Abstract
In summer 2020, New York City (NYC) implemented a free air conditioner (AC) distribution program in response to the threats of extreme heat and COVID-19. The program distributed and installed ACs in the homes of nearly 73,000 older, low-income residents of public and private housing. To evaluate the program’s impact, survey data were collected from October 2020 to February 2021 via mail and online from 1447 program participants and 902 non-participating low-income NYC adults without AC as a comparison group. Data were examined by calculating frequencies, proportions, and logistic regression models. Participants were 3 times more likely to report staying home during hot weather in summer 2020 compared to non-participants (adjusted odds ratio [AOR] = 3.0, 95% confidence interval [CI] = 2.2, 4.1), with no difference between groups in summer 2019 (AOR = 1.0, CI = 0.8, 1.3). Participants were less likely to report that 2020 hot weather made them feel sick in their homes compared to non-participants (AOR = 0.2, CI = 0.2, 0.3). The program helped participants—low-income residents and primarily people of color—stay home safely during hot weather. These results are relevant for climate change health-adaptation efforts and heat-health interventions.
Similar content being viewed by others
Introduction
In spring 2020, New York City was the US epicenter of the SARS-CoV-2 (COVID-19) pandemic that had taken the lives of nearly 20,000 residents and resulted in the hospital admission of more than 70,000 people by April 15, 2020 [1]. At the time, no effective treatments were known or vaccines available. New Yorkers were advised to stay home as much as possible as part of social distancing guidelines to prevent viral transmission. Schools, many workplaces, and public spaces were closed, including those that would usually serve as cooling centers during extreme heat events.
In a typical summer, the City advises those at risk of heat-health problems to use their air conditioning (AC) if they have one, setting it to low-cool or 78 °F to save money and protect the electric grid. Those without AC are advised to seek out a cool place, such as a City-run cooling center, an air-conditioned public place, or the home of family or friends with AC. In spring and summer 2020, however, restrictions and closures of non-essential businesses due to the COVID-19 pandemic significantly limited these options for New Yorkers without AC.
In an ordinary year, heat exposure takes a tremendous toll on the health of New Yorkers, killing on average 350 residents a year from 2010 to 2018 by worsening chronic health conditions [2]. These deaths inequitably affect non-Latinx Black New Yorkers [3]. These inequities are rooted in systemic racism that limits economic opportunities, access to health care, and leads to neighborhood and housing disinvestment [4, 5].
AC is the best protection against the adverse health effects of extreme heat. Cities with a higher AC prevalence experience fewer heat-related deaths [6,7,8]. Among New Yorkers who died of heat stress (i.e. the death was recognized and coded as caused by heat) from 2010 to 2019, 71% died in un-air-conditioned homes [2]. Non-Latinx Black and low-income NYC residents, however, are much less likely to have AC [9]. In spring 2020, Black and Latinx New Yorkers also were more likely to hold jobs that did not allow remote work [10], resulting in higher levels of SARS-CoV-2 exposure, and extremely high COVID-19 mortality rates [11]. Older age and having chronic underlying conditions, such as kidney conditions, diabetes, and respiratory or heart disease, also increased risk of severe outcomes from both COVID-19 and heat-related illness [12,13,14,15].
In response to the combined threats of COVID-19 and extreme heat, on May 15, 2020, NYC announced the creation of the Get Cool NYC emergency program, managed by NYC Emergency Management (NYCEM), which distributed and installed nearly 73,000 free home air conditioners to low-income adults aged 60 and older who did not have a working home AC in both New York City Housing Authority (NYCHA) public housing and private housing. In June, the first month of operation, enrollment was limited to clients of means-tested benefit or City programs, such as senior service programs, because they were already age and income verified.
Beginning in late June, supportive housing partners working with the Department of Health and Mental Hygiene (DOHMH) and property managers of Section 8 voucher buildings working with the Department of Housing Preservation and Development Authority (HPD) began enrolling eligible residents in their programs. In addition, the Health Department invited several hundred community- and faith-based organizations to enroll clients through an agreement with the Department allowing the organizations to verify client eligibility. More than 100 organizations, including the three organizations working with the existing Be a Buddy climate resilience program, enrolled approximately 5000 people. New Yorkers could also call 311, the City government’s information and help service, to inquire about eligibility.
