Abstract
Balancing stroke prevention and risk of bleeding in patients with atrial fibrillation (AF) is challenging. Direct oral anticoagulants (DOACs) are by now considered standard of care for treating patients with AF in international guidelines. Our objective was to assess the safety of long-term intake of DOACs in older adults with AF. We included RCTs in elderly (≥ 65 years) patients with AF. A systematic search in MEDLINE and EMBASE was performed on 19 April 2022. For determination of risk of bias, the RoB 2 tool was applied. We pooled outcomes using random-effects meta-analyses. The quality of evidence was assessed using GRADE. Eleven RCTs with a total of 63,374 patients were identified. Two RCTs compared apixaban with either warfarin or aspirin, four edoxaban with either placebo, aspirin, or vitamin K antagonists (VKAs), two dabigatran with warfarin and three rivaroxaban with warfarin. DOACs probably reduce mortality in elderly patients with AF (HR 0.89 95%CI 0.77 to 1.02). Low-dose DOACs likely reduce bleeding compared to VKAs (HR ranged from 0.47 to 1.01). For high-dose DOACS the risk of bleeding varied widely (HR ranged from 0.80 to 1.40). We found that low-dose DOACs probably decrease mortality in AF patients. Moreover, apixaban and probably edoxaban are associated with fewer major or clinically relevant bleeding (MCRB) events compared to VKAs. For dabigatran and rivaroxaban, the risk of MCRB varies depending on dose. Moreover, subgroup analyses indicate that in the very old (≥ 85) the risk for MCRB events might be increased when using DOACs.
Registration: PROSPERO: CRD42020187876.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Balancing stroke prevention and risk of bleeding in patients with atrial fibrillation (AF) is challenging. Vitamin K antagonists (VKA) have been the main treatment for stroke prevention in AF patients in the past. However, the huge inter-individual variability of the clinical response, the necessity of monitoring the INR (International Normalized Ratio) and the quite unmanageable spectrum of food and drug interactions are major disadvantages of VKAs [1].
In the last decade, various direct oral anticoagulants (DOACs) entered the market which aimed to overcome these disadvantages. Randomized controlled trials (RCTs) on DOACs, namely rivaroxaban, apixaban, dabigatran, and edoxaban have shown a positive benefit-risk profile [2,3,4,5,6,7,8,9]. DOACs are by now considered the standard of care for treating patients with AF in international guidelines [10, 11].
Various patient related factors, in particular renal dysfunction, hepatic impairment and body weight can impact the pharmacokinetics of DOACs and consequently the risk for adverse events, such as major bleeding [12]. Studies under routine care conditions indicate that the real-world population differs from the one in RCTs with respect to these characteristics. These differences could have a significant impact on the benefit-risk ratio of DOACs [13]. Most conspicuous is that the population in real-world data-based studies is about ten years older than in RCTs [14,15,16,17,18]. As pharmacokinetics of DOACs are different in older adults when compared to younger patients, safety analysis of DOAC use in the elderly is of major interest [19].
A systematic review of RCTs and observational studies suggest superior effectiveness and similar safety of DOACs compared to VKAs and that apixaban probably has the best safety profile in geriatric patients (≥ 75 years) [20]. Likewise, recent observational studies based on real-world data suggest that DOACs are not associated with an increased bleeding risk compared to VKAs but results appear to depend on the specific DOAC and are heterogeneous across countries [14,15,16,17,18].
RCTs on safety outcomes of different DOACs and dosages in older adults would be desirable. However, considering the large sample size needed to adequately power such trials, it appears unlikely that such trials will be performed in the future. This is probably also the reason why existing evidence on the safety of DOACs in older adults mainly stems from observational study designs and indirect comparisons. These are generally at risk for confounding bias. Noticeably, confounding by indication for safety outcomes would mean that patients at higher risk for adverse events when using DOACs would have a lower chance to get a DOAC prescribed and consequently would mean a bias towards the null effect, i.e. would suggest no safety concerns [21].
Therefore, our objective was to assess the safety of long-term intake of DOACs in older adults with AF. Our analyses are based on data from RCTs or subgroup analyses from RCTs on older adults (≥ 65 years) to increase the applicability of the results to patients in routine care.
Methods
We registered the protocol for this review in PROSPERO: CRD42020187876. All changes to the protocol are explicitly reported in the methods section.
This systematic review was performed according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [22] and follows the reporting recommendations of the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [23].
Eligibility criteria
Participants
Eligible participants must be diagnosed with atrial fibrillation (AF) and above the age of 65 years. We operationalized the age criterion as follows:
-
≥ 80% of the randomized population aged ≥ 65 years.
-
Subgroup analysis reports on participants aged ≥ 65 years.
Intervention
The intervention group must be treated with any type of non-vitamin K antagonist oral anticoagulant. These include:
-
apixaban
-
dabigatran
-
edoxaban
-
rivaroxaban
We only included trials with long-term DOACs treatment, defined as a treatment duration of at least 12 months. This criterion was added during study selection because different from our expectation, we recognized that in some, mainly early phase RCTs DOACs treatment was very short, which is not comparable to routine care. Any dose or regimen was eligible. Trials on DOACs not approved in the European Union before 2020 (e.g., ximelagatran, darexaban, or letaxaban) were excluded.
As comparator, we accepted any active control such as conventional anticoagulation treatment, and no treatment, or placebo treatment. Furthermore, additional antithrombotic treatment in combined regimens (i.e. antiplatelet therapy in addition to warfarin) had to be the same in all groups, so that the groups only differed regarding DOACs treatment.
