Abstract
Purpose
Disturbance to physical and psychological characteristics among COVID-19 survivors are not uncommon complications. In the current systematic review, we aimed to investigate the role of exercise rehabilitation programs, either in acute or post-acute phase, on COVID-19 patients’ outcomes.
Methods
A systematic search was conducted in November 2021 of Web of Sciences, PubMed-Medline, Google Scholar, and Scopus. Observational and intervention studies on COVID-19-infected patients undergoing a rehabilitation program including any type of exercise were included if they reported physical or psychological factors as outcomes. The Cochrane risk of bias tool for randomized controlled trials and Joanna Briggs Institute (JBI) critical appraisal checklist were used by two independent reviewers.
Results
A total number of 469, and 957 patients were included in 9 intervention studies, and 14 observational studies, respectively. Most factors reported by studies as outcomes fell in the categories of exercise capacity, respiratory function, as well as psychological aspects. The reported outcomes in almost all studies, disclosed the overall beneficial role of exercise rehabilitation in improving the outcomes.
Conclusion
The current review demonstrated that exercise rehabilitation generally could have a beneficial role in improvement of both physical and psychological related outcomes. As the best onset time, and FITT components are not yet completely clear, further large, well-designed RCTs are suggested to provide details of exercise rehabilitation program.
Similar content being viewed by others
Introduction
By the end of February 2021, more than 430 million people have been recognized as confirmed cases with SARS-CoV2 infection. In addition, after almost 2 years of COVID-19 pandemic, this ongoing public health problem has been responsible for more than 5.9 million deaths globally [1].
As the number of confirmed cases with COVID-19 increases, the pressure posed to global health and economy will become more evident [2, 3]. Not only is this due to increase in mortality, but also the result of increase in long-term health consequences among recovered cases [3].
A significant number of patients with COVID-19 suffer from prolonged symptoms [4]. Existing research indicates that patients with different age group as well as diverse severity of disease may experience persistent symptom [5].
Although the evidence suggests that efficacious and trustworthy vaccines may play a crucial role in terminating the pandemics [6], potential of high mutation rate within SARS-CoV-2 genome could make it more challenging [7]. Furthermore, long COVID still seems to exist as a significant complication of the disease [5].
Finding the most effective therapeutic interventions is still emerging with a variety of ongoing studies [8]. Besides that, it is likely, along with the primary prevention i.e., using vaccine, to combat the pandemic [7], the rehabilitation programs as a tertiary prevention could help to alleviate the huge health adverse effects due to COVID-19 [9], and to decrease the disease burden [10].
The evidence suggest that exercise could play a fundamental role in rehabilitation and restoring the normal life among COVID-19 survivors. In this sense, improvement in lung function, immunity enhancement by cytokine regulation, reduction in oxidative stress, as well as intestinal flora modulation were theoretically introduced [2]. On the other hand, inactivity has proposed as a novel risk factor for increasing COVID-19 duration [11]. In addition, sports participation was associated with lower rate of COVID-19 complication [12].
As the deterioration in physical and psychological characteristics among COVID-19 survivors are not uncommon complications [10], we aimed in this systematic review to investigate the role of exercise rehabilitation programs, either in acute or post-acute phase, on physical and psychological outcomes among COVID-19 patients.
Methods
This systematic review was undertaken using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. The protocol was registered to PROSPERO (CRD42022301087).
Search strategy
Web of Sciences, PubMed-Medline, Google Scholar, and Scopus were searched systematically between December 2019 and November 2021 in English language. The combination of (“physical activity” OR “exercise” OR “physical inactivity” OR “sedentary behavior” OR “life-style” OR “sports”) with (“COVID-19” OR “SARS-CoV-2” OR “SARS-CoV-2”) were defined as the search strategy.
Inclusion and exclusion criteria
All published observational and intervention studies on COVID-19-infected patients undergoing an exercise rehabilitation program were included if they met the following inclusion criteria: 1—Studies conducted on patients with confirmed diagnosis of COVID-19 regardless of the severity, either with or without comorbidity. 2—Rehabilitation programs included any type of exercise regardless of onset time, and duration of program. 3—Studies have reported either physical or psychological factors as outcome. All other study types (e.g., case reports, case series, qualitative, reviews, commentaries and editorials) were excluded.
