Abstract
Purpose
To evaluate the association of recently diagnosed obstructive sleep apnea (OSA) with TNF-α and IL-6 and to measure the effect of short-term continuous positive airway pressure (CPAP) therapy on these markers.
Methods
A prospective, open-label, controlled trial was conducted among patients referred for diagnostic polysomnography (PSG). After PSG, patients were divided into 3 groups: OSA intervention group (N = 21), OSA control untreated group (N = 19), and non-OSA control group (N = 24). IL-6 and TNF-α levels were measured at baseline and 1 month after intervention. Repeated measures (RM) ANOVA and ANCOVA were used to compare the three groups regarding changes in TNF-α and IL-6 levels by analyzing between-subject and within-subject effects as a function of time and adjusting for significant covariates.
Results
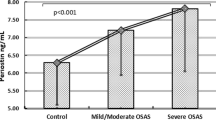
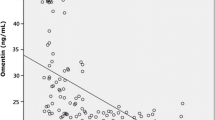
At baseline, IL-6 (p = 0.05) and TNF-α (p = 0.04) were significantly higher in the OSA patients than in the non-OSA controls. There was no effect of time either on the TNF-α (p = 0.069) or IL-6 (p = 0.717) after 1 month of CPAP. No interaction effect between group and time was found for either TNF-α (p = 0.240) or IL-6 (p = 0.552) after 1 month of CPAP. There was neither a group effect nor an interaction effect between group and time for either IL-6 or TNF α after adjusting for age, BMI, neck circumference, and AHI.
Conclusion
This study showed increases in proinflammatory state as illustrated by plasma TNF-α and IL-6 levels among recently diagnosed OSA patients, but there were no changes in these inflammatory markers following 1-month CPAP therapy.




Similar content being viewed by others
Change history
28 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11325-022-02605-2
References
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, Peppard PE (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698
Wali SO, Abalkhail B, Krayem A (2017) Prevalence and risk factors of obstructive sleep apnea syndrome in a Saudi Arabian population. Annals of thoracic medicine 12(2):88–94
Lee W, Nagubadi S, Kryger MH, Mokhlesi B (2008) Epidemiology of obstructive sleep apnea: a population-based perspective. Expert review of respiratory medicine 2(3):349–364
Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM (2009) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin sleep cohort study. WMJ: official publication of the State Medical Society of Wisconsin 108(5):246–249
Kato M, Roberts-Thomson P, Phillips BG, Haynes WG, Winnicki M, Accurso V, Somers VK (2000) Impairment of endothelium-dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation 102(21):2607–2610
McNicholas W, Bonsignore T, The Management Committee of EU COST ACTION B26 (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanism and research priorities. Eur Respir J 29:156–178
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, Hirano T, Adachi M (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107(8):1129–1134
Maeder MT, Strobel W, Christ M, Todd J, Estis J, Wildi K et al (2015) Comprehensive biomarker profiling in patients with obstructive sleep apnea. Clin Biochem 48(4–5):340–346
Ciftci TU, Kokturk O, Bukan N, Bilgihan A (2004) The relationship between serum cytokine levels with obesity and obstructive sleep apnea syndrome. Cytokine 28(2):87–91
Kheirandish-Gozal L, Gozal D (2019) Obstructive sleep apnea and inflammation: proof of concept based on two illustrative cytokines. Int J Mol Sci 20(3):459
Steiropoulos P, Papanas N, Nena E, Antoniadou M, Serasli E, Papoti S & Tsara V (2010) Inflammatory markers in middle-aged obese subjects: does obstructive sleep apnea syndrome play a role? Mediators of inflammation, 2010
Steiropoulos P, Kotsianidis I, Nena E, Tsara V, Gounari E, Hatzizisi O, Kyriazis G, Christaki P, Froudarakis M, Bouros D (2009) Long-term effect of continuous positive airway pressure therapy on inflammation markers of patients with obstructive sleep apnea syndrome. Sleep 32(4):537–543
Kohler M, Ayers L, Pepperell JC, Packwood KL, Ferry B, Crosthwaite N et al (2009) Effects of continuous positive airway pressure on systemic inflammation in patients with moderate to severe obstructive sleep apnoea: a randomised controlled trial. Thorax 64(1):67–73
Stradling JR, Craig SE, Kohler M, Nicoll D, Ayers L, Nunn AJ, Bratton DJ (2015) Markers of inflammation: data from the MOSAIC randomised trial of CPAP for minimally symptomatic OSA. Thorax 70(2):181–182