Outcomes
We prioritized all-cause mortality, all-cause hospitalization, and major or clinically relevant bleeding (MCRB) as primary outcomes (critical outcomes in GRADE). Secondary outcomes were any adverse event, discontinuation due to adverse events, renal failure, delirium, and falls (important outcomes). In addition, we extracted data on bleeding according to organ system classification.
We did not consider stroke or systemic embolism because we expected that the effectiveness of DOACs for reducing stroke is stable across age groups [24, 25] and consequently the subgroup effect of age would not shift the benefit-risk ratio.
Types of studies
Only RCTs or subgroup analyses of RCTs on the relevant age group were eligible.
Publication status
We only included trials published in English or German or with data available in an English language trial registry.
Information sources
The identification of relevant literature comprised two stages.
First, we searched the reference lists of all systematic reviews included in a previous overview of reviews conducted by the research group of one member of our review team [24].
Second, we updated the electronic literature searches used in the aforementioned overview. For this purpose, MEDLINE, MEDLINE in Process, and Embase (all via Embase) were searched for studies published from 1st June 2014 (the last search of previous overview) onwards. We ran the last search on 19th April 2022.
In addition, we searched the reference lists of all included RCTs and systematic reviews on the same topic. Moreover, we searched ClinicalTrials.gov for ongoing and unpublished trials on 30 June 2020.
Search strategy
The search strategy was prepared by an experienced information specialist in collaboration with clinical experts. The search terms used were e.g. aged, atrial fibrillation, or anticoagulant agent. The full search is presented in supplement I. The search was limited to English and German. In addition, we limited the search to articles and reviews (i.e., excluded conference abstracts) and excluded case reports, in vitro studies and animal experiments. The search included a search filter for the elderly, a modified generic search filter (in addition to specific terms such as bleeding or mortality) for adverse events and a validated search filter for RCTs [26,27,28]. The search strategy was reviewed by a second person using the PRESS-checklist and validated by checking if clearly eligible RCTs already known would have been identified [29].
Selection process
Two reviewers independently screened the titles and abstracts of all records identified by the literature search. Next, full-text articles of potentially relevant reports were retrieved and assessed for compliance with the eligibility criteria by two reviewers independently. Disagreements between reviewers were resolved by discussion until consensus.
Multiple reports of the same RCT were merged, so that each trial is the unit of analysis. The study selection process was summarized in an updated PRISMA flow diagram [23].
Data collection process
Descriptive data were extracted by one reviewer and checked for accuracy by a second reviewer. Two reviewers independently identified relevant outcome data by marking the section in the relevant source. Subsequently, one reviewer extracted the data, and a second reviewer checked for accuracy. All disagreements were resolved in discussions until consensus.
In case of missing data or inconsistent data on primary outcomes in different sources, we contacted the corresponding author by e-mail.
Data items
Supplement II lists all items for which we extracted data.
We extracted data on outcomes for the last available follow-up, i.e. the longest observation period.
Supplemental to the outcome data, we extracted data on within study subgroup analyses. We only extracted data if the relevant subgroup analysis was pre-specified and a test of interaction was used to quantify the statistical certainty of the subgroup effect [30].
Study risk of bias assessment
We assessed the risk of bias with the revised Cochrane risk-of-bias tool for RCTs (RoB 2 tool) [31]. The RoB 2 tool provides a framework for assessing the risk of bias for one particular outcome that is for each outcome separately.
Effect measures
All considered outcomes were dichotomous. We extracted relative risk ratios from regression analyses (e.g., hazard ratios from a survival analysis) with 95% CIs. If these were not available (e.g., data from trial registries), we extracted raw data on events and number of participants for each group and calculated relative risks.
Synthesis methods
Statistical synthesis method
We pooled data only if RCTs were sufficiently clinically and methodologically homogenous and the p-value of the statistical test for heterogeneity was > 0.05. To describe statistical heterogeneity, we calculated prediction intervals and I-square.
We pooled adverse event data separately for each comparator (VKAs, aspirin only, placebo) and dose because we assumed, they would have different risks, in particular for bleeding. We calculated systemic adverse events across AF patients (AF-only patients) and AF patients who had a percutaneous coronary intervention (AF-PCI patients), provided the patients were clinically comparable otherwise (e.g. renal function, comorbidity).
Mortality and hospitalization are composite outcomes, to be concrete measures that combine benefits (e.g. stroke reduction) and harms (e.g. bleeding). Therefore, for mortality and hospitalization we combined different comparators because we were interested in the net benefit of DOACs compared to all possible treatments that are applied in routine care. Moreover, we pooled mortality and hospitalization separately for AF and AF-PCI patients because the benefits of DOACs (e.g., stroke prevention) likely differ between AF and AF-PCI patients.
We derived the log standard errors, which are necessary for meta-analysis from the 95% confidence intervals (95% CIs). If more than one distinct subgroup for older adults was available (e.g. 65–74 years and ≥ 75 years), we pooled the results within one RCT using fixed effect meta-analysis. To combine different RCTs, we performed inverse variance random effects meta-analyses using the Hartung-Knapp method and the Paule–Mandel heterogeneity variance estimator [32, 33]. For outcomes for which only sparse data were available (event rate < 5%, zero event studies, less than four RCTs in meta-analysis) we planned to use beta-binomial regression models for sensitivity analyses [34, 35].