NYCHA is home to more than 350,000 New Yorkers in about 161,000 households in public housing, of which 41% are headed by an adult aged 62 or older and 91% are headed by someone who is Latinx or Black [16]. The average family size is 2.2 people and the average family income is $24,503 [17]. For the Get Cool program, NYCHA aimed to make AC installation available for all households that did not have a working AC with a resident aged 60 and older or with a resident of any age with a registered mobility impairment or dependence on lifesaving medical equipment in NYCHA records. Installed AC units belonged to NYCHA to facilitate ongoing maintenance; this also allowed the agency to waive the monthly AC surcharge it typically charges for resident-owned AC installation and use during the pandemic. NYCHA coordinated closely with the larger Get Cool program, but its AC installation and data management efforts were managed in-house.
Between June and September 2020, Get Cool led to the installation of more than 16,000 AC units in NYCHA homes and more than 56,000 in non-NYCHA homes. We performed an equity assessment of installations to better understand the neighborhood reach of the program. To evaluate the impact of receiving an AC, we surveyed Get Cool participants and a comparison group of non-participants about their experiences with hot weather during summer 2019 and 2020. The survey also asked about barriers to AC acquisition and use. An understanding of outcomes from this emergency program can inform future interventions to address increasing and intensifying heat due to climate change, particularly among people who are at increased heat-health risk.
Methods
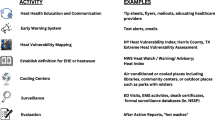
The study team included members from DOHMH, Columbia University’s Mailman School of Public Health, WE ACT for Environmental Justice (WE ACT), and NYCHA, with support from HPD and the New York City Department for the Aging (DFTA). AC installation rates were mapped to understand the spatial distribution of the program using Get Cool program AC installation data from NYCEM. Denominators were based on the number of adults 60 and older living below the federal poverty line from 2015 to 2019 American Community Survey population estimates. We also calculated AC installation rates by DOHMH heat vulnerability index (HVI) level and NYC Task Force for Racial Inclusion and Equity (TRIE) neighborhoods. The HVI estimates heat-health risk across NYC neighborhoods based on a statistical model that uses social and environmental factors, with levels 1 to 5 for lowest to highest risk [3, 18]. TRIE neighborhoods were designated in 2020 as those most impacted by COVID-19 and a high percentage of other health and socioeconomic inequities [19]. Rate denominators for HVI and TRIE areas were based on DOHMH population estimates for all adults aged 60 years and older in 2019, modified from US Census Bureau intercensal population estimates for modified zip code tabulation areas.
The survey included questions about household AC, where and how people kept cool during very hot weather in summer 2019 and 2020, feeling sick from heat while home, how the household was affected by COVID-19, barriers to using or purchasing AC in the past, energy insecurity, self-reported health status, and basic demographics. Participant and non-participant surveys were identical, except the participant survey included a question about Get Cool program satisfaction and references to receiving an AC. On both surveys, survey respondents had the option of writing brief free text responses to some questions.
During survey development, DOHMH convened a virtual meeting of about 80 partners from community-based organizations participating in the Get Cool program to describe evaluation plans and gather feedback on the draft survey. We tailored the survey for public housing residents, removing questions about energy insecurity, appropriate only for respondents paying utility bills directly, and household income. All survey respondents were offered a $10 gift card as an incentive.
Survey Among Public Housing Residents
NYCHA sent the survey to 5300 heads of households who received ACs. Recipients were randomly sampled from the 8055 Get Cool records entered in the NYCHA database as of October 2020. Because NYCHA aimed to provide all its residents aged 60 and older with ACs, the comparison survey was sent to 5300 heads of household aged 53–59 (younger than eligibility age) who were not otherwise eligible for Get Cool and had no NYCHA record of an AC. All 5028 heads of households aged 54–59 without a registered AC were included in the sample and the remaining 272 people were randomly selected from 802 heads of household aged 53. Some de-identified administrative data, such as age, race/ethnicity, and whether electricity was paid directly, were included in the NYCHA dataset from which the Get Cool participant and comparison records were randomly sampled. These elements were linked with survey responses based on survey ID numbers.
The survey was mailed in English and Spanish with a pre-paid return envelope. The cover letter included directions for how to take the survey online in English, Spanish, Russian, Traditional Chinese, and Simplified Chinese. Respondents could take the survey from November 13, 2020, to February 21, 2021. Because comparison group letters were mailed 2 weeks late, a reminder letter was sent to the comparison group in December 2020, making it clear that they had more time to take the survey. The participant version of the survey included 24 questions and the comparison included 23 questions. De-identified paper survey responses were data entered by trained DOHMH staff.
