Abstract
Objectives
This study investigated whether erosion and osteophyte correlates with condyle bone marrow abnormalities (BMA), as detected with quantitative T2 mapping.
Methods
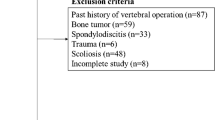
Fifty-six joints (in 44 patients) that demonstrated evidence of bony erosion (ER) or osteophytes (OS) related to disc displacement without reduction were studied with MR images. A control group of 50 joints (in 50 patients) was included. The subjects were divided into five groups; noAR (control), noBMA-ER, BMA-ER, noBMA-OS, and BMA-OS. T2 mapping was performed and the regions of interest were placed over the bone marrow at the top of the condyle. The mean T2 values of the bone marrow of the mandibular condyle were calculated for all mapping images. After assessing age-related changes in T2 values of noAR group using Pearson’s product-moment, differences in median T2 values of five groups were analyzed using Kruskal–Wallis test, and Steel–Dwass test (p < 0.05).
Results
There was no significant correlation between age and T2 value in noAR group. The median T2 values of noBMA-ER and BMA-ER groups were significantly higher than those of noAR, noBMA-OS and BMA-OS groups. Those of noBMA-OS and BMA-OS groups were significantly lower than those of noAR, noBMA-ER and BMA-ER groups. There was no significant difference between noBMA and BMA groups.
Conclusions
It is suggested that erosion and osteophyte of the condyle may correlate with bone marrow abnormalities. T2 mapping could be show slight marrow changes of the arthritic condyle.







Similar content being viewed by others
References
Larheim TA, Westesson PL, Hichs DG, et al. Osteonecrosis of the temporomandibular joint: correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg. 1999;57:888–98. https://doi.org/10.1016/S0278-2391(99)90001-0.
Sano T, Westesson PL, Larheim TA, et al. Osteoarthritis and abnormal bone marrow of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:243–52.
Emshoff R, Brandlmaier I, Schmid C, et al. Bone marrow edema of the mandibular condyle related to internal derangement, osteoarthrosis, and joint effusion. J Oral Maxillofac Surg. 2003;61:35–40. https://doi.org/10.1053/joms.2003.50006.
Higuchi K, Chiba M, Kondo T, Echigo S. The relationship between bone marrow edema and bone changes in the mandibular condyle: a longitudinal study with MR imaging. Oral Sci Int. 2013;10:33–9. https://doi.org/10.1016/S1348-8643(12)00053-5.
Toyoda N, Asada K, Arai T, et al. Follow-up study on morphologic bone changes of the condyle by MRI in TMD type IV in association with clinical findings. J Jpn Soc TMJ. 2000;12:68–76.
Hashizume A, Kobayashi K, Nakagawa Y, et al. A longitudinal study of bony changes on the mandibular condyle using tomography. Tsurumi Univ Dent J. 2003;29:281–7.
Koyama J, Nishiyama H, Hayashi T. Follow-up study of condylar bony changes using helical computed tomography in patients with temporomandibular disorder. Dentomaxillofac Radiol. 2007;36:472–7. https://doi.org/10.1259/dmfr/28078357.
Isberg A. Osteoarthrosis/osteoarthritis. Temporomandibular joint dysfunction: a practitioner’s guide. London: ISIS Medical Media; 2001. p. 103–8.
Otonari-Yamamoto M, Sano T, Okano T, et al. Association between osseous changes of the condyle and temporomandibular joint (TMJ) fluid in osteoarthritis. Oral Radiol. 2015;31:41–8. https://doi.org/10.1007/s11282-014-0185-1.
Mosher TJ, Dardzinski BJ, Smith MB. Human articular cartilage: influence of aging and early symptomatic degeneration on the spatial variation of T2—preliminary findings at 3 T. Radiology. 2000;214:259–66.
Dunn TC, Lu Y, Jin H, et al. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232:592–8. https://doi.org/10.1148/radiol.2322030976.
Stahl R, Blumenkrantz G, Carballido-Gamio J, et al. MRI-derived T2 relaxation times and cartilage morphometry of the tibio-femoral joint in subjects with and without osteoarthritis during a 1-year follow-up. Osteoarthr Cartil. 2007;15:1225–34. https://doi.org/10.1016/j.joca.2007.04.018.