We used the R-Package Meta in R 9.4 for the meta-analyses [36]. In case of heterogeneity, we synthesized results across RCTs presenting range of effects of the point estimate of the relative risk ratio.
Subgroup analyses for exploring heterogeneity
We expected that our primary analyses would be mainly based on data from subgroup-analyses, and we had therefore not planned to perform subgroup analyses. However, in some meta-analyses there was statistically significant heterogeneity, and therefore we performed post-hoc subgroup analyses on study level according to agent.
Sensitivity analyses
We planned to perform a sensitivity analysis excluding RCTs at high risk of bias in the randomisation domain.
Reporting bias assessment
We planned to assess publication bias by visual inspection of funnel plots for asymmetry, if at least 10 trials for each outcome were available.
We expected adverse events and mortality to be assessed in all RCTs. We considered RCTs/publications specifically on older adults in which mortality, overall adverse events, or discontinuation due to adverse events were not reported (and for which we got no information in response to author requests) susceptive for reporting bias. Bias in selection of the reported results within one trial is a domain of the RoB 2 tool (see above). In the RoB 2 assessment, we compared the list of outcomes reported in the protocols or methods section with the outcomes reported in the published paper.
Certainty of evidence assessment
We rated the certainty of the body of evidence using the GRADE approach (Grading of Recommendations, Assessment, Development and Evaluation). In the GRADE system evidence from RCTs starts as “high-certainty” and the following criteria are applied for downgrading the certainty of evidence by one or two levels [37]:
-
Risk of bias
-
Imprecision
-
Inconsistency
-
Indirectness
-
Publication bias
The rating of these criteria leads to four levels of the certainty of evidence for each of the prioritized outcomes [38]:
-
High-certainty evidence: the review authors have a lot of confidence that the true effect is similar to the estimated effect.
-
Moderate-certainty evidence: the review authors believe that the true effect is probably close to the estimated effect.
-
Low-certainty evidence: the review authors believe that the true effect might be markedly different from the estimated effect.
-
Very low-certainty evidence: the review authors believe that the true effect is probably markedly different from the estimated effect.
One reviewer judged the certainty of the evidence and a second reviewer verified the assessment. Disagreements were resolved by discussion until consensus.
The certainty of evidence and results are presented in 'Summary of Findings' (SoF) tables [39]. The SoF tables were prepared using GRADEpro GDT [40]. For estimating the absolute effect, we used absolute risks for the control group based on publications thought to be representative for routine care in Western countries [15, 16, 18]. If we could not find a suitable publication for one outcome, we used the risk of the comparator group of included RCTs.
To report the findings in consideration of the certainty of evidence, we used the standardized informative statements suggested by the GRADE working group [41].
The certainty of evidence is expressed with the following statements:
-
High-certainty: reduces/increases outcome
-
Moderate-certainty: “likely/probably” reduces/increases outcome
-
Low-certainty: “may” reduce/increase outcome
-
Very low-certainty: the evidence is uncertain
Results
Study selection
Figure 1 shows the study selection according to the PRISMA statement [23]. The initial screening of publications included in the previously published overview [24] identified 87 potentially relevant RCTs (based on 111 trial reports) of which we screened full-text versions. The update electronic search provided a total of 1657 citations after duplicate removal. Titles/abstracts of these were screened and 82 potentially eligible study reports were identified. The screening of full-text publications yielded eleven RCTs (reported in 20 publications) which met all eligibility criteria [2,3,4,5,6,7,8,9, 42,43,44]. The search in ClinicalTrials.gov and the screening of reference lists of included RCTs and relevant systematic reviews did not lead to additional inclusions. A list of excluded studies and the primary reason for exclusion are provided in Supplement III.
We contacted nine authors by e-mail for additional information. Four authors responded, and one provided additional numerical data [45]. In addition, we received results of an analysis of subgroup effects from an individual patient data (IPD) meta-analysis of five of the included RCTs, in response to an author request [2,3,4,5,6, 46].
Study characteristics
The eligible RCTs/subgroup analyses of RCTs (in the following all only called RCTs), included 63,374 participants in total. Table 1 shows the characteristics of the included RCTs (for detailed characteristics see supplemental Table IV).
Six RCTs (ARISTOTLE [2, 47], AVERROES [3, 48], ELDERCARE [43], ENGAGE [4, 49, 50], RE-LY [5, 51], and ROCKET [6, 52]) included any patient with AF and three trials (RE-DUAL [7, 53], PIONEER [8, 9], and ENTRUST [42]) were conducted in AF-PCI patients [54]. One RCT was conducted in participants with nonvalvular AF on haemodialysis due to end-stage renal disease (Valkyrie [45]) and one RCT (ENVISAGE) in AF patients after transcatheter aortic-valve replacement (TAVR) [44].
The median or mean age was 70 years or older. All RCTs included more men than women. In all RCTs, a significant proportion of the study population had an increased risk of bleeding and suffered from reduced renal function. Average BMI/weight was above the normal in most studies but does not reach severe obesity in any RCT.
Two RCTs compared apixaban with either warfarin or aspirin [2, 3], four edoxaban with either placebo, aspirin, or VKA [4, 42,43,44], two dabigatran with warfarin [5, 7] and three rivaroxaban with warfarin [6, 8, 45]. In the PCI trials, the patients were treated with antiplatelets in addition to oral anticoagulants [7, 8, 42].
