 41.6 years. Ten patients underwent scaphocapitate arthrodesis, while two patients underwent scaphotrapezio-trapezoid-capitate arthrodesis with an average clinical follow-up of 13.1 months. All patients achieved fusion. The average postoperative flexion-extension arc was 53° (range 20–110°). The average ulnar deviation was 9° (range 5–15°), and the average radial deviation was 13° (range 5–25°). Postoperative pain scores were significantly improved, having changed from an average of 6.6 preoperatively to 2.8 on a 10-point scale (W = 18, P < 0.05).
Conclusions
Despite a mean flexion-extension arc that is reduced from that of a normal individual, the postoperative range of motion following a midcarpal arthrodesis was not significantly different than that reported in a recent systematic review of proximal row carpectomy (73.5° compared with 53°, respectively) (P = 0.05). Additionally, given the significant postoperative reduction in associated pain symptoms at the time of follow-up, scaphocapitate arthrodesis should be considered as a treatment option for wrist salvage in the patient with advanced Kienbock’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salvage options following progressive collapse and fragmentation of the lunate in the setting of Kienbock’s disease are based on preservation of the existing carpal alignment and radiocarpal articulation through excision of the failing proximal row, or midcarpal fusions that maintain or improve the scaphoid posture [9, 12]. Scaphocapitate (SC) arthrodesis is a less well-described procedure when compared to proximal row carpectomy (PRC); however, advocates have cited the benefits of the maintenance of existing carpal height, relative preservation of normal radioscaphoid articulation, and the potential offloading of the lunate (Table 1).
Despite the popularity of PRC for salvage options in a various traumatic or degenerative diseases of the wrist, opponents of the technique have cited the limited lifespan of the radiocapitate articulation, with eventual eburnation, return of pain, and the need for wrist fusion. And as Kienbock’s disease typically affects young adults, the relative advantage of a procedure that maintains the normal radioscaphoid articulation is unclear. DiDonna et al. analyzed a series of 22 wrists in 21 patients undergoing proximal row carpectomy and found that two of the four failures were in younger patients with Kienbock’s disease [4]. In a series of 81 patients with PRC with 61 available for follow-up by Ali et al., 74 % (46 patients) were not satisfied with the results of their surgery [1]. The study cohort included 52 % manual laborers and 16 % of the patients had a diagnosis of Kienbock’s disease.
There are very few published reports on the results of scaphocapitate fusion for the treatment of advanced Kienbock’s disease [8, 13]. We retrospectively reviewed our experience with scaphocapitate arthrodesis in the setting of advanced Kienbock’s disease. Additionally, we compared these results with the available literature on scaphocapitate arthrodesis and proximal row carpectomy to better understand the potential benefits of each salvage choice and increase the available evidence for both the practitioner and patient when deciding between these treatment options and discussing expected surgical outcomes.
Methods
Following Institutional Review Board (IRB) approval, we performed a retrospective chart review of all consecutive patients with Lichtman stage IIIA or IIIB Kienbock’s disease who underwent either SC arthrodesis or scaphotrapeziotrapezoid-capitate (STT-C) arthrodesis at our institution from January 2004 to December 2013 (Fig. 1). Chart review included postoperative follow-up clinic visit documentation as well as operative reports and radiographic analysis. A 10-point Visual Analogue Scale was documented by the surgeon at the pre- and postoperative clinic visits, and these were compared preoperatively and postoperatively using a Wilcoxon signed-rank test.
Surgical Technique
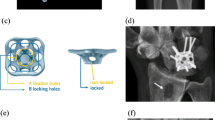
Following a longitudinal incision between the second and fourth dorsal compartments, a standard ligament sparing capsulotomy was performed. The scaphocapitate articulation was exposed, and any remaining articular cartilage was removed with curettes, curved osteotomes, and a surgical burr. In instances of progressive scaphoid flexion, a 1.5 mm Kirschner wire was placed as a joystick in the scaphoid and used to extend the scaphoid and correct any palmar flexion deformity, with an ideal radioscaphoid angle of approximately 45° (30–57°) [10]. Following this, another 1.5 mm Kirschner wire was utilized for provisional fixation of the scaphocapitate joint. In nine patients, a headless, cannulated compression screw (Acumed, Hillsboro, Oregon; Synthes, West Chester, Pennsylvania) was placed across the SC arthrodesis (Fig. 2). One SC arthrodesis was performed using only Kirschner wires. Of the two STT-C arthrodesis patients, one patient underwent STT-C fusion with Kirschner wires, and the other was completed with a small circular plate (Integra, Plainsboro, New Jersey).
1-year postoperative posteroanterior (left) and lateral (right) radiographs of the patient from Fig. 1, following midcarpal arthrodesis with two cannulated headless screws. Note the preservation of the radiocarpal joint height and improved scaphoid posture
Result
Ten patients underwent SC arthrodesis, while two patients underwent STT-C fusion, for a total of 12 patients. There were five women and seven men with a mean age of 41.6 years. The average follow-up time was 392 days with a range from 88 to 2308 days. In two patients, the lunate was fragmented and removal was performed. In conjunction with the original operation, one patient underwent a cubital tunnel release, one had a carpal tunnel release, and one patient had a concomitant arthroscopic triangular fibrocartilage complex debridement.
