Abstract
Background
Brachial plexus injury (BPI) is a life-altering event, and surgical treatment of BPI is costly ($66 million nationwide in 2006 alone). Despite the sizable costs associated with surgically treated BPI, the incidence of such cases in adults in the USA remains unknown.
Questions/Purposes
We sought to provide an estimate of the national incidence of surgically treated BPI in the USA and to determine whether changes have occurred over time.
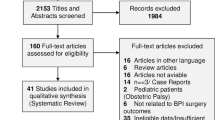
Methods
We sought to identify privately insured adults ages 18 through 64 years who underwent BPI surgery between 2008 and 2014 in the IBM® MarketScan® Commercial Database. We then extrapolated those data to the same age group in the general population (all insurance types were considered), using data from the National Health Interview Survey and a study on the proportion of BPI surgery cases covered by private insurance to estimate the national incidence. We also used the Cochran–Armitage trend test to evaluate for statistically significant changes in BPI incidence over time in MarketScan private insurance data.
Results
We identified 966 patients surgically treated for BPI in the MarketScan database in the study period. The average annual incidence of surgically treated BPI in this population of privately insured patients was 0.64 per 100,000 (range, 0.38 to 1.03). When extrapolated to all payers, the average annual incidence was 0.89 per 100,000 people (range, 0.53 to 1.47). In the MarketScan data, there was a statistically significant overall increase in the incidence of surgically treated BPI from 2008 through 2014 (0.47 per 100,000 to 1.03 per 100,000).
Conclusion
The estimated annual incidence of surgically treated BPI is 0.89 per 100,000 persons in the USA, and the incidence has increased over time. These findings can serve as a baseline for further studies of disease epidemiology and societal and financial impact.

Similar content being viewed by others
References
Bulstra LF, Rbia N, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Spinal accessory nerve to triceps muscle transfer using long autologous nerve grafts for recovery of elbow extension in traumatic brachial plexus injuries. J Neurosurg. 2018;129(4):1041–1047. doi:https://doi.org/10.3171/2017.6.JNS17290
Clarke TN, Schiller J. Early release of selected estimates based on data from 2016 national health interview survey. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/nhis.htm. Published 2017.
DeGeorge BR, Becker HA, Faryna JH, Spinner RJ, Bishop AT, Shin AY. Outcomes of muscle brachialis transfer to restore finger flexion in brachial plexus palsy. Plast Reconstr Surg. 2017;140(2):307e–317e. doi: https://doi.org/10.1097/PRS.0000000000003563
Desai MJ, Daly CA, Seiler JG, Wray WH, Ruch DS, Leversedge FJ. Radial to axillary nerve transfers: a combined case series. J Hand Surg Am. 2016;41(12):1128–1134. doi: https://doi.org/10.1016/j.jhsa.2016.08.022
Dy CJ, Baty J, Saeed MJ, Olsen MA, Osei DA. A population-based analysis of time to surgery and travel distances for brachial plexus surgery. J Hand Surg Am. 2016;41(9):903–909.e3. doi: https://doi.org/10.1016/j.jhsa.2016.07.054
Dy CJ, Garg R, Lee SK, Tow P, Mancuso CA, Wolfe SW. A systematic review of outcomes reporting for brachial plexus reconstruction. J Hand Surg Am. 2015;40(2):308–313. doi: https://doi.org/10.1016/j.jhsa.2014.10.033
Faciszewski T, Broste SK, Fardon D. Quality of data regarding diagnoses of spinal disorders in administrative databases. A multicenter study. J Bone Jt Surg Am. 1997;79(10):1481–1488. doi: https://doi.org/10.2106/00004623-199710000-00004
Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare’s hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82(2):243–248. doi: https://doi.org/10.2105/AJPH.82.2.243
Flores LP. [Epidemiological study of the traumatic brachial plexus injuries in adults.] [Article in Portuguese]. Arq Neuropsiquiatr. 2006;64(1):88–94.
Freedman JD, Green L, Landon BE. All-payer claims databases—uses and expanded prospects after Gobeille. N Engl J Med. 2016;375(23):2215–2217. doi: https://doi.org/10.1056/NEJMp1613276
Goldie BS, Coates CJ. Brachial plexus injury: a survey of incidence and referral pattern. J Hand Surg Br. 1992;17(1):86–88.