All trials were funded by the pharmaceutical industry.
Risk of bias of included RCTs
Figure 2 contains the risk of bias assessment for each individual RCT. Results are presented on study level (not outcome level) because in none of the RCTs the risk of bias differed for different outcomes (e.g., bleeding and falls). For five RCTs we assessed the overall risk of bias to be low [45, 47, 49, 51, 52] and for five RCTs we had some concerns regarding the overall risk of bias [9, 42, 43, 48, 53]. One study was rated to be at high risk of bias [44].
Bias due to missing evidence
We could not prepare funnel-plots because none of the meta-analyses included at least ten studies. Three publications focused on the elderly but did not report mortality or any adverse event, although this could be expected [49, 52, 53].
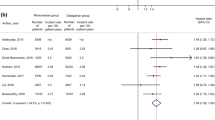
Effects of DOACs on the elderly
The results of the meta-analyses and of each individual RCT included in the meta-analyses are shown in the forest-plots (Fig. 3 Mortality AF (n = 20.904), Fig. 4 Major bleeding low dose (n = 24.997) and supplemental Fig. I). Results of the syntheses with certainty of evidence ratings are presented in the Summary of Findings (Table 2). The RCTs that were not included in the meta-analyses, because they did not match any pre-specified comparison, or because of clinical heterogeneity are presented in supplement V.
Mortality
DOACs probably reduce mortality in elderly patients with AF-only (HR 0.89 95%CI 0.77 to 1.02) [7, 43, 44, 47, 48, 51]. Likewise, in the Valkyrie trial, end stage-renal disease patients with AF receiving low-dose rivaroxaban had numerically lower mortality compared to patients receiving VKAs (RR 0.82 95%CI 0.46 to 1.45) [45]. We could not find any RCT that reported mortality in elderly AF-PCI patients.
Major or clinically relevant bleeding
In the meta-analyses, there was statistically significant heterogeneity and therefore the results were not pooled across all included RCTs [9, 42, 44, 47, 49, 51,52,53]. This was true for both, the meta-analysis on low-dose and on high-dose DOACs. To explore this heterogeneity, we performed post-hoc subgroup analyses. We decided to stratify the analyses according to dose and agent because previous systematic reviews and large real-world studies had suggested that dabigatran and rivaroxaban tend to have a higher bleeding risk than apixaban and edoxaban [13, 15, 16, 18, 20, 55].
For low doses, the separate analyses according to agents did not resolve heterogeneity [9, 47, 49, 51, 53]. A common quantitative measure would therefore be misleading and consequently no meta-analysis was performed, and we only compiled a narrative synthesis. According to this, low-dose DOACs likely reduce bleeding compared to VKAs (HR ranged from 0.47 to 1.01). Likewise, in end-stage renal disease patients, low-dose rivaroxaban decreased major bleeding risk numerically compared to VKAs (RR 0.58 95%CI 0.25 to 1.34) [45]. In the ELDERCARE trial low-dose edoxaban increased major bleeding numerically compared to placebo (HR 1.87 95%CI 0.90 to 3.89) [43]. In the AVERROES trial, apixaban increased major bleeding risk numerically compared to aspirin, but 95%CIs overlapped appreciable benefit and harm (1.21 95%CI 0.69 to 2.12) [48].
For high-dose DOACs, the distinct meta-analyses according to agent did not resolve heterogeneity, and we only performed a narrative synthesize. The risk of major bleeding varied widely (HR ranged from 0.80 to 1.40) [42, 44, 49, 51,52,53].
Subgroup considerations
Table 3 shows the results of the within study subgroup analyses for age. The subgroup analyses indicate that the positive effect on mortality in favour of DOACs might decrease with age. The MCRB risk appears to increase with age, whereby the effect direction in favour of DOACs might reverse in very old people (about 85–90 years). Noticeable, in our meta-analyses of high-dose DOACs the bleeding risk tended to be higher in studies that included older or more morbid patients [42, 44, 49, 51,52,53]. This was even true for studies on the same agent.
Subgroup analyses for major bleeding according to all AF patients versus AF-PCI patients [8, 42, 53] do not change the results (data not shown). An explorative analysis of bleeding risk according to body part suggested that DOACs increase the risk of gastrointestinal bleeding but reduce the risk of intracranial bleeding numerically (data not shown).
Secondary outcomes
Apixaban likely reduces overall hospitalisations (HR 0.84 95%CI 0.76 to 0.93) [47, 48]. In the ELDERCARE trial the difference in hospitalizations was negligible (RR 1.02 95%CI 0.67 to 1.58) [43]. Discontinuations due to adverse events, were numerically slightly increased in patients taking VKAs compared to edoxaban but the effect is uncertain because of statistical imprecision (RR 1.12 95%CI 0.58 to 2.15) [43, 44].
We did not find any RCT that reported on hospitalisations in AF-PCI patients. There is no evidence from RCTs on overall adverse events, renal failure, falls or delirium in elderly patients with AF treated with DOACs.
Sensitivity analyses
We performed no sensitivity analysis according to risk of bias because none of the RCTs was assessed to be at risk of bias in the randomisation domain.
Sensitivity analyses of meta-analyses including < 4 RCTs and few numbers of events were not possible because the beta-binomial model is a one-stage model, which requires data that allow to reconstruct a contingency table, but for almost all RCTs only aggregated data (e.g., HRs) were available.