Survey Among Residents of Private Housing
The private housing survey was mailed to 3800 people who received Get Cool ACs, who were randomly sampled from 23,195 participants who agreed to follow-up contact at the time of AC installation. Surveys were distributed to a comparison group of 8329 non-eligible New Yorkers comprising the following: (1) HPD-managed Sect. 8 tenants aged 55–59 years (n = 5300); (2) DFTA clients not eligible for the program (n = 21); and (3) New Yorkers who called 311 to inquire about the program but were not eligible (n = 3008).
DOHMH contracted with ICF, an independent survey research firm, to mail the survey, as well as two reminder letters and two reminder emails (for those with an email address). Respondents could complete the survey in English or Spanish on paper with a pre-paid return envelope or in any of 7 languages online (Haitian-Creole and French, in addition to the languages available to NYCHA residents). Respondents could take the survey from October 9, 2020, to December 9, 2020. The participant version of the survey included 30 questions and the comparison included 29 questions. Trained ICF staff completed data entry.
Statistical Methods
Data were processed and analyzed in SAS (SAS Institute, Cary, NC). Data from the public housing and private housing surveys were examined separately and then pooled together. The comparison group was restricted to respondents who reported not having a home AC in 2019. Data were examined by calculating frequencies, proportions, and logistic regression models. Missing data were excluded from analyses. Significance was assessed by examining magnitude of estimates and confidence limits.
This research was reviewed by the NYC DOHMH and Columbia University Institutional Review Boards and was determined to be exempt.
Results
The Get Cool program reached every neighborhood of the city [20]. AC installation rates were higher in areas with more older adults living below the federal poverty level (see Fig. 1). More ACs were installed in neighborhoods ranking high on the DOHMH Heat Vulnerability Index [3] and with the greatest morbidity and mortality from COVID-19. Installation rates were more than twice as high in HVI 4 areas (47.7 per 1000 older adults) and nearly five times higher in HVI 5 areas (94.1 per 1000) compared to HVI levels 1–3 areas (20.4 per 1000, see Supplemental Table 1). Installations in TRIE areas were about four times higher compared to non-TRIE areas (68.1 installations vs. 18.1 per 1000).
Rate of Get Cool AC installations by modified zip code tabulation area, heat vulnerability index (HVI) level, and NYC Task Force for Racial Inclusion and Equity (TRIE) neighborhoods designated as most impacted by COVID-19 and other health and socioeconomic disparities. Rate denominators are the number of adults 60 and older living below the federal poverty level. Rate numerators based on NYC Emergency Management Get Cool program AC installation data. Map created by Erika Poulsen, NYC Department of Health and Mental Hygiene
Together, the surveys had a response rate of 15.9% (1447 of 9100 mailed) for participants and 13.8% (1885 of 13,629 mailed) for the comparison group using the American Association of Public Opinion Research response rate 2 definition, i.e., the number of returned complete and partial surveys divided by the total number people invited to take the survey. In the comparison group, 902 (48%) respondents reported not having AC in 2019 (n = 507 for the public housing survey, and n = 395 for the private housing survey) and were included in this analysis. Among the 2349 responses analyzed, 88% (n = 2056) of responses were in English, 11% (n = 266) in Spanish, 1% (n = 13) in Chinese-Traditional, and the remaining 1% were in Chinese-Simplified (n = 6), Russian (n = 7), and Creole (n = 1). Mailed surveys accounted for 74% (n = 1732) of responses.
Respondents were primarily people of color, with the participant group including more Latinx (39% versus 32%) and fewer non-Latinx Black residents (39% versus 54%) than the comparison (Table 1). About 60% reported not having an AC in 2019. One quarter of the comparison group was aged 60 or older. Seventy percent (95% confidence interval [CI]: 65, 75) of the private housing comparison and 67% (CI: 63, 70) of the private housing participant group reported a household income of less than $20,000 (data not shown). Chronic health conditions were prevalent in both groups, including hypertension, diabetes, and asthma or chronic obstructive pulmonary disease (COPD). In addition, 24% (CI: 22, 26) of participants and 29% (CI: 26, 32) of non-participants reported that they or someone in their household had anxiety, depression, or other mental health conditions.
