Abstract
This paper offers the perspective of a behavioural scientist advising and providing evidence for Ireland's government during the coronavirus pandemic. It describes how behavioural research informed the public response in the early months of the crisis, but lost influence as political conflict increased. It proposes some broader lessons for managing public health crises, one of which is to recognise the potential wisdom of crowds.
Similar content being viewed by others
1 Introduction
On 29 February 2020, the first case of COVID-19 in Ireland was confirmed. Any hopes that this deadly virus would not reach our “island behind an island” died. Battle commenced. This article offers some reflections on what has followed from the perspective of a behavioural scientist with a government advisory role. It describes how Ireland has fared and highlights factors that perhaps contributed. It then offers some lessons that might be learned and which may generalise beyond this island. The contribution is unashamedly parochial and mixes claims for which there is clear evidence with personal observations for which there is not.
2 The Irish case
Scholarly debate about the determinants of national variation in health outcomes will doubtless rage for decades. Nevertheless, by objective measures, such as cases and deaths per capita, Ireland coped better in the first six months of the pandemic than its near western European neighbours. I believe that behavioural science played some part in Ireland’s relative success. However, in common with many European nations, Ireland has experienced a second wave of infection, the severity of which surprised its expert community and political class. Behavioural science may have something to say about this too.
I head the Behavioural Research Unit at Ireland’s Economic and Social Research Institute (ESRI). At the outset, the ESRI team rapidly compiled and published a review of relevant behavioural evidence (Lunn et al. 2020a). While the review ranged from nudges to promote handwashing to principles of crisis communication, the primary argument was the need to understand the public response as a cooperative solution to a collective action problem (Ostrom et al. 1992; Ledyard 1995). We circulated a preprint within government on 11 March, which advocated clear and repeated government communication of a strategy that was “best for all”, coupled with efforts to build and exploit common identity for the fight ahead. Researchers who generate evidence for policy rarely know how much their findings influence policy, but judging by the content and language of successive government decisions as the virus spread, the review apparently had some impact. As Ireland imposed strong social distancing restrictions faster than its neighbours, the initial public response was overwhelmingly positive and cohesive.
Ireland established a National Public Health Emergency Team (NPHET) and formed multiple subgroups to supply evidence and advice to NPHET, including a Behavioural Change Subgroup, which I was asked to join. Small countries probably enjoy an advantage when trying to pull together expertise in an emergency. Ireland has only a handful of teams that do applied behavioural science. They know each other well and have worked previously with relevant government officials.
The Subgroup met online weekly to consider evidence from domestic tracking surveys and emerging international behavioural literature, and to commission and oversee rapidly conducted behavioural research studies. Between late March and the end of July, the group generated evidence for NPHET on interventions to improve hand hygiene (Murphy 2020), wellbeing impacts (Lades et al. 2020), messages to promote social distancing (Lunn et al. 2020b), public expectations (Belton et al. 2020), the use of decision aids to support symptom recognition and self-isolation (Lunn et al. 2021), accuracy of compliance measurement (Timmons et al. 2020a), comprehension of the test and trace system (Timmons et al. 2020b), and the perceived risk of different social scenarios (Timmons et al. 2020c). It also conducted a survey of business readiness for re-opening and a behavioural pre-test of Ireland’s contact tracing app (Julienne et al. 2020).
The majority of these studies were rapid online experiments undertaken to answer research questions asked by NPHET, with preliminary results delivered in three to four weeks to inform evidence and communications. The group received weekly feedback on how the research was contributing to government advice. Findings were released publicly and received widespread media coverage. In this way, behavioural science in Ireland contributed directly and transparently to the national effort, measuring public understanding, diagnosing problems and pretesting interventions.