Discussion
Summary and interpretation in consideration of other evidence
Our systematic review on safety outcomes shows that DOACs probably reduce mortality in elderly AF-only patients to a larger extent than VKAs. The findings were consistent across different agents and different doses agree with previous results of RCTs on all age groups, which suggests that the global effectiveness of DOACs in AF is not significantly influenced by age and a positive benefit-risk ratio of DOACs in comparison to VKAs does also exist in the older population with AF-only [13, 25, 46]. Likewise, the effects seem consistent across different DOACs [56]. In the population with AF, the lower risk for bleeding in the low-dose treatment groups is apparently not counterbalanced by a higher risk for lethal thromboembolic events. In the high-dose treatment groups a significantly higher bleeding risk seems to exist for dabigatran and rivaroxaban, which might be explained by the different extent of renal elimination. The major bleeding risk for edoxaban was not consistent. In the ENGAGE and ENTRUST trials the bleeding risk using DOACs was reduced compared to VKAs. In contrast, in the ENVISAGE study the risk was increased [42, 44]. This finding might be explained by the higher average age and higher cardiovascular morbidity compared to both other studies.
We found no RCT that reported on mortality for AF-PCI patients, however meta-analyses in the entire population, i.e. not only elderly, showed that mortality in the DOACs group was not statistically significantly higher than in the VKA group [42, 57]. Apparently, in this population, the approach of combining DOACs with only one antiplatelet agent (instead of dual antiplatelet therapy = DAPT) in comparison to the efficacy and safety with VKA plus DAPT results in a lower risk for bleeding, but a higher risk for thromboembolic or coronary events.
Studies based on real-world data showed heterogeneous results for mortality when using DOACs compared to VKAs in AF patients [14,15,16,17]. The studies neither distinguished between AF-only and AF-PCI patients nor patients with different heart disease severity in general. Remarkably, in these observational studies, morbidity due to cardiovascular diseases was high and more similar to the PCI population than to the AF-only population in our review. The differences in morbidity, in particular the probable differences in proportion of PCI-patients, might be one explanation for the heterogeneous results for the effectiveness of DOACs in studies based on real-world data and also for the tendency of a weaker impact of DOACs on mortality under routine conditions compared to the RCTs on AF-only patients [14, 15, 57].
Another explanation for the heterogeneous findings could be the type of VKA used. In large real-world studies performed in the USA and Denmark, taking DOACs was associated with fewer deaths compared to VKAs [16, 17]. In contrast, similar studies performed in Germany showed higher mortality compared to VKAs [15]. The reason for this difference could be the different VKA prescribing practices; in the USA, warfarin is mainly, whereas phenprocoumon is prescribed in Germany. Pharmacological studies showed that for long-term use, phenprocoumon is preferable compared to warfarin because phenprocoumon patients more often have an INR in the therapeutic range [58]. Conspicuously, the patterns of mortality and major bleeding risk appear to agree, concrete studies showing higher major bleeding risk tend to show less favourable results for mortality, indicating that at least a part of the differences in mortality might be explained by death as a result of major bleeding. However, to our knowledge no RCTs exist that directly compare phenprocoumon to warfarin.
We found that low-dose DOACs probably decrease MCRB compared to VKA in AF-only and similarly in AF-PCI patients but could not quantify this reduction reliably because of statistical heterogeneity. The heterogeneity could neither be fully explained by subgroup analyses of patient type (AF-only vs. AF-PCI) nor by subgroup analysis on drug type. All but one RCT showed reduced MCRB and in one RCT the bleeding rates were comparable between DOACs (dabigatran) and warfarin. In the two RCTs on low-dose dabigatran, the PCI trial showed lower major bleeding risk using dabigatran compared to warfarin, which is probably explained by the concomitant therapy with only one antiplatelet agent in the DOACs group and DAPT in the warfarin group. Consistent with real-world studies, edoxaban and even more apixaban showed the lowest risk for MCRB while heterogeneity is large [15, 16, 56].
Preliminary evidence, showed numerically more MCRB when taking low-dose DOACs compared to aspirin and placebo in AF-only patients [43, 48]. Furthermore, the RCT of low-dose rivaroxaban in AF-only patients with end-stage renal disease provides a hint that the results for MCRB in this population might be similar to the results in the elderly in general, meaning that the current evidence from RCTs does not indicate that in patients with end-stage renal disease DOACs should not be prescribed in general [45].
For high-dose DOACs the MCRB risk seems to depend on the agent. This seems to be true both for AF-only and AF-PCI patients. Rivaroxaban and dabigatran increased the bleeding risk. Again, the real-world studies found heterogeneous results for these drugs [14,15,16,17,18]. However, it must be considered that the impact of different doses of DOACs was not analysed in these observational studies. Considering that the quality of evidence for our findings is high and considering results of previous analyses on the influence of dosing, it appears plausible that the different doses are an additional important explanation for the heterogeneous findings on safety of DOACs in the real-world [13]. For high-dose edoxaban, MCRB risk was very heterogeneous. One explanation could be the higher age and morbidity in the ENVISAGE trial, compared to all other trials [44].
Applicability of findings
Comparing our study population to the patient population from real-world studies confirmes that our population mirrors the patients in routine care quite well. Therefore, none of the RCTs was down-graded due to limited applicability in the certainty of evidence assessment. Notwithstanding, the AF-only patients still tend to be less morbid and comorbid than patients in real-world studies [14,15,16,17,18, 59]. Moreover, all but two studies that compared DOACs to VKAs used warfarin whereas in some countries other VKAs are mainly prescribed, which limits applicability of the results to these countries [60].