Both groups were affected by COVID-19, with 11% (CI: 10, 13) of participants and 8% (CI: 6, 9) of non-participants reporting a household member diagnosed with COVID-19. Five percent (CI: 4, 6) of participants and 3% (CI: 2, 4) of the comparison group reported that a household member died. Some respondents wrote that even though they did not lose a household member or experience illness in the household, they were still deeply affected by the pandemic. “From all my childhood friends, I am the only one left with a living parent (who did not die of Covid). I am their relief, but it is trying for me,” wrote a respondent. About one-fifth of each group reported having a household member lose a job. “My job ended on March 15,” wrote one respondent. “I lost a substantial amount of my income.” Some respondents described experiencing fear and isolation because of COVID-19: “It took a toll on my mental state of mind. I was feeling depressed,” said a respondent. “It is a very scary time, and I am worried for myself and my relatives,” wrote another. “I can’t go to adult day care, can’t communicate with my friends, can’t get enough food on time,” wrote another respondent.
In summer 2020, more participants reported staying home during very hot weather than non-participants (Table 2: 89%, CI: 88, 91 versus 73%, CI: 70, 76 respectively). Among participants, 87% (CI: 85, 89) used AC to cool their homes during very hot weather in 2020 always, most of the time, or half the time (data not shown). Participants were also more likely to report staying home because they were comfortable there. In summer 2019, there was no difference in staying home between the groups (Table 2: 71%, CI: 69, 74 versus 69%, CI: 66, 72 respectively). Non-participants were more likely to go to a work location to cool off in 2020 (12% [CI: 10, 14] for the comparison group and 5% [CI :4, 6] for participant), possibly because the comparison group skewed younger, although the majority of both groups did not go to work to cool off. More than one-quarter of non-participants (27%, CI: 24, 30) reported that hot weather made them or someone in their household feel sick at home in summer 2020, compared to only 10% (CI: 9, 12) of participants. Only 7% (CI: 6, 9) of participants and 9% (CI: 7, 10) of non-participants reported going to a City-designated cooling center in 2020, with slightly higher rates of attendance in 2019 (17% of participants and 11% of non-participants).
In logistic regression models including race/ethnicity and age, participants were three times more likely to stay home in 2020 during hot weather compared to non-participants (Table 3, adjusted odds ratio [AOR] = 3.0, CI: 2.2, 4.1), but there was no difference between groups in summer 2019 (AOR = 1.0, CI: 0.8, 1.3). Also adjusting for race/ethnicity and age, participants were less likely to report that hot weather made them feel sick in their homes (AOR = 0.2, CI = 0.2, 0.3). Overall, 91% of participants reported satisfaction with the Get Cool program.
Both participants and non-participants cited many obstacles to getting an AC in the past. Cost of the unit (62% and 56% respectively), electricity cost (40% and 25% respectively), and cost of proper installation (29% and 24% respectively) were the top barriers (Table 4). “Had air conditioner when I was working. Retired. I had to let it go,” wrote one respondent. Another noted they could “hardly pay my rent.” For public housing residents, the year-round monthly AC surcharge fee was one of the largest barriers to getting an AC in the past. More than one-third (35%, CI: 31, 38) of public housing participants and 41% (CI: 37, 45) of non-participants reported concerns about paying the monthly fee, which ranges from $4 to $10 per AC unit depending on age and income levels and is required by the US Department of Housing and Urban Development (HUD) for resident-owned air conditioners.
Discussion
More ACs were installed in both high-heat vulnerability areas and in neighborhoods that were highly impacted by the first wave of COVID-19 in NYC. Survey results indicate that the Get Cool program was successful in helping at-risk individuals stay home safely with AC during a summer of active COVID-19 transmission and extreme heat. Participants were more likely to report staying home in hot weather in 2020 than non-participants, with no difference between groups in 2019 (i.e., pre-intervention). Previous studies have shown that people prefer to be able to stay home during hot weather, but lower-income and non-Latinx Black New Yorkers lack equitable cooling access [9]. Participants in the AC program were also much less likely to report that hot weather made them feel sick in their homes than non-participants, indicating that having the unit helped keep them safe during hot weather. Substantial NYC air quality improvements in spring 2020 related to decreased economic activity may have also contributed to people feeling less sick on hot days [21], but any such impacts would affect the two groups equally so cannot explain lower reports of heat health impacts among participants. The survey also documented the substantial impacts of COVID-19 in the population prioritized by the Get Cool program.