Eligibility and data extraction
The title and abstract of studies, found based on the above strategy, were screened by two independent investigators (FH & BM) and a third one (MS) as consultant in specific disagreement cases. Full texts of eligible studies were reviewed.
The previously designed data extraction sheet including the name of first author, study design, sample size, methodology, sex and age range of patients, onset and type of rehabilitation, outcome definition and assessment time was used.
Quality assessment
For intervention and observational studies, the Cochrane risk of bias tool for randomized controlled trials [14] and Joanna Briggs Institute (JBI) [15] critical appraisal checklist were used, respectively. Two independent reviewers (BM & BT) were involved in quality assessment.
Results
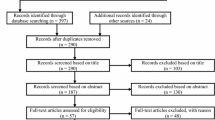
As seen in Fig. 1, 5035 studies were identified initially through Web of Sciences, PubMed-Medline, Google Scholar, and Scopus databases. After duplicate removal, 3332 studies were remained. Title/abstract screening excluded another 3245 studies and 87 studies were selected for full-text review. Finally, 23 studies including fourteen observational and nine intervention studies met the inclusion criteria. Most factors reported by studies as outcomes fell in the categories of exercise capacity, respiratory function, as well as psychological aspects.
Risk of bias assessment revealed variation in scores of different domains through all studies. Table 1 and Fig. 2 illustrate the results of quality assessment of observational, and intervention studies, respectively. Results of The Risk of Bias VISualization (ROBVIS) [16] was utilized to demonstrate the results of quality assessment of intervention studies.
Intervention studies
A total number of 469 patients were included in nine intervention studies [17,18,19,20,21,22,23,24,25] (Table 2). The duration of rehabilitation programs was within the range of 5–42 days. Acute and post-acute rehabilitation were considered in six and three studies, respectively.
According to the National Institute for Health and Care Excellence (NICE), acute and post-acute phases were defined as within the first 4 weeks of symptoms onset, and more than 4 weeks of symptoms onset, respectively [26]. However, acute phase was considered as the first 40 days of symptoms onset in studies by Gonzalez-Gerez et al. [18], and Rodriguez-Blanco et al. [24]. This discrepancy was due to problems related to diagnostic testing caused by collapses in their health systems.
The reported outcomes in eight studies of nine disclosed the overall beneficial role of exercise rehabilitation in improving the outcomes.
Five studies by Gonzalez-Gerez et al. [18], Liu et al. [21], Mohamed et al. [22], Ozlu et al. [23], and Rodriguez-Blanco et al. [24] demonstrated the beneficial effects of acute exercise rehabilitation among COVID-19 patients. The reported severity was within mild to moderate in these studies.
In studies by Abodonya et al. [17], Liu et al. [20], and Tang et al. [25] exercise rehabilitation in post-acute phase was significantly effective in improving the physical (including both exercise capacity, and respiratory function) and psychological outcomes among the patients with either mild-to-moderate severity or severe to critically ill.
Andre et al. revealed that inpatient rehabilitation (including unsupervised physical activity) among older hospitalized patients with COVID-19 was ineffective to improve neither exercise capacity nor psychological aspects [19].
Rehabilitation and exercise capacity
Six minutes’ walk test (6MWT), and thirty-second sit-to-stand test (30STS) were the most common tests evaluated as exercise capacity in included studies. The results demonstrated a significant improvement in favor of rehabilitation group. Sit to stand test, semi-tandem and side by side stand, as well as walking speed were considered as outcomes in study by Andre et al. [19] They have not reported significant difference between two groups.
Rehabilitation and respiratory function
Spirometry outcomes and dyspnea scale were considered as the most common outcomes. Spirometry-related factors consisted of force expiratory volume in one second (FEV1), forced volume capacity (FVC), FEV/FVC%, and transfer factor for lung carbon monoxide (TLCO%). Borg scale and modified Medical Research Council (mMRC) were considered as dyspnea scale in two and one studies, respectively. All factors were significantly improved in favor of rehabilitation group.