Quality of the evidence
The risk of bias of the body of evidence was low. The main limitation of the certainty of evidence for mortality was statistical imprecision. In each individual study, DOACs were at least as effective as VKAs in preventing mortality but effect sizes apparently varied. Although the difference in effectiveness between studies might be simply due to random error, we could not exclude that this is due to the different DOACs. In addition, for low-dose DOACs, the certainty of evidence on MCRB is limited by unexplained heterogeneity.
The evidence in this systematic review is incomplete regarding several safety outcomes including overall adverse events, adverse events leading to discontinuation, and adverse events particularly relevant for the elderly such as delirium or falls.
Limitations
One limitation of this systematic review is the literature search. We decided to identify the evidence using previous systematic reviews to speed up the review process. We anticipated that this is a reasonable shortcut considering the very huge number of systematic reviews on DOACs and therefore low risk of missing relevant literature when relying on previous systematic literature searches. In addition, some might argue that the findings are limited because a large part of them stems from subgroup analyses from RCTs on elderly. However, most of the RCTs were very large and additionally stratified the randomisation for age and adjusted the analyses for important prognostic factors. Therefore, it seems improbable that this approach has introduced bias.
Conclusion
Implications for research
There is an important research gap on overall adverse events and particularly outcomes that are relevant for older adults such as falls, fractures or renal impairment in AF-patients in general [61]. In addition, for AF-PCI patients high quality data on mortality is lacking. Studies on these outcomes are necessary for sufficient balancing of the benefits and harms of DOACs use in elderly patients, especially given the low absolute mortality and MCRB risk. Moreover, patient characteristics which might explain the heterogeneity in the real-world, such as very high age, body weight, renal function, severe and multi-morbidity, should be further explored because better information on these potential predictors could contribute to an improved individualization of anticoagulation therapy.
Implications for practice
No conclusive judgement on the safety of DOACs in older adults is possible because of the lack of RCTs assessing overall adverse events and outcomes relevant in the elderly (e.g., fractures, delirium) [61]. Our data and external evidence from real-world studies suggest that the bleeding risk depends on agent, dose and age. Moreover, the impact of DOACs on mortality and hospitalization probably depends on patient type (AF-only vs. AF-PCI). Similarly to previous systematic reviews on all age groups, we found that low-dose DOACs probably decrease mortality in older AF-only patients. Moreover, apixaban and low-dose edoxaban are associated with fewer MCRB events compared to VKAs [13]. For dabigatran and rivaroxaban, the risk of MCRB varies depending on dose. Moreover, subgroup analyses indicate that in the very old (≥ 85 years) the bleeding risk of DOACs in general, but especially for dabigatran and rivaroxaban might be even higher than for VKAs. The uncertainty due to heterogeneous bleeding risk and the limited impact of DOACs on absolute mortality, suggest once again that the individual anticoagulation treatment choice should cautiously balance the individual patient’s benefit-risk profile, especially in the very old or morbid patient.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AF :
-
Atrial fibrillation
- DOAC :
-
Direct oral anticoagulants
- MCRB :
-
Major or clinically relevant bleeding
- PCI :
-
Percutaneous coronary intervention
- RCT :
-
Randomised controlled trial
- TAVR :
-
Transcatheter aortic-valve replacement
- VKA :
-
Vitamin K antagonists
References
Mekaj YH, et al. New oral anticoagulants: their advantages and disadvantages compared with vitamin K antagonists in the prevention and treatment of patients with thromboembolic events. Ther Clin Risk Manag. 2015;11:967–77. https://doi.org/10.2147/TCRM.S84210.
Granger CB, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92. https://doi.org/10.1056/NEJMoa1107039.
Connolly SJ, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–17. https://doi.org/10.1056/NEJMoa1007432.
Giugliano RP, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104. https://doi.org/10.1056/NEJMoa1310907.
Connolly SJ, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. https://doi.org/10.1056/NEJMoa0905561.
Patel MR, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. https://doi.org/10.1056/NEJMoa1009638.
Cannon CP, et al. Dual antithrombotic therapy with Dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017;377(16):1513–24. https://doi.org/10.1056/NEJMoa1708454.
Gibson CM, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016;375(25):2423–34. https://doi.org/10.1056/NEJMoa1611594.
Gibson CM, et al. Recurrent hospitalization among patients with atrial fibrillation undergoing intracoronary stenting treated with 2 treatment strategies of rivaroxaban or a dose-adjusted oral vitamin K antagonist treatment strategy. Circulation. 2017;135(4):323–33.
Gerhard Hindricks and others, 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612
January CT, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76. https://doi.org/10.1016/j.jacc.2014.03.022.
Chen A, Stecker E, Warden BA. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc. 2020;9(13):e017559. https://doi.org/10.1161/JAHA.120.017559.
Lopez-Lopez JA, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. 2017;359:j5058. https://doi.org/10.1136/bmj.j5058.
Gieling E, et al. Mortality risk in atrial fibrillation: the role of aspirin, vitamin K and non-vitamin K antagonists. Int J Clin Pharm. 2019;41(6):1536–44. https://doi.org/10.1007/s11096-019-00916-1.
Paschke LM, et al. Comparing stroke prevention therapy of direct oral anticoagulants and vitamin K antagonists in patients with atrial fibrillation: a nationwide retrospective observational study. BMC Med. 2020;18(1):254. https://doi.org/10.1186/s12916-020-01695-7.
