Abstract
Purpose
Ropinirole is an antiparkinsonian drug and has recently been suggested to be effective in amyotrophic lateral sclerosis. It is expected that ropinirole prescriptions will increase in the near future. However, the fatal concentration in blood is unclear at this time. Therefore, we report a fatal case involving ropinirole intoxication and discuss the fatal concentrations with reference to several autopsy cases involving ropinirole.
Methods
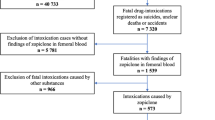
Ropinirole was quantified in femoral vein blood, cardiac blood, and urine from five autopsy cases in which ropinirole was detected by drug screening in our laboratory. One is a ropinirole intoxication case (this report) and the others were non-intoxication cases. Their ropinirole concentrations were compared and discussed.
Results
The ropinirole concentration in this case was 100 ng/mL in femoral blood, 160 ng/mL in cardiac blood, and 1840 ng/mL in urine. The ropinirole concentrations in the four non-ropinirole poisoning cases were 7–35 ng/mL (mean: 24 ng/mL) in femoral blood, 13–100 ng/mL (mean: 60 ng/mL) in cardiac blood, and 140–1090 ng/mL (mean: 640 ng/mL) in urine. Cardiac/peripheral ratios were in the range of 1.6–2.1 (mean 1.8).
Conclusions
There were no obvious signs of overdose, and the high cardiac/peripheral blood ratio suggested that postmortem redistribution may have occurred, but the peripheral blood ropinirole concentration (100 ng/mL) was obviously higher than that reported in the previous fatal case of ropinirole poisoning (64 ng/mL). Based on these results, the cause of death in this case was considered to be shock and fatal arrhythmia due to ropinirole poisoning. This case provides important data on postmortem blood and urinary levels of ropinirole poisoning.



Similar content being viewed by others
References
Rizek P, Kumar N, Jog MS (2016) An update on the diagnosis and treatment of Parkinson disease. CMAJ 188:1157–1165. https://doi.org/10.1503/cmaj.151179 (open access article)
Delamarre A, Meissner WG (2017) Epidemiology, environmental risk factors and genetics of Parkinson’s disease. Presse Med 46:175–181. https://doi.org/10.1016/j.lpm.2017.01.001 (open access article)
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (2016) Global regional and national incidence, prevalence and years lived with disability for 310 disease and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6001 (open access article)
Marras C, Beck JC, Bower JH, Roberts E, Ritz B, Ross GW, Abbott RD, Savica R, Van Den Eeden SK, Willis AW, Tanner CM, Parkinson’s Foundation P4 Group (2018) Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis 4:21. https://doi.org/10.1038/s41531-018-0058-0 (open access article)
Vidaihlet MJ, Bonnet AM, Belal S, Dubois B, Marle C, Agid Y (1990) Ropinirole without levodopa in Pakinson’s disease. Lancet 336:316–317. https://doi.org/10.1016/0140-6736(90)91855-5
Trenkwalder C, Hening WA, Montagna P, Oertel WH, Allen RP, Walters AS, Costa J, Stiasny-Kolster K, Sampaio C (2008) Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord 23:2267–2302. https://doi.org/10.1002/mds.22254 (open access article)
Fujimori K, Ishikawa M, Otomo A, Atsuta N, Nakamura R, Akiyama T, Hadano S, Aoki M, Saya H, Sobue G, Okano H (2018) Modeling sporadic ALS in IPSC-derived motor neurons identifies a potential therapeutic agent. Nat Med 24:1579–1589. https://doi.org/10.1038/s41591-018-0140-5
Morimoto S, Takahashi S, Fukushima K, Saya H, Suzuki N, Aoki M, Okano H, Nakahara J (2019) Ropinirole hydrochloride remedy for amyotrophic lateral sclerosis–protocol for a randomized, double-blind, placebo-controlled, single-center, and open-label continuation phase I/IIa clinical trial (ROPALS trial). Regen Ther 11:143–166. https://doi.org/10.1016/j.reth.2019.07.002 (open access article)
Okano H, Yasuda D, Fujimori K, Morimoto S, Takahashi S (2020) Ropinirole, a new ALS drug candidate developed using iPSCs. Trends Pharmacol Sci 41:99–109. https://doi.org/10.1016/j.tips.2019.12.002 (open access article)
Frucht S, Rogers JD, Greene PE, Gordon MF, Fahn S (1999) Falling asleep at the wheel: motor vehicle mishaps in persons taking pramipexole and ropinirole. Neurology 52:1908–1910. https://doi.org/10.1212/wnl.52.9.1908
Duband S, Bidat C, Gaillard Y, Rochet M, Camdessanche JP, Péoc’h M (2012) A fatal intoxication case involving ropinirole. J Forensic Leg Med 19:422–425. https://doi.org/10.1016/j.jflm.2012.04.013
Simkó J, Szentandrássy N, Harmati G, Bárándi L, Horváth B, Magyar J, Bányász T, Lórincz I, Nánási PP (2010) Effects of ropinirole on action potential characteristics and the underlying ion currents in canine ventricular myocytes. Naunyn Schmied Arch Pharmacol 382:213–220. https://doi.org/10.1007/s00210-010-0538-1