Two patients developed symptoms consistent with chronic regional pain syndrome (CRPS) within 100 days of follow-up and were required to undergo aggressive hand therapy and desensitization modalities. One patient underwent a dorsal capsulotomy for persistent wrist stiffness with restricted wrist flexion capability that was bothersome to the patient at 10 months after the initial surgery, with improvement of wrist flexion and extension.
The average postoperative flexion-extension arc across the 12 patients was 53° (range 20–110°). The average postoperative flexion was 22° (range 10–35°), and the average postoperative extension was 31° (98 range 10–55°). The average ulnar deviation was 9° (range 5–15°), and the average radial deviation was 13° (range 5–25°). Using a Wilcoxon signed-rank test, there was a significant difference in the visual analog pain scores between pre- and postoperatively, with the average preoperative pain score 6.6 while the average postoperative pain score at final follow-up was 2.8 (W = 18, p < 0.05). All patients had radiographic union of the scaphocapitate fusion, with an average time to union of 14 weeks (range of 7–23 weeks).
Discussion
Originally described by Sutro [15] and Helfet [5] for the management of scaphoid nonunion, Pisano et al. described SC arthrodesis for Kienbock’s disease in 1991 [11]. As progressive collapse and fragmentation of the lunate is thought to result from excessive force across the lunate, the goal of the fusion is to unload the lunate and delay the development of further radiocarpal and midcarpal arthritis. Biomechanical studies have suggested that SC arthrodesis decreases force across the radiolunate and lunocapitate articulations while resulting in increased joint force across the radioscaphoid joint [7, 16, 17].
More recently, Luegmair described substantial pain relief in five patients with stages IIIB and IV Kienbock’s disease managed with SC arthrodesis, at an average follow-up of 8.75 years [8]. They reported a postoperative flexion-extension arc of 84° and radial-ulnar deviation arc of 41° in patients with stage IIIB–IV Kienbock’s disease managed with SC arthrodesis. Sennwald et al. also reported on ten patients with stage III Kienbock’s disease who underwent SC fusion with pain relief reported in 90 % of patients at an average follow-up of 36 months [13].
In the current study, we had complete radiographic union in all our patients, at a mean of 14 weeks with significant improvements in pain score. There were two cases of CRPS that resolved with therapy and one case of stiffness requiring wrist capsulotomy. At the time of final follow-up, there were no failures requiring revision surgery or conversion to a total wrist fusion.
In our cohort, the mean wrist flexion-extension arc was 53°, with 20° flexion and 33° extension. Brumfield and Champoux studied 19 normal adults with a uniaxial electrogoniometer in order to determine the wrist range of motion in order to complete 15 activities of daily living (ADLs) and found that the necessary wrist motion to accomplish these activities was with a flexion/extension arc of 45° (10° of flexion to 35° of extension) [2]. Our results suggest that SC fusion for Kienbock’s disease is a procedure with a low complication rate that allows preservation of a functional range of motion in the wrist in order to perform ADLs.
A gold standard surgical treatment for advanced Kienbock’s disease has not been established. Innes et al. conducted a systemic review of multiple treatment options for late Kienbock’s disease and found that subjective pain improved regardless of treatment type and that range of motion improved significantly in all groups except nonsurgical treatment and partial arthrodesis [6]. Proximal row carpectomy (PRC) is a well-established technique for managing advanced wrist arthritis, including advanced Kienbock’s disease. In 2012, Chim et al. performed a systematic review of the available literature on long-term outcomes following proximal row carpectomy [3]. In a total of six articles with 147 patients, the average weighted postoperative range of motion was 73.5° of flexion/extension arc and 31.5° radial/ulnar deviation. These results were comparable to the postoperative range of motion in Luegmair’s SC arthrodesis study, whereas our results demonstrated a relative decrease in total range of motion following fusion [8]. However, Chim et al. cautioned that PRC may be best suited for individuals greater than 35 years old and involved in less demanding activities as they found the majority of their failures in patients under 35 years of age and involved in an active occupation. Of the 147 patients in the six included studies in Chim’s analysis, there were a total of 21 failures (14.3 %) that required reoperation, and these failures were evenly divided among a range of wrist pathology that included Kienbock’s disease. Of the six included studies, the study with the greatest subset of patients with poor results also had the greatest proportion of patients involved in manual labor (76.5 %), suggesting that patients involved in demanding labor postoperatively may have the worst outcomes following PRC [1]. At the conclusion of their analysis, the authors recommend PRC as best suited for patients greater than 35 years old and involved in less demanding activities. Similar findings were reported by DiDonna et al. with two of their four failures in patients with Kienbock’s disease [4]. The authors recommended against PRC for patients younger than the age of 35 years.