Graham DJ, et al. Comparative stroke, bleeding, and mortality risks in older medicare patients treated with oral anticoagulants for nonvalvular atrial fibrillation. Am J Med. 2019;132(5):596-604 e11. https://doi.org/10.1016/j.amjmed.2018.12.023.
Larsen TB, et al. Efficacy and safety of dabigatran etexilate and warfarin in “real-world” patients with atrial fibrillation: a prospective nationwide cohort study. J Am Coll Cardiol. 2013;61(22):2264–73. https://doi.org/10.1016/j.jacc.2013.03.020.
Souverein PC, et al. Comparing risk of major bleeding between users of different oral anticoagulants in patients with nonvalvular atrial fibrillation. Br J Clin Pharmacol. 2021;87(3):988–1000. https://doi.org/10.1111/bcp.14450.
Committee for Medicinal Products for Human Use (CHMP). Assessment report INN/active substance: direct oral anticoagulants (DOACs). 26 March 2020 EMA/194375/2020 In: Assessment report, EMA, Editor. 2020. Available from: https://www.ema.europa.eu/en/documents/referral/assessment-report-article-53-procedure-direct-oral-anticoagulants-doacs_en.pdf. Accessed Sept 2020.
Grymonprez M, et al. Effectiveness and safety of oral anticoagulants in older patients with atrial fibrillation: a systematic review and meta-analysis. Front Pharmacol. 2020;11:583311. https://doi.org/10.3389/fphar.2020.583311.
Safieddine M, et al. Compared to randomized studies, observational studies may overestimate the effectiveness of DOACs: a metaepidemiological approach. J Clin Epidemiol. 2021;130:49–58. https://doi.org/10.1016/j.jclinepi.2020.10.013.
Higgins JP, et al. Cochrane handbook for systematic reviews of interventions. Wiley; 2019.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Sommerauer C, et al. Effectiveness and safety of vitamin K antagonists and new anticoagulants in the prevention of thromboembolism in atrial fibrillation in older adults - a systematic review of reviews and the development of recommendations to reduce inappropriate prescribing. Bmc Geriatrics. 2017;17(1):223.ARTN 223. https://doi.org/10.1186/s12877-017-0573-6.
Ruff CT, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0.
Wong SS, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically sound treatment studies in EMBASE. J Med Libr Assoc. 2006;94(1):41–7.
Canadian Health Libraries Association (FMD3S). Concepts de stratégies de recherche, Personnes âgées. 2018; Available from: https://extranet.santecom.qc.ca/wiki/!biblio3s/doku.php?id=concepts:personnes_agees#dokuwiki__top. Accessed Sept 2020
Canadian Health Libraries Association (FMD3S). Concepts de stratégies de recherche, Effets secondaires. 2018; Available from: https://extranet.santecom.qc.ca/wiki/!biblio3s/doku.php?id=concepts:effets-secondaires. Accessed Sept 2020
McGowan J, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
Schandelmaier S, et al. A systematic survey identified 36 criteria for assessing effect modification claims in randomized trials or meta-analyses. J Clin Epidemiol. 2019;113:159–67. https://doi.org/10.1016/j.jclinepi.2019.05.014.
Sterne JAC, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. In Cochrane Handbook for Systematic Reviews of Interventions. 2019. https://doi.org/10.1002/9781119536604.ch10.
Langan D, et al. A comparison of heterogeneity variance estimators in simulated random-effects meta-analyses. Res Synth Methods. 2019;10(1):83–98. https://doi.org/10.1002/jrsm.1316.
Mathes T, Kuss O. A comparison of methods for meta-analysis of a small number of studies with binary outcomes. Res Synth Methods. 2018;9(3):366–81. https://doi.org/10.1002/jrsm.1296.
Kuss O. Statistical methods for meta-analyses including information from studies without any events-add nothing to nothing and succeed nevertheless. Stat Med. 2015;34(7):1097–116. https://doi.org/10.1002/sim.6383.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60. https://doi.org/10.1136/ebmental-2019-300117.
Balshem H, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
Hultcrantz M, et al. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017;87:4–13. https://doi.org/10.1016/j.jclinepi.2017.05.006.
Guyatt G, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. https://doi.org/10.1016/j.jclinepi.2010.04.026.
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2022. Available from gradepro.org. Accessed Sept 2020.
Santesso N, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol. 2020;119:126–35. https://doi.org/10.1016/j.jclinepi.2019.10.014.
Vranckx P, et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet. 2019;394(10206):1335–43. https://doi.org/10.1016/S0140-6736(19)31872-0.
Okumura K, et al. Low-dose edoxaban in very elderly patients with atrial fibrillation. N Engl J Med. 2020;383(18):1735–45. https://doi.org/10.1056/NEJMoa2012883.
Van Mieghem NM, et al. Edoxaban versus vitamin K antagonist for atrial fibrillation after TAVR. N Engl J Med. 2021;385(23):2150–60. https://doi.org/10.1056/NEJMoa2111016.
De Vriese AS, et al. Multicenter randomized controlled trial of vitamin K antagonist replacement by rivaroxaban with or without vitamin K2 in hemodialysis patients with atrial fibrillation: the Valkyrie Study. J Am Soc Nephrol. 2020;31(1):186–96.