Rehabilitation and psychological aspects
Outcomes in this field generally were related to the quality of life, anxiety, and depression measured via questionnaire-based approach.
Other outcomes
Only in one study, blood immune markers including leukocytes, lymphocytes, interleukins, IgA, and TNF-alpha were considered as outcomes. Although only changes in leukocytes, lymphocytes and IgA were reached statistical difference, improvement in all investigated factors was seen. All differences were in favor of exercise rehabilitation except TNF-alpha [22].
Observational studies
A total number of 957 patients were included in 14 observational studies [27,28,29,30,31,32,33,34,35,36,37,38,39,40] (Table 3).
The duration of rehabilitation programs was within the range of 1–42 days. Acute and post-acute rehabilitation were considered in five and nine studies, respectively. The reported outcomes in all studies disclosed the overall beneficial role of exercise rehabilitation in improving the outcomes. All types of disease severity from mild to severe and critically ill patients were included in the studies. Only one study dealt with the rehabilitation of patients with persistent symptoms.
Rehabilitation and exercise capacity
Factors related to aerobic capacity, as well as strength and balance capacity were measured as outcomes in this field. Aerobic capacity-related factors, including 6MWT, shuttle test, cardio-pulmonary exercise test (CPET), sit to stand score (STSS), step test score (STS), and 10-m walk test were measured in seven studies. Significant improvement in hand grip and quadriceps muscle strength reported in cohort and cross-sectional studies on 21, and 22 patients with severe–critically ill COVID-19, respectively. Tinetti balance test, Berg Balance Scale, Short Physical Performance Battery (SPPB), and Barthel Index (BI) were considered as balance factors in included studies. The overall results demonstrated significant improvement in favor of rehabilitation groups.
Rehabilitation and respiratory function
Dyspnea scores including Borg dyspnea scale, and spirometry factors including FEV1%, FVC%, total lung capacity (TLC), diffusing capacity for carbon monoxide (DLCO), maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP), P/F ratio, peak expiratory flow rate (PEFR), maximum inspiratory pressure (PImax), maximum expiratory pressure (PEmax), as well as acute symptoms and oxygen requirement were considered as parameters of respiratory function in included observational studies.
Rehabilitation and psychological aspects
Questionnaire-based measurement of quality of life, anxiety, and depression were generally regarded as psychological outcomes. Improvement in psychological aspects were observed in all studies, although statistical significance was not reached in some studies.
Discussion
The current systematic review aimed to figure out the role of exercise rehabilitation on COVID-19 patients’ outcomes. Results of included studies generally have revealed the benefits of exercise rehabilitation. Overall, both physical and psychological related outcomes have improved by exercise rehabilitation.
The results are contrary to that of Connoly et al. who found that the benefit of post-discharge exercise-based rehabilitation on exercise capacity and health-related quality of life among 483 ICU survivors were inconclusive [41], but are broadly consistent with earlier systematic review study conducted by Goodwin et al., which has postulated that exercise and mobilization could have a substantial role in improving the outcomes among critical care admitted patients with severe respiratory illness. As they generalized the results to the cases with COVID-19 infection, they have concluded that exercise could make a significant contribution to improve the physical outcomes. However, their finding regarding quality of life was under debate [42].
In a 2022 study by Barman et al., respiratory rehabilitation including either aerobic or respiratory muscle training has a positive effect on exercise capacity as well as pulmonary function among patients with Severe Acute Respiratory Syndrome (SARS) [43]. With respect to the minimal clinically important difference (MCID) of 20–30 m established for 6MWD, analysis of pooled data in the mentioned study revealed that 6MWD as a valid tool to determine the exercise capacity had been improved significantly higher than MCID. [43] The amount of such increase in all included studies were higher than previously reported MCID except in study by Tang et al. [25]
It is worth noting that a wide variety in the rehabilitation onset were used in included studies in our review. Although most of intervention studies focus on acute rehabilitation, post-acute rehabilitation was considered as a dominant approach in observational studies.