The cost to purchase and run an AC remains a large barrier to equitable access to summer cooling. More than half of participants and non-participants reported that the cost of an AC unit had prevented them from having one in the past. More than 90% of New Yorkers citywide have AC, but there are large inequities by neighborhood, with prevalence ranging from 95% in wealthy neighborhoods to 71% in lower-income areas [22], and lower rates of AC access among Black New Yorkers. In addition, 40% of participants and 25% of non-participants said the additional energy costs were a barrier. This is consistent with previous NYC surveys that also cited increases in electricity bills as a deterrent to AC use [9, 23]. People living in public housing reported that the monthly AC surcharge charged by NYCHA as required by HUD deterred them from getting an AC, even though many residents are highly heat susceptible. Previous studies have shown that inequities in energy security are prevalent, with low-income people and people of color facing a higher energy burden due in part to lack of weatherization, including structural deficiencies and outdated appliances [24, 25].
A relatively small percent of both groups used cooling centers in 2020 and 2019, highlighting the importance of access to home cooling. While the survey did not ask about reasons for cooling center use, some people with AC may go to cooling centers because of concerns about paying the electricity bill [26]. Increasing funding for cooling center programs to allow for more programming to encourage use, extended hours, and advertising in collaboration with community organizations and residents could increase attendance and bolster the utility of these important community resources [27].
While AC helps people to stay home safely in hot weather, it does not replace the need for community supports, including for mental health and other social services. Social isolation during social distancing and other stressors from the pandemic, such as loss of a job, illness, or loss of friends or loved ones, may have exacerbated or increased the existing burden of mental health problems. In addition to the prevalence of chronic conditions, there were high levels of anxiety, depression, and mental health conditions reported among all households surveyed. In comparison, the NYC Community Health Survey, a representative telephone survey of NYC adults, measured current prevalence of depression at 9.3% (8.1, 9.8) citywide in 2017 [28]. While this was an individual measure and we asked about household prevalence of mental health conditions, the average of 26% of households across both groups reporting a mental health condition paints a picture of the isolation and mental stress that respondents experienced during and following the first COVID-19 wave in NYC. This underscores the importance of coupling interventions to increase home safety and comfort with social connectedness programs.
Our analysis had several limitations. For the map of installations, denominator data that matched eligibility criteria exactly was not available. However, mapping installations against the number of older adults living below the federal poverty line, although a lower income threshold than required by the Get Cool program, provides a visualization of how many ACs were delivered in areas with larger numbers of resource-limited older adults. In addition, the heat vulnerability index and TRIE area designations include measures of limited financial resources. Because people took the survey in late 2020 and early 2021, there may have been recall bias and confusion about questions that asked about “this summer (2020)” versus “last summer (2019),” despite inclusion of the year in all questions. In addition, more than a third of program participants reported having an AC in 2019. These respondents may have been confused by the question timeframe and wording, which asked about which rooms in the home had AC “last summer (2019),” since the survey was mailed in fall 2020 and responses collected into early 2021, the next calendar year. In addition, AC units may have broken, or survey respondents may have moved to housing without AC prior to 2020.
Participants who were aware that the survey was asking about their new AC may have been more likely to report using it, potentially leading to an over-estimation of benefits. However, the magnitude of difference between the participant and comparison group in staying home and not feeling ill is unlikely to be solely explained by this factor. Differences between our participant and non-participant groups may also affect comparability. There may have been confounding by age because by necessity our comparison group skewed younger and reported a higher, though still minimal, prevalence of going to a workplace. Older adults may have been more likely to follow social distancing recommendations out of fear of contracting COVID-19 than younger adults, also affecting comparability of the groups. About 25% of our comparison group, however, was aged 60 or older, and younger and older non-participants had similar rates of staying home in 2019 and 2020. The comparison group also differed from the participant group by race and ethnicity, with fewer Latinx respondents and more Black respondents.
Because we did not aim to make the survey representative of any group beyond Get Cool participants, we did not weight survey responses to be representative of a larger population. Participants of the Get Cool program itself were largely enrolled based on participation in other safety-net programs, with the exception of the DOHMH community- and faith-based organization partner enrollment. Previous research has shown that people linked to services may be more likely to receive other types of services [29]. The Get Cool program and this evaluation both suffered from a general limitation of government programs that recruit from people connected to existing programs—they likely missed New Yorkers who would have benefitted from the service and cannot estimate outcomes for that population.