With regard to the limitations of our study, this was a retrospective study looking at short-term follow-up of patients undergoing scaphocapitate for advanced Kienbock’s disease. We had limited preoperative data on wrist range of motion that would have been helpful to compare to our postoperative range of motion. Furthermore, pre- and postoperative data on grip strength would be beneficial to see if our findings correlated with other published reports on SC arthrodesis and PRC. Additionally, some reports have identified an increased rate of radioscaphoid arthritis following SC fusion as Luegmair et al. identified a rate of secondary radioscaphoid osteoarthritis at 50 % in ten patients at a mean follow-up of 8.75 years [8]. As such, the potential for delayed radioscaphoid arthritis in our cohort with more long-term follow-up is possible.
Kienbock’s disease is one of low prevalence with a poorly defined treatment algorithm, and surgeons may base management decisions on small reported series such as ours due to the lack of treatment consensus [14]. Our study does not suggest that scaphocapitate arthrodesis is the proper treatment for all cases of advanced Kienbock’s disease, but rather our results suggest that scaphocapitate arthrodesis is a reasonable alternative to proximal row carpectomy as a salvage procedure in patients with advanced Kienbock’s disease that provides pain relief and functional range of motion. Further investigations should include long-term outcomes of patients with scaphocapitate arthrodesis for treatment of Kienbock’s disease as well as grip strength measurements and patient reported outcome questionnaires. There is a paucity of literature on functional outcomes of scaphocapitate fusion, compared to the published reports on proximal row carpectomy, and other midcarpal fusions such as four-corner fusions, capitolunate fusions, and scaphotrapeziotrapezoid fusions.
References
Ali MH, Rizzo M, Shin AY, Moral SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (NY). 2012;7(1):72–8.
Brumfield RH, Champoux J. A biomechical study of normal function wrist motion. Clin Orthop Relat Res. 1984;187:23–5.
Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a systematic review of the literature. J Wrist Surg. 2012;1(2):141–8.
DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: Study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86-A(11):2359–65.
Helfet AJ. A new operation for ununited fracture of the scaphoid. J Bone Joint Surg. 1952;34B:329.
Innes L, Strauch RJ. Systematic review of the treatment of Kienböck’s disease in its early and late stages. J Hand Surg Am. Elsevier Inc. 2010;35(5):713–717.e1-4.
Iwasaki N, Genda E, Barrance PJ, et al. Biomechical analysis of limited intercarpal 201 fusion for the treatment of Kienbock’s disease: a three-dimensional theoretical study. J Orthop Res. 1998;16(2):256–63.
Luegmair M, Saffar P. Scaphocapitate arthrodesis for treatment of late stage Kienbock disease. J Hand Surg Eur. 2014;39(4):416–22.
Lutsky K, Beredjiklian PK. Kienböck disease. J Hand Surg [Am]. 2012;37(9):1942–52.
Minamikawa Y, Peimer CA, Yamaguchi T, et al. Ideal scaphoid angle for intercarpal arthrodesis. J Hand Surg [Am]. 1992;17:370–5.
Pisano SM, Peimer CA, Wheeler DR, et al. Scaphocapitate intercarpal arthrodesis. J Hand Surg Am. 1991;16(2):328–33.
Schuind F, Eslami S, Ledoux P. Kienbock’s disease. J Bone Joint Surg (Br). 2008;90(2):133–9.
Sennwald GR, Ufenast H. Scaphocapitate arthrodesis for the treatment of Kienböck’s disease. J Hand Surg [Am]. 1995;20(3):506–10.
Squitieri L, Petruska E, Chung KC. Publication bias in Kienböck’s disease: systematic review. J Hand Surg Am. Elsevier Inc. 2010;35(3):359–367.e5.
Sutro CJ. Treatment of nonunion of the carpal navicular bone. Surgery. 1946;20:536–40.
Viegas SF, Patterson RM, Peterson PD, et al. Evaluation of the biomechanical 198 efficacy of limited intercarpal fusions for the treatment of scapho-lunate dissociation. J Hand Surg Am. 1990;15(1):120–8.
Young Szalay MD, Peimer CA. Scaphocapitate arthrodesis. Tech Hand Upper Extrem Surg. 2002;6(2):56–60.
Delétang F, Segret J, Dap F, Dautel G. Chronic scapholunate instability treated by scaphocapitate fusion: a midterm outcome perspective. 2011;97(2):164–71.
Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995;20(6):965–70.
Imbriglia JE, Broudy AS, Hagberg WC, McKernan D. Proximal row carpectomy: clinical evaluation. J Hand Surg Am. 1990;15(3):426–30.
Conflict of Interest
Matthew L. Iorio declares that he has no conflict of interest.
Colin D. Kennedy declares that he has no conflict of interest.
Jerry I. Huang declares that he has no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee onhuman experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study and from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Iorio, M.L., Kennedy, C.D. & Huang, J.I. Limited intercarpal fusion as a salvage procedure for advanced Kienbock disease. HAND 10, 472–476 (2015). https://doi.org/10.1007/s11552-014-9705-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9705-z