Koff MF, Amrami KK, Kaufman KR. Clinical evaluation of T2 values of patellar cartilage in patients with osteoarthritis. Osteoarthr Cartil. 2007;15:198–204. https://doi.org/10.1016/j.joca.2006.07.007.
Schmid-Schwap M, Bristela M, Pittschieler E, et al. Biochemical analysis of the articular disc of the temporomandibular joint with magnetic resonance T2 mapping: a feasibility study. Clin Oral Invest. 2013;5:1–7. https://doi.org/10.1007/s00784-013-1154-5.
Nikkuni Y, Nishiyama H, Hayashi T. Clinical significance of T2 mapping MRI for the evaluation of masseter muscle pain in patients with temporomandibular joint disorders. Oral Radiol. 2013;29:50–5. https://doi.org/10.1007/s11282-012-0108-y.
Yoda T, Sato T, Abe T, et al. Long-term result of surgical therapy for masticatory muscle tendon-aponeurosis hyperplasia accompanied by limited mouth opening. J Oral Maxillofac Surg. 2009;38:1143–7. https://doi.org/10.1016/j.ijom.2009.07.002.
Iizuka T. The clinical guidelines for temporomandibular joint disorders. J Jpn Soc TMJ. 2003;15:4–20.
Yatani H. Global trends and future perspectives of TMD management: Impact of the innovation of classification and diagnostic criteria. New classification (2013) and its diagnostic criteria of temporomandibular disorders revised by the Japanese Society for Temporomandibular Joint. J Jpn Soc TMJ. 2015;27:76–86 (in Japanese).
Ahmad M, Hollender L, Anderson Q, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–60. https://doi.org/10.1016/j.tripleo.2009.02.023.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015. http://www.R-project.org/.
Moffett BC, Johnson LC, McCabe JB, et al. Articular remodeling in the adult human temporomandibular joint. Am J Anat. 1964;115:119–42.
Oberg T, Carlsson GE, Fajars CM. The temporomandibular joint. A morphologic study on a human autopsy material. Acta Odont Scand. 1971;29:349–84. https://doi.org/10.3109/00016357109026526.
Takenoshita Y. Development with age of the human mandibular condyle: histological study. Cranio. 1987;5:317–23.
Westesson P-L, Rohlin M. Internal derangement related to osteoarthritis in temporomandibular joint autopsy specimens. Oral Surg Oral Med Oral Pathol. 1984;57:17–22. https://doi.org/10.1016/0030-4220(84)90251-2.
Westesson P-L. Structural hard-tissue changes in temporomandibular joints with internal derangement. Oral Surg Oral Med Oral Pathol. 1985;59:220–4. https://doi.org/10.1016/0030-4220(85)90022-2.
Anderson QN, Katzberg RW. Pathologic evaluation of disc dysfunction and osseous abnormalities of the temporomandibular joint. J Oral Maxillofac Surg. 1985;43:947–51. https://doi.org/10.1016/0278-2391(85)90008-4.
Sakamoto I, Yoda T, Sakurai J, et al. Clinical study on morphological bone changes of the condyle in temporomandibular disorders. 2: relation to clinical findings. J Jpn Soc TMJ. 1996;8:216–24.
Alexiou K, Stamatakis H, Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofac Radiol. 2009;38:141–7. https://doi.org/10.1259/dmfr/59263880.
Nah KS. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012;42:249–53. https://doi.org/10.5624/isd.2012.42.4.249.
Nishiyama H, Sasai T, Benedek P, Maeda T, Matsumura S, Fuchihata H. Angle dependence of signal intensity of a bovone tendon at spin echo sequence. Dental Radiol. 1999;39:27–34.
Acknowledgements
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant number 15K20390.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kenichiro Shigeno, Yoshinori Sasaki, Mika Otonari-Yamamoto, Hitoshi Ohata, and Takahiko Shibahara declare that they have no conflict of interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for which identifying information is included in this article.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Shigeno, K., Sasaki, Y., Otonari-Yamamoto, M. et al. Evaluating the mandibular condyles of patients with osteoarthritis for bone marrow abnormalities using magnetic resonance T2 mapping. Oral Radiol 35, 272–279 (2019). https://doi.org/10.1007/s11282-018-0357-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-018-0357-5