It seems there is still big controversy over the appropriate time of rehabilitation onset among COVID-19 patients. Chinese and Italian societies of rehabilitation did not recommend acute rehabilitation due to probable decrease in oxygen blood saturation [44, 45]. A similar conclusion was reached by Demeco et al. [46] In their study, severe and critically ill patients were recommended to postpone the respiratory rehabilitation until their status become more stable. In contrast, the results of the study by Goodwin et al. focusing on acute rehabilitation in critical care setting were pleasant [42].
The results of the current review revealed that acute rehabilitation in either mild to moderate [18, 21, 22, 24, 39, 40] or severe patients [8, 23, 29, 36] were associated with successful outcomes.
In addition, components of exercise prescription including frequency, intensity, time and type (FITT) were broadly varied through the studies. It is not yet completely clear what FITT components are of interest to COVID-19-affected patients.
Wittmer et al. have sounded a note of caution on exercise prescription for COVID-19 patients [47]. They concluded that exercise intensity must be adapted according to clinical status and stage of illness. Neither too much to be problematic nor too little to be ineffective. The challenges to determine the intensity are twofold. First, it should be compatible with patients with muscle strength decrement [48]. Second, the intensity should not be as vigorous as it poses a further pressure to respiratory system for the reason that SARS could happen to some mild-moderate patients [49].
The results of observational studies included in study by Wittmer et al. demonstrated that low-to-moderate intensity and low intensity were associated with good results in mild, and moderate COVID-19 patients, respectively. Early mobilization was also related to better prognosis in severe to critical COVID-19 patients [47]. Similarly, included studies in our review revealed that progressive mild-to-moderate intensity could bring positive results.
Hassanodin et al. demonstrated that comorbidities should be considered in any rehabilitation. It is clearly affect the participation or progression of program [50]. It seems individualized rehabilitation approach is rational. According to position statement of Taiwan Academy, rehabilitation programs for patients with COVID-19 should adjusted according to clinical statuses. COVID-19 patients were categorized into the following groups: 1—mild severity without any risk factor, 2—mild severity with established risk factor, 3—moderate-to-severe severity, 4—ventilator-assisted cases without cognitive problem, and 5- ventilator- assisted cases with cognitive problem [51].
As there was a huge heterogeneity regarding the components of rehabilitation training, it is not possible to compare the results within the different frequency and duration of programs. Also, a large modes of workouts including breathing exercise, muscle relaxation training, aerobic, strengthening, stretching as well as balance training were used as exercise rehabilitation in included studies.
It is thought that the broad expression of Human Angiotensin-Converting Enzyme-2 (hACE-2) receptors in multiple organs could lead to wide extra-pulmonary manifestations in COVID-19 [52]. Most outcomes have been addressed by included studies were related to cardiopulmonary, and psychological factors. It seems the remaining extra-pulmonary manifestations including neurologic, gastrointestinal, hematologic, hepatic, and renal involvement should be more considered in future studies. Although study by Mohammed et al. demonstrated the benefits of exercise on some hematologic factors [52], the role of exercise in coagulopathy is relatively scarce. Previous research introduced the coagulopathy as the most important feature of hematologic manifestations in COVID-19 [53]. In this regard, Zadow et al. reported that mild-to-moderate exercise training might improve the coagulopathy problems associated with COVID-19. However, probably the opposite effect could be observed in high intensity exercise [54].
Limitation
In current study, there were huge heterogeneity in included studies. In addition to differences in FITT components of exercise, large variation in disease severity, as well as rehabilitation onset was observed. In addition, the measured outcomes were broadly different in each study. In light of these considerations, meta-analysis could not be performed. We have also included all studies determining the effect of exercise as a part of rehabilitation on COVID-19 outcomes. As the other non-exercise component of rehabilitation programs including either nutritional, or psychological consultation have been neglected, the results should be interpreted with some cautions.
Conclusion
Exercise rehabilitation generally could have a beneficial role in improvement of both physical and psychological related outcomes. As the best onset time, and FITT components are not yet completely clear, further large, well-designed RCTs are mandatory to provide details of exercise rehabilitation program.