By mid-May, the first curve was flattened. With falling case numbers, Ireland’s government began a phased lifting of public health restrictions. As economic and social activity returned, infections continued to fall faster than expected. Evidence from other European nations suggested the same. Political and commercial lobbying intensified and the lifting of restrictions was accelerated. The case numbers stayed low until late July. Weekly expert meetings became fortnightly and exhausted public officials and researchers began to take holidays.
With hindsight, it seems likely that during this period, the first small ripples that would form Ireland’s second wave began. While epidemiologists argued that it would take at least two to three weeks for changes to restrictions to have an impact on transmission, the reality is that it probably took much longer. The behavioural tracking data collected by Ireland’s Department of HealthFootnote 1 did not display step-jumps when social distancing restrictions were lifted. Instead, people remained cautious and behaviour changed only gradually over many weeks. For instance, in the two months from mid-May to mid-July, the proportion of people reporting that they had returned to leaving their home “as much as usual” rose from 16 to 35%, but the week-on-week trend was almost linear. The response to lifting restrictions had a long “behavioural lag”. Failure to account for this behavioural lag led the authorities to underestimate of the impact of lifting restrictions on disease transmission.
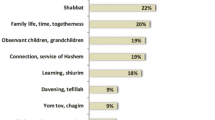
At the same time, the tracking data recorded something curious: despite falling case numbers, the Irish public was, on average, becoming more worried about the virus not less. The proportion of the public who expected a second wave climbed from 54 to 78% in the six weeks from mid-June. Moreover, they were not just predicting containable local outbreaks. The proportion believing that “the worst of the pandemic is behind us” fell from 62 to 29% during the same period. This large fluctuation in sentiment occurred before any increase in case numbers was reported. The implication is that this Irish data displayed a “wisdom of crowds” effect (Galton 1907). The public had been bombarded with information about how to prevent coronavirus transmission. Observing the extent and type of social interactions around them, people’s opinion of what was to come, when aggregated, proved more prescient than the views of Ireland’s expert community, which found itself surprised by the rapidity and scale of the second wave.
In late July, the Behavioural Change Subgroup met for the last time. Having successfully deployed the tools of behavioural science to help flatten the curve initially, public policy then made insufficient use of it. It is not straightforward to discern why. There was a change of government and in some key personnel. The political consensus broke down. Positions were taken on either side of debates about how to balance the health of the people against that of the economy. As businesses reopened, different sectors sought, and obtained, different regulatory treatment. Broad, simple public health messages morphed into complex rules that varied from context to context. Rising infections were blamed on the failure of a minority to follow these rules. Noncompliance became the focus of a public debate that failed also to address the appropriate scale of compliant social interaction. The demand for behavioural evidence fell away.
As we entered the Autumn, behavioural myths took hold. Public discussion unquestioningly decided that complacency and pandemic fatigue had set in. The latter was a global concern, defined by the World Health Organization (2020) as “demotivation to follow recommended protective behaviours, emerging gradually over time and affected by a number of emotions, experiences and perceptions.” (p.7). Yet, in Ireland at least, data suggested that neither complacency nor fatigue were primary drivers of behaviour. Instead of gradual demotivation, Ireland’s tracking data suggested that between July and October both support for restrictions and compliance with them increased steadily and appreciably. While the psychological determinants of these trends cannot be ascertained for sure, complacency and fatigue are clearly not in the running. The figures were matched by rising worry and anxiety, suggesting that individuals were rebalancing their personal trade-offs between risk and social activity as infection began to rise again.
3 Some lessons
In my view, Ireland’s experience contains lessons for managing public health emergencies. Firstly, as in other countries, the willingness of the population to make voluntary sacrifices for the common good was extraordinary to observe. On a personal level, while knowing that previous evidence suggested widespread public cooperation was likely (e.g., Mawson 2005), I nevertheless watched with awe. Secondly, when a diverse group of behavioural scientists get together regularly to discuss a policy problem, commission research and interpret findings, useful evidence can be generated very rapidly. In our case, while online data collection made this possible, debate and oversight of experimental designs and results by scientific peers greatly increased evidence quality. Such oversight could similarly improve evidence for policy during normal times. Thirdly, in a novel and dynamic situation, if public authorities want to coordinate a behavioural response, they have to keep monitoring and researching behaviour. This was done successfully in the early part of the crisis in Ireland, but when behavioural evidence gathering fell away, decision-making and coordination suffered. Lastly, when uncertain policy outcomes depend on multiple, dispersed behaviours and factors, aggregate public judgement deserves respect. In Ireland, we ignored the concerns of our crowd-a crowd that turned out to be wise.
