Abstract
Background
Disorders involving the peripheral nervous system can have devastating impacts on patients’ daily functions and routines. There is a lack of consideration of the impact of injury on social/emotional well-being and function.
Methods
We performed a retrospective database and chart review of adult patients presenting between 2010 and 2012 with peripheral nerve compression, brachial plexus injury, thoracic outlet syndrome (TOS), or neuromas. At the initial assessment, patients completed a questionnaire used to obtain demographic and psychosocial variable data including the (1) average level of pain over the last month, (2) self-perceived depression, (3) how much pain impacts quality of life (QoL), (4) current level of stress, and (5) ability to cope with stress. Statistical analyses were used to assess the differences between the dependent variables and diagnostic and demographic groups.
Results
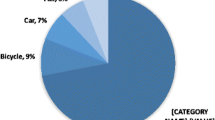
This study included 490 patients (mean age 50 ± 15 years); the most common diagnosis was single nerve compression (n = 171). Impact on QoL was significantly greater in patients with TOS, cutaneous peroneal compressions, and neuroma versus single site nerve compressions. Average pain, impact on QoL, and stress at home were significantly higher in females versus males. Impact on QoL was correlated with average pain, depression, stress at home, and ability to cope with stress at home.
Conclusions
Our study demonstrates that patients with single site nerve compression neuropathies experience fewer negative psychosocial effects compared to patients with more proximal upper extremity peripheral nerve disorders and neuromas. The impact on QoL was strongly correlated with pain and depression, where patients with neuromas and painful peroneal nerve entrapments reported greater detriments to QoL.


Similar content being viewed by others
References
Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung depression scale predicts patient satisfaction independent of the extent of improvement after revision lumbar surgery. Spine J. 2013;13:501–6.
Aprile I, Caliandro P, La Torre G, et al. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005;10:259–68.
Ayers DC, Franklin PD, Ring DC. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. J Bone Joint Surg Am. 2013;95:e165.
Bailey R, Kaskutas V, Fox I, et al. Effect of upper extremity nerve damage on activity participation, pain, depression, and quality of life. J Hand Surg [Am]. 2009;34:1682–8.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–8.
Bear-Lehman J, Poole SE. The presence and impact of stress reactions on disability among patients with arm injury. J Hand Ther. 2011;24:89–93.
Becker SJ, Makanji HS, Ring D. Expected and actual improvement of symptoms with carpal tunnel release. J Hand Surg [Am]. 2012;37:1324–9. e1-5.
Boogaard S, De Vet HC, Faber CG, et al. An overview of predictors for persistent neuropathic pain. Expert Rev Neurother. 2013;13:505–13.
Calderon SA, Zurakowski D, Davis JS, et al. Quantitative adjustment of the influence of depression on the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire. Hand (N Y). 2010;5:49–55.
Cederlund RI, Ramel E, Rosberg HE, et al. Outcome and clinical changes in patients 3, 6, 12 months after a severe or major hand injury—can sense of coherence be an indicator for rehabilitation focus? BMC Musculoskelet Disord. 2010;11:286.
Choi PD, Novak CB, Mackinnon SE, et al. Quality of life and functional outcome following brachial plexus injury. J Hand Surg [Am]. 1997;22:605–12.
Ciaramitaro P, Mondelli M, Logullo F, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010;15:120–7.
Cocito D, Paolasso I, Pazzaglia C, et al. Pain affects the quality of life of neuropathic patients. Neurol Sci. 2006;27:155–60.
Edwards RR, Haythornthwaite JA, Sullivan MJ, et al. Catastrophizing as a mediator of sex differences in pain: differential effects for daily pain versus laboratory-induced pain. Pain. 2004;111:335–41.
Guse DM, Moran SL. Outcomes of the surgical treatment of peripheral neuromas of the hand and forearm: a 25-year comparative outcome study. Ann Plast Surg. 2013;71:654–8.
Kuntsche E, Gabhainn SN, Roberts C, et al. Drinking motives and links to alcohol use in 13 European countries. J Stud Alcohol Drugs. 2014;75:428–37.
Lozano Calderon SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg [Am]. 2008;33:303–7.
Mackinnon SE, Novak CB. Clinical commentary: pathogenesis of cumulative trauma disorder. J Hand Surg [Am]. 1994;19:873–83.
Nisenzon AN, Robinson ME, Bowers D, et al. Measurement of patient-centered outcomes in Parkinson’s disease: what do patients really want from their treatment? Parkinsonism Relat Disord. 2011;17:89–94.
Novak CB, Anastakis DJ, Beaton DE, et al. Patient-reported outcome after peripheral nerve injury. J Hand Surg [Am]. 2009;34:281–7.
Novak CB, Anastakis DJ, Beaton DE, et al. Relationships among pain disability, pain intensity, illness intrusiveness, and upper extremity disability in patients with traumatic peripheral nerve injury. J Hand Surg [Am]. 2010;35:1633–9.
Novak CB, Anastakis DJ, Beaton DE, et al. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011;93:929–36.
Pincus T, Burton AK, Vogel S, et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27:E109–20.
Pourmemari MH, Viikari-Juntura E, Shiri R. Smoking and carpal tunnel syndrome: a meta-analysis. Muscle Nerve. 2014;49:345–50.
Ring D. Symptoms and disability after major peripheral nerve injury. Hand Clin. 2013;29:421–5.
Ring D, Kadzielski J, Fabian L, et al. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88:1983–8.
Rinker B, Fink BF, Barry NG, et al. The effect of cigarette smoking on functional recovery following peripheral nerve ischemia/reperfusion injury. Microsurgery. 2011;31:59–65.
Selby JV, Lopstein SH. PCORI at 3 years—progress, lessons, and plans. N Engl J Med. 2014;370:592–5.
Switaj P, Grygiel P, Anczewska M, et al. Loneliness mediates the relationship between internalised stigma and depression among patients with psychotic disorders. Int J Soc Psychiatry. 2013.
van Wilgen P, Beetsma A, Neels H, et al. Physical therapists should integrate illness perceptions in their assessment in patients with chronic musculoskeletal pain; a qualitative analysis. Man Ther. 2013.
Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009;91:2014–8.
Vranceanu AM, Jupiter JB, Mudgal CS, et al. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg [Am]. 2010;35:956–60.
Conflict of Interest
Danielle M. Wojtkiewicz declares that she has no conflict of interest.
James Saunders declares that he has no conflict of interest.
Leahthan Domeshek declares that she has no conflict of interest.
Christine B. Novak declares that she has no conflict of interest.
Vicki Kaskutas declares that she has no conflict of interest.
Susan E. Mackinnon declares that she has no conflict of interest.
Statement of Animal and Human Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Wojtkiewicz, D.M., Saunders, J., Domeshek, L. et al. Social impact of peripheral nerve injuries. HAND 10, 161–167 (2015). https://doi.org/10.1007/s11552-014-9692-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9692-0