Abbreviations
- BI:
-
Barthel index
- CPET:
-
Cardio-pulmonary exercise test
- DLCO:
-
Diffusing capacity for carbon monoxide
- FEV1:
-
Force expiratory volume in 1 s
- FITT:
-
Frequency, intensity, time and type
- FVC:
-
Forced volume capacity
- hACE-2:
-
Human angiotensin-converting enzyme-2
- MCID:
-
Minimal clinically important difference
- MEP:
-
Maximum expiratory pressure
- mMRC:
-
Modified Medical Research Council
- MP:
-
Maximum inspiratory pressure
- NICE:
-
The National Institute for Health and Care Excellence
- PEFR:
-
Peak expiratory flow rate
- PEmax:
-
Maximum expiratory pressure
- PImax:
-
Maximum inspiratory pressure
- PRISMA:
-
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ROBVIS:
-
Results of the risk of bias visualization
- SARS:
-
Severe acute respiratory syndrome
- SPPB:
-
Short physical performance battery
- STS:
-
Step test score
- STSS:
-
Sit to stand score
- TLC:
-
Total lung capacity
- TLCO%:
-
Transfer factor for lung carbon monoxide
- 6MWT:
-
Six minutes’ walk test
- 30STS:
-
Thirty-second sit-to-stand test
References
WHO Coronavirus Disease (COVID-19) Dashboard. Available from https://covid19.who.int/. Accessed 29 Feb 2022
Bo W, Xi Y, Tian Z (2021) The role of exercise in rehabilitation of discharged COVID-19 patients. Sports Med Health Sci 3(4):194–201
Barker-Davies RM, O’Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S et al (2020) The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 54(16):949–959
Gloeckl R, Leitl D, Jarosch I, Schneeberger T, Nell C, Stenzel N, et al (2021) Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res https://doi.org/10.1183/23120541.00108-2021
Gaffney AW (2022) The long-COVID conundrum. Am J Med 135:5–6
Kaplan RM, Milstein A (2021) Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc Natl Acad Sci 118(10): e2021726118
Peng X-L, Cheng J-S-Y, Gong H-L, Yuan M-D, Zhao X-H, Li Z, et al (2021) Advances in the design and development of SARS-CoV-2 vaccines. Milit Med Res 8(1):1–31
Li C-X, Noreen S, Zhang L-X, Saeed M, Wu P-F, Ijaz M, et al (2021) A critical analysis of the SARS-CoV-2 (COVID-19) pandemic, emerging variants, therapeutic interventions, and vaccination strategies. Biomed Pharmacother 146:112550
Nieman DC (2021) Exercise is medicine for immune function: implication for COVID-19. Curr Sports Med Rep 20(8):395–401
Li J, Xia W, Zhan C, Liu S, Yin Z, Wang J, et al (2021) A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax. https://doi.org/10.1136/thoraxjnl-2021-217382
Tavakol Z, Ghannadi S, Tabesh MR, Halabchi F, Noormohammadpour P, Akbarpour S, et al (2021) Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study. J Public Health. https://doi.org/10.1007/s10389-020-01468-9
Halabchi F, Mazaheri R, Sabeti K, Yunesian M, Alizadeh Z, Ahmadinejad Z et al (2020) Regular sports participation as a potential predictor of better clinical outcome in adult patients with COVID-19: a large cross-sectional study. J Phys Act Health 18(1):8–12
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88:105906
Higgins J, Altman D, Sterne J (2011) Assessing risk of bias in included studies. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook cochrane org, pp 243–96
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al (2017) Systematic reviews of etiology and risk. Joanna Briggs institute reviewer's manual The Joanna Briggs Institute, p 5
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Research Synthesis Methods. https://doi.org/10.1002/jrsm.1411
Abodonya AM, Abdelbasset WK, Awad EA, Elalfy IE, Salem HA, Elsayed SH (2021) Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: a pilot control clinical study. Medicine 100(13):e25339
Gonzalez-Gerez JJ, Saavedra-Hernandez M, Anarte-Lazo E, Bernal-Utrera C, Perez-Ale M, Rodriguez-Blanco C (2021) Short-term effects of a respiratory telerehabilitation program in confined COVID-19 patients in the acute phase: a pilot study. Int J Environ Res Public Health 18(14):7511