At the time of writing, there remains great uncertainty about how long this pandemic will last and the toll that, ultimately, it will take. That toll might be reduced if we share our experiences and learn lessons as we go.
Notes
https://www.gov.ie/en/collection/6b4401-view-the-amarach-public-opinion-survey/, accessed 15 October 2020.
References
Belton C, Julienne H, Timmons S, Barjaková M, Lavin C, McGowan F, Lunn PD (2020) Public expectations for lifting Covid-19 restrictions. ESRI Survey and Statistical Report Series, No 88
Galton F (1907) Vox Populi. Nature 75:7
Julienne H, Lavin C, Belton C, Barjaková M, Timmons S, Lunn P (2020) Behavioural pre-testing of COVID Tracker, Ireland’s contact tracing app. ESRI Working Paper, No 687
Lades LK, Laffan K, Daly M, Delaney L (2020) Daily emotional well‐being during the COVID‐19 pandemic. British J Health Psychol 25(4):902–911
Ledyard O (1995) Public goods: some experimental results. In: Kagel J, Roth A (eds) (Chap 2) Handbook of experimental economics. Princeton University Press, Princeton
Lunn PD, Belton CA, Lavin C, McGowan FP, Timmons S, Robertson DA (2020a) Using behavioral science to help fight the coronavirus. J Behav Public Adm 3(1):1–15
Lunn PD, Timmons S, Barjaková M, Belton CA, Julienne H, Lavin C (2020b) Motivating social distancing during the COVID-19 pandemic. Social Sci Med 265:113478
Lunn PD, Timmons S, Julienne H, Belton CA, Barjaková M, Lavin C, McGowan FP (2021) Using decision aids to support self-isolation during the COVID-19 pandemic. Psychol Health 36(2):195–213
Mawson AR (2005) Understanding mass panic and other collective responses to threat and disaster. Psychiatry Interpers Biol Process 68(2):95–113
Murphy R (2020) Using Behavioural Science to Improve Hand Hygiene in Workplaces and Public Places. Research Services and Policy Unit, Department of Health, Ireland
Ostrom E, Walker J, Gardner R (1992) Covenants with and without a sword: self-governance is possible. Am Political Sci Rev 86(2):404–417
Timmons S, McGinnity F, Belton CA, Barjaková M, Lunn PD (2020a) The effects of framing and social desirability on estimates of compliance with COVID-19 health behaviours. J Epidemiol Commun Health, published online, 16 Oct 2020
Timmons S, Barjaková M, Robertson DA, Belton CA, Lunn PD (2020b) Public Understanding and Perceptions of the COVID-19 Test-and-Trace System. ESRI Survey Statistical Report Series, No 96
Timmons S, Belton C, Robertson DA, Barjaková M, Lavin C, Julienne H, Lunn PD (2020c) Is it riskier to meet 100 people outdoors or 14 people indoors? Comparing public and expert perceptions of COVID-19 risk. ESRI Working Paper, No 689
World Health Organization 2020 Pandemic fatigue: reinvigorating the public to prevent COVID-19 WHO Regional Office for Europe Policy framework for supporting pandemic prevention and management Copenhagen 2020
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lunn, P.D. Coronavirus in Ireland: one behavioural scientist’s view. Mind Soc 20, 229–233 (2021). https://doi.org/10.1007/s11299-021-00275-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11299-021-00275-3