Di Giacopo R, Fasano A, Fenici R, Loria G, Bentivoglio AR (2010) Rare and serious cardiac side effects during ropinirole titration. Mov Disord 25:1509–1510. https://doi.org/10.1002/mds.23115
Nagasawa S, Saka K, Yamagishi Y, Yajima D, Chiba F, Yamaguchi R, Torimitsu S, Iwase H (2021) Association between sexual activity-related death and non-prescription use of phosphodiesterase type 5 inhibitors. Leg Med 48:101815. https://doi.org/10.1016/j.legalmed.2020.101815
Usui K, Hayashizaki K, Hashiyada M, Funayama M (2012) Rapid drug extraction from human whole blood using a modified QuEChERS extraction method. Leg Med 14:286–296. https://doi.org/10.1016/j.legalmed.2012.04.008
U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Veterinary Medicine (2018) Bioanalytical method validation: guidance for industry. https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf. Accessed 24 May 2018
Nishikawa N, Nagai M, Moritoyo T, Yabe H, Nomoto M (2009) Plasma amantadine concentrations in patients with Parkinson’s disease. Parkinsonism Relat Disord 15:351–353. https://doi.org/10.1016/j.parkreldis.2008.08.005 (open access article)
Sande MA, Mandell GL (1980) Antimicrobial agents, chap 54. In: Goodman and Gilman’s the pharmacological basic of therapeutic, 6th edn. Macmillan Publishers, New York, p 1241
Schulz M, Schmoldt A, Andersen-Streichert H, Iwersen-Bergmann S (2020) Revisited: therapeutic and toxic blood concentrations of more than 1100 drugs and other xenobiotics. Crit Care 24:195. https://doi.org/10.1186/s13054-020-02915-5 (open access article)
Dalpe-Scott M, Degouffe M, Garbutt D, Drost M (1955) A comparison of drug concentrations in postmortem cardiac and peripheral blood in 320 cases. Can Soc Sci J 28:113–121. https://doi.org/10.1080/00085030.1995.10757474
Tompson DJ, Vearer D (2007) Steady-state pharmacokinetic properties of a 24-hour prolonged-release formulation of ropinirole: results of two randomized studies in patients with Parkinson’s disease. Clin Ther 29:2654–2666. https://doi.org/10.1016/j.clinthera.2007.12.010
Hattori N, Hasegawa K, Sakamoto T (2012) Pharmacokinetics and effect of food after oral administration of prolonged release tablets of ropinirole hydrochloride in Japanese patients with Parkinson’s disease. J Clin Pharm Ther 37:571–577. https://doi.org/10.1111/j.1365-2710.2012.01336.x
Perea E, Robbins BV, Hutto B (2006) Psychosis related to ropinirole. Am J Psychiatry 163:547–548. https://doi.org/10.1176/appi.ajp.163.3.547
Navacerrada F, González-Alonso MR, Alonso-Navarro H, Pilo-de-la-Fuente B, Plaza-Nieto JF, Jiménez-Jiménez FJ (2011) Liver toxicity possibly related with ropinirole use in the treatment of restless legs syndrome. Eur J Neurol 18:e65. https://doi.org/10.1111/j.1468-1331.2010.03317.x
Mannelli M, Lazzeri C, Ianni L, La Villa G, Pupilli C, Bellini F, Serio M, Franchi F (1997) Dopamine and sympathoadrenal activity in man. Clin Exp Hypertens 19:163–179. https://doi.org/10.3109/10641969709080813
Yeh T-L, Yang Y-K, Chiu N-T, Yao W-J, Yeh S-J, Wu J-S, Chuang J-I, Chang SH (2006) Correlation between striatal dopamine D2/D3 receptor binding and cardiovascular activity in healthy subjects. Am J Hypertens 19:964–969. https://doi.org/10.1016/j.amjhyper.2006.03.005 (open access article)
Hurst RS, Higdon NR, Lawson JA, Clark MA, Rutherford-Root KL, McDonald WG, Haas JV, McGrath JP, Meglasson MD (2003) Dopamine receptor agonists differ in their actions on cardiac ion channels. Eur J Pharmacol 482:31–37. https://doi.org/10.1016/j.ejphar.2003.09.054
Humphrey SJ, Turman CN, Curry JT, Wheeler GJ (2006) Cardiovascular and electrocardiographic effects of the dopamine receptor agonists ropinirole, apomorphine, and PNU-142774E in conscious beagle dogs. J Cardiovasc Pharmacol 47:337–347. https://doi.org/10.1097/01.fjc.0000205983.05771.f5
Baselt RC (2017) Disposition of toxic drugs and chemicals in man, 11th edn. Biomedical Publications, Seal Beach, p 1805
Acknowledgements
We thank Vikas Narang, chief operating officer from Editage for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or other relations that could lead to conflicts of interest.
Ethics approval
All the procedures performed in this study were in accordance with the ethical standards set by our institutional review board, and the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nagasawa, S., Yamaguchi, R., Saka, K. et al. Ropinirole involved in a fatal case: blood and urinary concentrations. Forensic Toxicol 40, 173–179 (2022). https://doi.org/10.1007/s11419-021-00593-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11419-021-00593-8