Laurine A, Rolland Y, Gerard S, Kergoat M-J, Peyrusqué E, Aubertin-Leheudre M (2021) Feasibility and effect of implementing physical activity program implementation during COVID-19 in hospitalized positive COVID-19 older adults. J Nutr Health Aging 25(6):724–726
Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y (2020) Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract 39:101166
Liu Y, Yang Y-Q, Liu Y, Pei S-L, Yang H-H, Wu J-J, et al (2021) Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychol Health Med 27:333–342
Mohamed AA, Alawna M (2021) The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: a randomized control trial. J Bodyw Mov Ther 28:425–432
Özlü İ, Öztürk Z, Karaman Özlü Z, Tekin E, Gür A (2021) The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID-19: a randomized controlled study. Perspect Psychiatr Care 57(4):1791–1797
Rodriguez-Blanco C, Gonzalez-Gerez JJ, Bernal-Utrera C, Anarte-Lazo E, Perez-Ale M, Saavedra-Hernandez M (2021) Short-term effects of a conditioning telerehabilitation program in confined patients affected by COVID-19 in the acute phase. A pilot randomized controlled trial. Medicina 57(7):684
Tang Y, Jiang J, Shen P, Li M, You H, Liu C, et al (2021) Liuzijue is a promising exercise option for rehabilitating discharged COVID-19 patients. Medicine. 100(6): e24564
Shah W, Hillman T, Playford ED, Hishmeh L (2021) Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ 372:n136
Al Chikhanie Y, Veale D, Schoeffler M, Pépin J, Verges S, Hérengt F (2021) Effectiveness of pulmonary rehabilitation in COVID-19 respiratory failure patients post-ICU. Respir Physiol Neurobiol 287:103639
Daynes E, Gerlis C, Chaplin E, Gardiner N, Singh SJ (2021) Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition—a cohort study. Chron Respir Dis 18:14799731211015692
Everaerts S, Heyns A, Langer D, Beyens H, Hermans G, Troosters T et al (2021) COVID-19 recovery: benefits of multidisciplinary respiratory rehabilitation. BMJ Open Respir Res 8(1):e000837
Hameed F, Palatulan E, Jaywant A, Said R, Lau C, Sood V et al (2021) Outcomes of a COVID-19 recovery program for patients hospitalized with SARS-CoV-2 infection in New York City: a prospective cohort study. PM&R 13(6):609–617
Jiandani MP, Salagre SB, Kazi S, Iyer S, Patil P, Khot WY, et al (2020) Preliminary observations and experiences of physiotherapy practice in acute care setup of COVID 19: a retrospective observational study. J Assoc Physic India 68:18–24
Li L, Yu P, Yang M, Xie W, Huang L, He C, et al (2021) Physical therapist management of COVID-19 in the intensive care unit: the West China Hospital experience. Phys Therapy 101(1):pzaa198
Maniscalco M, Fuschillo S, Ambrosino P, Martucci M, Papa A, Matera MG et al (2021) Preexisting cardiorespiratory comorbidity does not preclude the success of multidisciplinary rehabilitation in post-COVID-19 patients. Respir Med 184:106470
Martin I, Braem F, Baudet L, Poncin W, Fizaine S, Aboubakar F et al (2021) Follow-up of functional exercise capacity in patients with COVID-19: it is improved by telerehabilitation. Respir Med 183:106438
Olezene CS, Hansen E, Steere HK, Giacino JT, Polich GR, Borg-Stein J et al (2021) Functional outcomes in the inpatient rehabilitation setting following severe COVID-19 infection. PLoS ONE 16(3):e0248824
Rosen K, Patel M, Lawrence C, Mooney B (2020) Delivering telerehabilitation to COVID-19 inpatients: a retrospective chart review suggests it is a viable option. HSS J 16(1_suppl):64–70
Udina C, Ars J, Morandi A, Vilaró J, Cáceres C, Inzitari M (2021) Rehabilitation in adult post-COVID-19 patients in post-acute care with therapeutic exercise. J Frailty Aging 10(3):297–300
Zampogna E, Paneroni M, Belli S, Aliani M, Gandolfo A, Visca D et al (2021) Pulmonary rehabilitation in patients recovering from COVID-19. Respiration 100(5):416–422
Zha L, Xu X, Wang D, Qiao G, Zhuang W, Huang S (2020) Modified rehabilitation exercises for mild cases of COVID-19. Ann Palliat Med 9:3100–3106