Carnicelli AP, Hong H, Giugliano RP, Connolly SJ, Eikelboom J, Patel MR, Wallentin L, Morrow DA, Wojdyla D, Hua K, Hohnloser SH, Oldgren J, Ruff CT, Piccini JP, Lopes RD, Alexander JH, Granger CB; COMBINE AF Investigators. Individual Patient Data from the Pivotal Randomized Controlled Trials of Non-Vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation (COMBINE AF): Design and Rationale: From the COMBINE AF (A Collaboration between Multiple institutions to Better Investigate Non-vitamin K antagonist oral anticoagulant use in Atrial Fibrillation) Investigators. Am Heart J. 2021;233:48–58. https://doi.org/10.1016/j.ahj.2020.12.002
Halvorsen S, et al. Efficacy and safety of apixaban compared with warfarin according to age for stroke prevention in atrial fibrillation: observations from the ARISTOTLE trial. Eur Heart J. 2014;35(28):1864–72. https://doi.org/10.1093/eurheartj/ehu046.
Ng KH, et al. Efficacy and safety of apixaban compared with aspirin in the elderly: a subgroup analysis from the AVERROES trial. Age Ageing. 2016;45(1):77–83. https://doi.org/10.1093/ageing/afv156.
Kato ET, et al. Efficacy and safety of edoxaban in elderly patients with atrial fibrillation in the ENGAGE AF-TIMI 48 trial. J Am Heart Assoc. 2016;5(5):e003432. https://doi.org/10.1161/JAHA.116.003432.
Lauw MN, et al. Effects of dabigatran according to age in atrial fibrillation. Heart. 2017;103(13):1015–23. https://doi.org/10.1136/heartjnl-2016-310358.
Eikelboom JW, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011;123(21):2363–72. https://doi.org/10.1161/CIRCULATIONAHA.110.004747.
Halperin JL, et al. Efficacy and Safety of rivaroxaban compared with warfarin among elderly patients with nonvalvular atrial fibrillation in the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF). Circulation. 2014;130(2):138-U45. https://doi.org/10.1161/Circulationaha.113.005008.
Ten Berg JM, et al. Comparison of the effect of age (< 75 versus ≥ 75) on the efficacy and safety of dual therapy (Dabigatran + Clopidogrel or Ticagrelor) versus triple therapy (Warfarin + Aspirin + Clopidogrel or Ticagrelor) in patients with atrial fibrillation after percutaneous coronary intervention (from the RE-DUAL PCI Trial). Am J Cardiol. 2020;125(5):735–43.
Lip GY, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary intervention/stenting. Thromb Haemost. 2010;103(01):13–28.
Fernandez MM, et al. Systematic review and network meta-analysis of the relative efficacy and safety of edoxaban versus other nonvitamin K antagonist oral anticoagulants among patients with nonvalvular atrial fibrillation and CHADS2 score ⩾ 2. SAGE Open Med. 2015;3:2050312115613350. https://doi.org/10.1177/2050312115613350.
Menichelli D, et al. Real-world safety and efficacy of direct oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of 605 771 patients. Eur Heart J Cardiovasc Pharmacother. 2021;7(FI1):f11–9. https://doi.org/10.1093/ehjcvp/pvab002.
Al Said S, et al. Non‐vitamin K antagonist oral anticoagulants (NOACs) post‐percutaneous coronary intervention: a network meta‐analysis. Cochrane Database Syst Rev. 2019(12). https://doi.org/10.1002/14651858.CD013252.pub2.
Beinema M, et al. Pharmacogenetic differences between warfarin, acenocoumarol and phenprocoumon. Thromb Haemost. 2008;100(6):1052–7.
Nielsen PB, et al. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510. https://doi.org/10.1136/bmj.j510.
Le Heuzey JY, et al. Differences among western European countries in anticoagulation management of atrial fibrillation. Data from the PREFER IN AF registry. Thromb Haemost. 2014;111(5):833–41. https://doi.org/10.1160/TH13-12-1007.
Thürmann PA. Clinical studies in geriatric population. In: Hock F, Gralinski M, (eds). Drug discovery and evaluation: Methods in clinical pharmacology. Cham: Springer; 2020. https://doi.org/10.1007/978-3-319-68864-0_43.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was part of the project “Updating the PRISCUS list of potentially inappropriate medications for the elderly” funded by the German Federal Ministry of Education and Research (Grant Number: 01KX1812).
Author information
Authors and Affiliations
Contributions
KD: study selection, data extraction, interpretation of results, writing of manuscript, revision of manuscript
SB: data extraction, interpretation of results, revision of manuscript
AW: study selection, data extraction, interpretation of results, revision of manuscript
NKM: interpretation of results, writing of manuscript
SH: design and conduct of electronic searches
SS: study selection, data extraction, revision of manuscript
AS: development of study concept, interpretation of results, revision of manuscript
DP: development of study concept, interpretation of results, revision of manuscript
PAT: development of study concept, interpretation of results, revision of manuscript
TM: development of study concept, study selection, data extraction, statistical analysis, interpretation of results, writing of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest/competing interests
KD, SB, AW, NKM, SH, DP, AS, DP, SS, PAT and TM declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Doni, K., Bühn, S., Weise, A. et al. Safety outcomes of direct oral anticoagulants in older adults with atrial fibrillation: a systematic review and meta-analysis of (subgroup analyses from) randomized controlled trials. GeroScience 46, 923–944 (2024). https://doi.org/10.1007/s11357-023-00825-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-00825-2