Conclusions
The emergency distribution and installation of free air conditioners helped participants stay home safely in summer 2020. While Get Cool was launched as a joint COVID-19 and heat emergency response measure, program outcomes are relevant for heat adaptation with or without active COVID-19 transmission. AC access is critical to achieving climate justice as cities continue to warm, and public health crises persistently impact the same heat-vulnerable communities that have endured decades of systemic racism and disinvestment.
AC access could be improved by substantially improving the reach, decreasing the application burden, and increasing funding levels of existing cooling assistance programs, such as the Home Energy Assistance Program (HEAP). Currently, HEAP in New York provides a small amount of cooling assistance each year by funding the purchase of an AC but does not provide summer utility assistance. Given that NYC has one of the largest energy cost burdens in the country for low-income residents [30], HEAP and other energy assistance programs also should provide utility subsidies so people can afford to run ACs in summer, in line with the life-saving supports instituted in the past to ensure winter heat. In addition, the City should explore regulations to require landlords to provide access to working AC and prohibit additional surcharges for use.
Given the huge public health challenges posed by climate change in cities like NYC, increased AC access needs to go hand-in-hand with other interventions. Public AC access programs should, at minimum, prioritize providing efficient models and properly air-sealing units when installed. Additional interventions should include initiatives like increasing funding for energy efficiency and weatherization programs, ramping up community solar programs to help ease energy costs, increasing funding for cooling centers and greening in high heat-risk areas, and funding community-led resilience programs. Heat waves and other climate change hazards exacerbate existing inequities, and interact with other public health emergencies, as demonstrated by the COVID-19 pandemic, requiring not only emergency but also structural and sustainable solutions.
References
New York City Department of Health & Mental Hygiene. NYC COVID-19 data: trends and totals; Available from: https://www1.nyc.gov/site/doh/covid/covid-19-data-totals.page. Accessed 4 Oct 2021.
New York City Department of Health & Mental Hygiene. New York City heat-related mortality report. 2021. Available from: https://nyccas.cityofnewyork.us/nyccas2021v9/report/1. Accessed 4 Oct 2021.
Madrigano J, Ito K, Johnson S, Kinney PL, Matte T. A case-only study of vulnerability to heat wave-related mortality in New York City (2000–2011). Environ Health Perspect. 2015;123(7):672–8.
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63.
Hoffman JS, Shandas V, Pendleton N. The effects of historical housing policies on resident exposure to intra-urban heat: a study of 108 US urban areas. Climate. 2020;8(1):12. https://doi.org/10.3390/cli8010012
Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64(12):827–33.
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155(1):80–7.
O’Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health. 2005;82(2):191–7.
Madrigano J, Lane K, Petrovic N, Ahmed M, Blum M, Matte T. Awareness, risk perception, and protective behaviors for extreme heat and climate change in New York City. Int J Environ Res Public Health. 2018;15(7):1433. https://doi.org/10.3390/ijerph15071433.
Gwynn RC. Health inequity and the unfair impact of the COVID-19 pandemic on essential workers. Am J Public Health. 2021;111(8):1459–61.
Thompson CB, Baumgartner J, Pichardo C, et al. COVID-19 outbreak — New York City, February 29–June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1725–9. https://doi.org/10.15585/mmwr.mm6946a2.
Fletcher BA, Lin S, Fitzgerald EF, Hwang SA. Association of summer temperatures with hospital admissions for renal diseases in New York State: a case-crossover study. Am J Epidemiol. 2012;175(9):907–16.
Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738–46.
Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117(1):61–7.
New York City Department of Health & Mental Hygiene. What you need to know about COVID-19. 2021; Available from: https://www1.nyc.gov/site/doh/covid/covid-19-main.page. Accessed 5 Oct 2021.
New York City Housing Authority. Resident data book summary. Manhattan, NY: New York City Housing Authority; 2021. https://www1.nyc.gov/assets/nycha/downloads/pdf/Resident-Data-Book-Summary-2021.pdf. Accessed 5 Oct 2021.
New York City Housing Authority. NYCHA. Fact Sheet; 2021. Available from: https://www1.nyc.gov/assets/nycha/downloads/pdf/NYCHA-Fact-Sheet_2021.pdf. Accessed 5 Oct 2021.
New York City Department of Health & Mental Hygiene. Heat vulnerability index. 2018. Available from: https://a816-dohbesp.nyc.gov/IndicatorPublic/VisualizationData.aspx?id=2411,719b87,107,Summarize. Accessed 17 May 2022.