Zhang X-B, Zhang J-L, Li M-X, Yuan Y-P, Sun J (2021) Baduanjin exercise can alleviate anxiety and depression of patients with COVID-19 in Square cabin hospital: a cross-sectional survey. Medicine 100(32):e26898
Connolly B, Salisbury L, O'neill B, Geneen L, Douiri A, Grocott MP, et al (2016) Exercise rehabilitation following intensive care unit discharge for recovery from critical illness: executive summary of a Cochrane Collaboration systematic review. J Cachexia Sarcopenia Muscle. 7(5):520–526
Goodwin VA, Allan L, Bethel A, Cowley A, Cross JL, Day J et al (2021) Rehabilitation to enable recovery from COVID-19: a rapid systematic review. Physiotherapy 111:4–22
Barman A, Sinha MK, Sahoo J, Jena D, Patel V (2022) Respiratory rehabilitation in patients recovering from severe acute respiratory syndrome: a systematic review and meta-analysis. Heart Lung 53:11–24
Xi ZJHHH, Zhi Z (2020) Chinese Association of Rehabilitation Medicine, Respiratory rehabilitation committee of Chinese Association of Rehabilitation Medicine, Cardiopulmonary rehabilitation Group of Chinese Society of Physicai Medicine and Rehabilitation. In: Recommendations for respiratory rehabilitation of COVID-19 in adults, vol 432020, p E029
MEDICA EM (2020) Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency
Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, Petraroli A et al (2020) Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res 48(8):0300060520948382
Wittmer VL, Paro FM, Duarte H, Capellini VK, Barbalho-Moulim MC (2021) Early mobilization and physical exercise in patients with COVID-19: a narrative literature review. Complement Ther Clin Pract 43:101364
Rayegani SM, Raeissadat SA, Fakharian A, Babaee M, Nezamabadi M, Boland Nazar NS, et al (2021) Role of rehabilitation medicine in the COVID-19 pandemic: an Iranian consensus. Eur J Phys Rehabil Med 57: 309–310
Vitacca M, Carone M, Clini EM, Paneroni M, Lazzeri M, Lanza A et al (2020) Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration 99(6):493–499
Hasanudin H, Sukartini T, Makhfudli M, Rosyid AN, Revita NCT, Aini HN (2022) The effectiveness of pulmonary rehabilitation on pulmonary function among adults patients of COVID-19 survivors: a systematic review. J Respir 8(1):15–25
Cheng Y-Y, Chen C-M, Huang W-C, Chiang S-L, Hsieh P-C, Lin K-L et al (2021) Rehabilitation programs for patients with COronaVIrus Disease 2019: consensus statements of Taiwan Academy of Cardiovascular and Pulmonary Rehabilitation. J Formos Med Assoc 120(1):83–92
Thakur V, Ratho RK, Kumar P, Bhatia SK, Bora I, Mohi GK et al (2021) Multi-organ involvement in COVID-19: beyond pulmonary manifestations. J Clin Med 10(3):446
Higgins V, Sohaei D, Diamandis EP, Prassas I (2021) COVID-19: from an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci 58(5):297–310
Zadow EK, Wundersitz DWT, Hughes DL, Adams MJ, Kingsley MIC, Blacklock HA, et al., editors. Coronavirus (COVID-19), coagulation, and exercise: interactions that may influence health outcomes. Seminars in thrombosis and hemostasis; 2020: Thieme Medical Publishers
Author information
Authors and Affiliations
Contributions
FH devised the project, the main conceptual ideas and proof outline. He also revised the drafted manuscript critically for important intellectual content. BM, MS, and BT contributed to study implementation. They drafted the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This study is a review type and ethical approval is not required.
Informed consent
For this type of review study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Halabchi, F., Selk-Ghaffari, M., Tazesh, B. et al. The effect of exercise rehabilitation on COVID-19 outcomes: a systematic review of observational and intervention studies. Sport Sci Health 18, 1201–1219 (2022). https://doi.org/10.1007/s11332-022-00966-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-022-00966-5