Kalsbeek WD, McLaurin RL, Harris BS, Miller JD. The National Head and Spinal Cord Injury Survey: major findings. J Neurosurg. 1980;Suppl:S19–S31.
Kim DH, Murovic JA, Tiel RL, Kline DG. Gunshot wounds involving the brachial plexus: surgical techniques and outcomes. J Reconstr Microsurg. 2006;22(2):67–72. doi: https://doi.org/10.1055/s-2006-932499
Lad SP, Nathan JK, Schubert RD, Boakye M. Trends in median, ulnar, radial, and brachioplexus nerve injuries in the United States. Neurosurgery. 2010;66(5):953–960. doi: https://doi.org/10.1227/01.NEU.0000368545.83463.91
Maldonado AA, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Free functioning gracilis muscle transfer with and without simultaneous intercostal nerve transfer to musculocutaneous nerve for restoration of elbow flexion after traumatic adult brachial pan-plexus injury. J Hand Surg Am. 2017;42(4):293.e1–293.e7. doi: https://doi.org/10.1016/j.jhsa.2017.01.014
Midha R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery. 1997;40(6):1182–1188; discussion 1188–1189. doi: https://doi.org/10.1097/00006123-199706000-00014
Ray WZ, Murphy RKJ, Santosa K, Johnson PJ, Mackinnon SE. Medial pectoral nerve to axillary nerve neurotization following traumatic brachial plexus injuries: indications and clinical outcomes. Hand (N Y). 2012;7(1):59–65. doi: https://doi.org/10.1007/s11552-011-9378-9
Ray WZ, Pet MA, Yee A, Mackinnon SE. Double fascicular nerve transfer to the biceps and brachialis muscles after brachial plexus injury: clinical outcomes in a series of 29 cases. J Neurosurg. 2011;114(6):1520–1528. doi: https://doi.org/10.3171/2011.1.JNS10810
Sulaiman OAR, Kim DD, Burkett C, Kline DG. Nerve transfer surgery for adult brachial plexus injury: a 10-year experience at Louisiana State University. Neurosurgery. 2009;65(4 Suppl):A55–A62. doi: https://doi.org/10.1227/01.NEU.0000341165.83218.AC
Wolfe SW, Johnsen PH, Lee SK, Feinberg JH. Long-nerve grafts and nerve transfers demonstrate comparable outcomes for axillary nerve injuries. J Hand Surg Am. 2014;39(7):1351–1357. doi: https://doi.org/10.1016/j.jhsa.2014.02.032
Funding
This publication was made possible by Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345, sub-award KL2 TR000450 (C.J.D.), from the National Center for Advancing Translational Sciences (NCATS) components of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. The Center for Administrative Data Research (M.A.O., K.P.) is supported in part by Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the NCATS and grant R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christopher J. Dy, MD, MPH, FACS; Kate Peacock, BS; and Margaret A. Olsen, PhD, MPH, declare that they have no conflict of interest. Wilson Z. Ray, MD, reports receiving grants from the Department of Defense and from the National Institutes of Health/National Institute of Neurological Disorders and Stroke, and personal fees from Globus Medical and from Depuy Synthes, outside the submitted work. David M. Brogan, MD, MSc, reports receiving grants from American Foundation for Surgery of the Hand, nonfinancial support from Axogen, personal fees from Arthrex and from TriMed, and grants from the University of Missouri Orthopedic Association and from KL2 Research Award, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Disclaimer
This publication’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCATS, ARHQ, or NIH.
Additional information
Level of Evidence: Level III: Retrospective Cohort Study.
Electronic supplementary material
ESM 1
(PDF 1224 kb)
Rights and permissions
About this article
Cite this article
Dy, C.J., Peacock, K., Olsen, M.A. et al. Incidence of Surgically Treated Brachial Plexus Injury in Privately Insured Adults Under 65 Years of Age in the USA. HSS Jrnl 16 (Suppl 2), 339–343 (2020). https://doi.org/10.1007/s11420-019-09741-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-019-09741-8