Ünüvar Doğan F, Yosunkaya Ş, Kuzu Okur H, Can Ü (2014) Relationships between obstructive sleep apnea syndrome, continuous positive airway pressure treatment, and inflammatory cytokines. Sleep disorders 2014:1–6
Johns MW (1991) Sleep disorders unit. a new method for measuring daytime sleepiness: the epworth sleepiness scale. Sleep 14(6):540–545
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV (2017) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications: version 2.3. American Academy of sleep medicine, Darien, IL
American Academy of Sleep Medicine (2014) International classification of sleep disorders. American Academy of sleep medicine, Darien
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA, Positive Airway Pressure Titration Task Force of the American Academy of Sleep Medicine (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 04:157–171
Schwab RJ, Badr SM, Epstein LJ, Gay PC, Gozal D, Kohler M et al (2013) An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med 188(5):613–620
Nadeem R, Molnar J, Madbouly EM, Nida M, Aggarwal S, Sajid H, Naseem J, Loomba R (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 09:1003–1012
Wang J, Yu W, Gao M, Zhang F, Gu C, Yu Y, Wei Y (2015) Impact of obstructive sleep apnea syndrome on endothelial function, arterial stiffening, and serum inflammatory markers: an updated meta-analysis and metaregression of 18 studies. J Am Heart Assoc 4(11):e002454
Unnikrishnan D, Jun J, Polotsky V (2015) Inflammation in sleep apnea: an update. Reviews in Endocrine and Metabolic Disorders 16(1):25–34
Ryan S, Nolan GM, Hannigan E, Cunningham S, Taylor C, McNicholas WT (2007) Cardiovascular risk markers in obstructive sleep apnoea syndrome and correlation with obesity. Thorax 62(6):509–514
Trayhurn P, Wang B, Wood IS (2008) Hypoxia in adipose tissue: a basis for the dysregulation of tissue function in obesity? Br J Nutr 100(2):227–235
Ryan S (2017) Adipose tissue inflammation by intermittent hypoxia: mechanistic link between obstructive sleep apnoea and metabolic dysfunction. J Physiol 595(8):2423–2430
Baessler A, Nadeem R, Harvey M, Madbouly E, Younus A, Sajid H, Naseem J, Asif A, Bawaadam H (2013) Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers-a meta-analysis. J Inflamm 10(1):13
Xie X, Pan L, Ren D, Du C, Guo Y (2013) Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med 14(11):1139–1150
Jullian-Desayes I, Joyeux-Faure M, Tamisier R, Launois S, Borel AL, Levy P, Pepin JL (2015) Impact of obstructive sleep apnea treatment by continuous positive airway pressure on cardiometabolic biomarkers: a systematic review from sham CPAP randomized controlled trials. Sleep Med Rev 21:23–38
Acknowledgments
We are grateful to Dr. Afnan Hafiz and Dr. Ibrahim Zakaria for their help in the data collection process. Authors would also like to thank Mr. Badrudin Banjar and Mrs. Ofelia El-Assal from the Immunology Lab, King Abdulaziz University Hospital for their help in collecting and analyzing blood samples. Finally, we would like to acknowledge the great efforts done by Mrs. Walaa Abuzahra, Research Coordinator, Sleep Medicine and Research Center, in coordinating all study procedures.
Funding
This project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah, Saudi Arabia under grant no. (KEP-2-140-39). The authors, therefore, acknowledge and appreciate DSR technical and financial support.
Author information
Authors and Affiliations
Contributions
SW, JM, FH, DG involved in planning for the study including the research question, methodology and data collection. FS, HM collected data and were involved in planning and supervised the work. DM processed the experimental data, performed the statistical analysis, drafted the manuscript and designed the figs. JM performed the measurements and processed the collected data. SW, JM, DM, DG aided in interpreting the results and worked on the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest/competing interests
None.
Availability of data and material
All research data available at the Sleep Medicine and Research Center, King Abdulaziz University Hospital, Jeddah, Saudi Arabia and will be retained for a period of 5 years.
Ethics approval
Reference number 178–18
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wali, S.O., Al-Mughales, J., Alhejaili, F. et al. The utility of proinflammatory markers in patients with obstructive sleep apnea. Sleep Breath 25, 545–553 (2021). https://doi.org/10.1007/s11325-020-02149-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02149-3