NYC Taskforce on Racial Inclusion & Equity (TRIE) Neighborhoods. https://www1.nyc.gov/site/trie/index.page. Accessed 5 Oct 2021.
New York City Emergency Management & New York City Housing Authority. Get Cool program installation data. 2021. (Not publicly available).
Pitiranggon M, Johnson S, Huskey C, Eisl H, Ito K. Effects of the COVID-19 shutdown on spatial and temporal patterns of air pollution in New York City. Environ Adv. 2022;7(100171):2666–7657. https://doi.org/10.1016/j.envadv.2022.100171.
U.S. Census Bureau. New York City Housing and Vacancy Survey (HVS). Households reporting air conditioning, 2017. New York City Department of Health and Mental Hygiene Environment and Health Data Portal. Available at https://a816-dohbesp.nyc.gov/IndicatorPublic/beta/data-explorer/housing-safety/. Accessed 5 Oct 2021.
Lane K, Wheeler K, Charles-Guzman K, et al. Extreme heat awareness and protective behaviors in New York City. J Urban Health. 2014;91(3):403–14.
Lewis J, Hernandez D, Geronimus AT. Energy efficiency as energy justice: addressing racial inequities through investments in people and places. Energy Effic. 2019;13(3):419–32.
Tong K, Ramaswami A, Xu CK, Feiock R, Schmitz P, Ohlsen M. Measuring social equity in urban energy use and interventions using fine-scale data. Proc Natl Acad Sci USA. 2021;118(24):e2023554118. https://doi.org/10.1073/pnas.2023554118.
Berisha VHD, Roach M, White JR, McKinney B, Bentz D, Mohamed A, Uebelherr J, Goodin K. Assessing adaptation strategies for extreme heat: a public health evaluation of cooling centers in Maricopa County, Arizona. Weather Climate Soc. 2017;9:71–80.
WE ACT for Environmental Justice, A call for NYC cooling center improvements: results from WE ACT for Environmental Justice’s Cooling Center Audit Project. 2020. https://www.weact.org/wp-content/uploads/2020/07/WE-ACT-Cooling-Center-Report-Short032320.pdf. Accessed 5 Oct 2021.
New York City Department of Health & Mental Hygiene. Prevalence for current depression. 2017; Available from: https://a816-health.nyc.gov/hdi/epiquery/visualizations?PageType=ps&PopulationSource=CHS. Accessed 5 Oct 2021.
Higgins L. and Lutzenhiser L. Ceremonial equity: low-income energy assistance and the failure of socio-environmental policy. Soc Probl. 1995;42(4):468–92.
Drehobl A, Ross L, Ayala R. How high are household energy burdens? Washington, DC: American Council for an Energy-Efficient Economy; 2020. https://www.aceee.org/sites/default/files/pdfs/u2006.pdf. Accessed 5 Oct 2021.
Acknowledgements
The authors gratefully acknowledge the survey respondents for taking the time to share their experiences. We are grateful to Erika Poulsen from the Department of Health & Mental Hygiene for mapping the Get Cool AC installation rates. We also thank our colleagues Anne-Marie Flatley, Jordan Bonomo, and Vlada Kenniff from the New York City Housing Authority, Narine Malcolm, Gail Garbowski, and Miranda Simes from Columbia University Mailman School of Public Health, Krisly Diaz, Tatyana Dubson, Rebecca Goldberg, Kaz Ito, Sarah Johnson, Aining Liu, and Carla Rossi from the NYC Department of Health and Mental Hygiene, as well as colleagues from the NYC Department of Housing, Preservation and Development, the NYC Department for the Aging, and New York City Emergency Management for many different but critical types of support to this evaluation survey. We also wish to thank Kizzy Charles-Guzman from the Mayor’s Office of Climate and Environmental Justice, the Air Conditioning Task Force, and the many City staff across multiple agencies who worked on the program in 2020. This study was funded by National Institute of Environmental Health Sciences grant P30 ES009089 (Center for Environmental Health in Northern Manhattan), New York City tax levy funds, and New York City Housing Authority operating funds from the US Department of Housing and Urban Development.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lane, K., Smalls-Mantey, L., Hernández, D. et al. Extreme Heat and COVID-19 in New York City: An Evaluation of a Large Air Conditioner Distribution Program to Address Compounded Public Health Risks in Summer 2020. J Urban Health 100, 290–302 (2023). https://doi.org/10.1007/s11524-022-00704-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00704-9