Abstract
Purpose
The association between insomnia disorder and cancer-related mortality risk remains controversial. Therefore, this study aimed to investigate the correlation between insomnia disorder and cancer-related mortality.
Methods
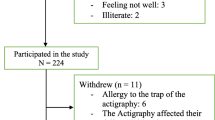
Patients who were diagnosed with musculoskeletal disease (MSD) between 2010 and 2015 were included in this study as a secondary analysis of a patient cohort with MSD in South Korea. Cancer mortality was evaluated between January 1, 2016, and December 31, 2020, using multivariable Cox regression modeling. Patients with and without insomnia disorder constituted the ID and non-ID groups, respectively.
Results
The final analysis incorporated a total of 1,298,314 patients diagnosed with MSDs, of whom 11,714 (0.9%) died due to cancer. In the multivariable Cox regression model, the risk of total cancer-related mortality was 14% (hazard ratio [HR], 1.14; 95% confidence interval [CI], 1.10–1.19; P < 0.001) higher in the ID group than in the non-ID group. Moreover, the ID group had a higher risk of mortality due to esophageal (HR, 1.46; 95% CI, 1.08–1.96; P = 0.015), colorectal (HR, 1.20; 95% CI, 1.05–1.36; P = 0.007), head and neck (HR, 1.39; 95% CI, 1.01–1.94; P = 0.049), lung (HR, 1.17; 95% CI, 1.08–1.27; P < 0.001), and female genital organ (HR: 1.39, 95% CI: 1.09, 1.77; P = 0.008) cancers; leukemia; and lymphoma (HR, 1.30; 95% CI, 1.12–1.49; P < 0.001).
Conclusion
Insomnia disorder was associated with elevated overall cancer mortality in patients with MSDs, which was more evident for cancer mortality due to esophageal, colorectal, head and neck, lung, and female genital organ cancers; leukemia; and lymphoma.

Similar content being viewed by others
Data availability
Data will be available upon reasonable request to the corresponding author.
References
Global Burden of Disease Cancer C, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA et al (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol 3(4):524–48. https://doi.org/10.1001/jamaoncol.2016.5688
Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD et al (2022) Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the global burden of disease study 2019. JAMA Oncol 8(3):420–444
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA: Cancer J Clin 72(1):7–33
Dalmartello M, La Vecchia C, Bertuccio P, Boffetta P, Levi F, Negri E et al (2022) European cancer mortality predictions for the year 2022 with focus on ovarian cancer. Ann Oncol 33(3):330–339
Winkelman JW (2015) Insomnia disorder. N Engl J Med 373(15):1437–1444
Fang H-F, Miao N-F, Chen C-D, Sithole T, Chung M-H (2015) Risk of cancer in patients with insomnia, parasomnia, and obstructive sleep apnea: a nationwide nested case-control study. J Cancer 6(11):1140–1147
Shi T, Min M, Sun C, Zhang Y, Liang M, Sun Y (2020) Does insomnia predict a high risk of cancer? A systematic review and meta-analysis of cohort studies. J Sleep Res 29(1):e12876
Ge L, Guyatt G, Tian J, Pan B, Chang Y, Chen Y et al (2019) Insomnia and risk of mortality from all-cause, cardiovascular disease, and cancer: systematic review and meta-analysis of prospective cohort studies. Sleep Med Rev 48:101215. https://doi.org/10.1016/j.smrv.2019.101215
Song IA, Choi HR, Oh TK (2022) Long-term opioid use and mortality in patients with chronic non-cancer pain: ten-year follow-up study in South Korea from 2010 through 2019. EClinicalMedicine 51:101558. https://doi.org/10.1016/j.eclinm.2022.101558
Tang NK, McBeth J, Jordan KP, Blagojevic-Bucknall M, Croft P, Wilkie R (2015) Impact of musculoskeletal pain on insomnia onset: a prospective cohort study. Rheumatology 54(2):248–256
Uhlig BL, Sand T, Nilsen T, Mork PJ, Hagen K (2018) Insomnia and risk of chronic musculoskeletal complaints: longitudinal data from the HUNT study, Norway. BMC Musculoskelet Disord 19:1–9
Moradi-Lakeh M, Forouzanfar MH, Vollset SE, El Bcheraoui C, Daoud F, Afshin A et al (2017) Burden of musculoskeletal disorders in the Eastern Mediterranean Region, 1990–2013: findings from the Global Burden of Disease Study 2013. Ann Rheum Dis 76(8):1365–1373. https://doi.org/10.1136/annrheumdis-2016-210146
Savard J, Laroche L, Simard S, Ivers H, Morin CM (2003) Chronic insomnia and immune functioning. Psychosom Med 65(2):211–221. https://doi.org/10.1097/01.psy.0000033126.22740.f3
Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E (2021) Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol 4(1):1304. https://doi.org/10.1038/s42003-021-02825-4
Wu AH, Wang R, Koh W-P, Stanczyk FZ, Lee H-P, Yu MC (2008) Sleep duration, melatonin and breast cancer among Chinese women in Singapore. Carcinogenesis 29(6):1244–1248
Ta WEHR (1991) The durations of human melatonin secretion and sleep respond to changes in daylength (photoperiod). J Clin Endocrinol Metab 73(6):1276–1280
Luo J, Zhang Z, Sun H, Song J, Chen X, Huang J et al (2020) Effect of melatonin on T/B cell activation and immune regulation in pinealectomy mice. Life Sci 242:117191
Kakizaki M, Inoue K, Kuriyama S, Sone T, Matsuda-Ohmori K, Nakaya N et al (2008) Sleep duration and the risk of prostate cancer: the Ohsaki cohort study. Br J Cancer 99(1):176–178
Jiao L, Duan Z, Sangi-Haghpeykar H, Hale L, White D, El-Serag H (2013) Sleep duration and incidence of colorectal cancer in postmenopausal women. Br J Cancer 108(1):213–221
Cao J, Eshak ES, Liu K, Muraki I, Cui R, Iso H et al (2019) Sleep duration and risk of breast cancer: the JACC study. Breast Cancer Res Treat 174:219–225
Peng TR, Yang LJ, Wu TW, Chao YC (2020) Hypnotics and risk of cancer: a meta-analysis of observational studies. Medicina (Kaunas) 56(10). https://doi.org/10.3390/medicina56100513
Massoco C, Palermo-Neto J (2003) Effects of midazolam on equine innate immune response: a flow cytometric study. Vet Immunol Immunopathol 95(1–2):11–19
Torres SR, Fröde TS, Nardi GM, Vita N, Reeb R, Ferrara P et al (2000) Anti-inflammatory effects of peripheral benzodiazepine receptor ligands in two mouse models of inflammation. Eur J Pharmacol 408(2):199–211
Yoon K, Shin CM, Han K, Jung JH, Jin EH, Lim JH et al (2023) Risk of cancer in patients with insomnia: nationwide retrospective cohort study (2009–2018). PLoS ONE 18(4):e0284494
Blaess J, Walther J, Petitdemange A, Gottenberg JE, Sibilia J, Arnaud L et al (2020) Immunosuppressive agents for rheumatoid arthritis: a systematic review of clinical trials and their current development stage. Ther Adv Musculoskelet Dis 12:1759720X20959971. https://doi.org/10.1177/1759720X20959971
Hsu CY, Lin MS, Su YJ, Cheng TT, Lin YS, Chen YC et al (2017) Cumulative immunosuppressant exposure is associated with diversified cancer risk among 14 832 patients with systemic lupus erythematosus: a nested case-control study. Rheumatology (Oxford) 56(4):620–628. https://doi.org/10.1093/rheumatology/kew457
Cronstein BN, Sunkureddi P (2013) Mechanistic aspects of inflammation and clinical management of inflammation in acute gouty arthritis. J Clin Rheumatol 19(1):19
Araki Y, Mimura T (2016) The mechanisms underlying chronic inflammation in rheumatoid arthritis from the perspective of the epigenetic landscape. J Immunol Res 2016:6290682. https://doi.org/10.1155/2016/6290682
Nigam M, Mishra AP, Deb VK, Dimri DB, Tiwari V, Bungau SG et al (2023) Evaluation of the association of chronic inflammation and cancer: Insights and implications. Biomed Pharmacother 164:115015. https://doi.org/10.1016/j.biopha.2023.115015
McBeth J, Symmons D, Silman A, Allison T, Webb R, Brammah T et al (2009) Musculoskeletal pain is associated with a long-term increased risk of cancer and cardiovascular-related mortality. Rheumatology 48(1):74–77
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
In-Ae Song and Tak Kyu Oh helped with the study's design, conducted data analysis, and wrote the initial manuscript. Hye Yoon Park reviewed the manuscript closely and assisted with data collection. The manuscript was read and approved in its final form by all authors.
Corresponding author
Ethics declarations
Ethical approval
All procedures involving human participants in this study were conducted in adherence to the ethical guidelines set forth by the relevant national and institutional research committees (IRB: X-2105–685-901, Seoul National University Bundang Hospital). Additionally, the 1964 Declaration of Helsinki and any subsequent amendments or comparable ethical standards were utilized.
Consent to participate
For this type of study, formal consent was not required.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oh, T.K., Park, H.Y. & Song, IA. Insomnia disorder and cancer mortality in South Korea: a secondary analysis of musculoskeletal disease cohort. Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03009-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03009-0