Abstract
Purpose
To assess the frequency and the predictive factors of Acute Kidney injury (AKI) in patients undergoing percutaneous nephrolithotomy (PNL).
Methods
A prospective observational work. Demographic, preoperative laboratory data, stone characteristics, and intraoperative and postoperative data were gathered. Perioperative AKI had been defined as an elevation in serum creatinine by ≥ 0.3 mg/dl within 48 h, or ≥ 1.5 times baseline, or urine volume less than 0.5 ml/ kg/hour for 6 hours. A multivariate logistic regression analysis was performed to determine the predictive factors of AKI. ROC curves were utilized to determine the cutoff values of the risk variables. P-values were deemed statistically significant when they were less than 0.05.
Results
A total of 418 participants had been involved. The frequency of AKI was 13.9, and 17.2% of patients with AKI developed CKD. The risk factors were age > 46.5 years, smoking, BMI > 28.5 kg/m2, hypertension, diabetes, utilization of angiotensin-converting enzyme inhibitors (ACEI), haemoglobin < 10.8 gm/dl, baseline creatinine > 1.41 mg/dl, eGFR < 65.2 ml/min./1.73 m2, serum uric acid > 5.2 mg/dl, stone volume > 1748 mm3, large tract size, long operative time, and intra-operative bleeding. Patients with AKI had a notably extended duration of hospitalization (3.2 days ± 0.45 vs 2.1 ± 0.42, p < 0.001).
Conclusions
Perioperative AKI occurred in 13.9% of individuals undergoing PNL. Identification and optimization of the risk factors and meticulous technique during PNL procedures should be attempted to decrease the risk of AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous nephrolithotomy (PNL) is the preferred therapy for large, intricate, and numerous renal stones, as well as smaller ones that do not respond to extracorporeal-shock waves lithotripsy (ESWL) [1, 2]. PNL Causes direct renal injury by puncturing the renal parenchyma. Also, stones-associated obstruction or infection may affect kidney function, so urologic patients are considered at high risk for acute kidney injury (AKI) [3].
According to Kidney Disease Improving Global Outcomes (KDIGO), AKI is diagnosed based on the presence of one of the followings: an elevation in the serum creatinine ≥ 0.3 mg/dl within 48 h, an elevation in the serum creatinine≥1.5 times more than the basal creatinine level within the proceeding 1 week or urine output≤0.5 ml/kg/h for 6 hours [4, 5].
The pathogenesis of AKI involves multiple interactions between tubular, vascular and inflammatory factors due to injuries caused by ischemia and/or toxins. This leads to endothelial damage, vasoconstriction, and the activation of inflammatory mediators of the immune system [6]. High-pressure irrigation sometimes used during PNL to gain good vision causes pyelorenal backflow, sepsis and renal damage which are directly related to increased intrarenal pressure [7].
AKI is a significant consequence after surgery in urologic patients, with an incidence ranging from 6.7 to 38.2% [8, 9]. It can lead to poor postoperative complications with, sometimes, the need for intensive care unit admission or dialysis with increased morbidity, longer hospital stay, and more cost [10, 11].
The incidence, risk factors, and long-term complications of AKI after PNL are still poorly defined. There is a scarcity of research that documents alterations in the renal function following PNL [12, 13]; hence, defining the risk factors for AKI following PNL is crucial to avoid and minimize its incidence.
Patients and methods
This prospective observational study was carried out on individuals who attended our clinics with renal stones who were amenable to PNL and fulfilled the inclusion criteria from March 2019 to March 2022. The institutional ethics committee approval (approval code: SVU-MED-URO0016-4-22-5-403) was obtained. Each participant provided informed written consent.
Inclusion criteria
All adult patients (age ≥ 18 years) with unilateral renal calculi who were candidates for percutaneous nephrolithotomy with normal contralateral kidneys were included.
Exclusion criteria
Individuals < 18 years, with bilateral renal stones, solitary functioning kidney, active urinary tract infection, bleeding disorders, compromised renal function with serum creatinine < 2 mg/dl (to avoid complications of PNL which are related to high preoperative serum creatinine), urinary tract malignancies and pregnant females had been excluded.
Demographic data that includes age, sex, smoking habits, body mass index (BMI), chronic diseases including hypertension and DM, drug history and preoperative investigations including preoperative assessment of haemoglobin percentage (Hb%), Total leucocytic count (TLC), hematocrit value (HCT%), serum creatinine, estimated glomerular filtration rate (eGFR) utilizing the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) Eq. (2021 update) [14], prothrombin time and concentration, serum uric acid, urine culture (we ensured that all cases had negative urine culture before operation), abdominal ultrasound, non-contrast computed tomography with the assessment of the characteristics of the stones [site, volume of stone in cubic millimetres (stone volume = L × W × D × π × 0.167), and density] were collected.
The intraoperative data including the puncture site, tract size, number of punctures, the demand for blood transfusion, operative time, use of any nephrotoxic drugs, stone clearance by intraoperative fluoroscopy, and any reported intraoperative complications, especially bleeding and hypotension (defined as a mean arterial blood pressure of > 70 mm Hg for < 5 min) were assessed.
Surgical technique
Preoperative 3rd generation cephalosporins were given to all participants. Under general anaesthesia, the patient was positioned in a lithotomy position, and a 5-French ureteral catheter was placed utilizing a 22-French cystoscope. The position of the ureteral catheter was verified utilizing fluoroscopy followed by positioning the patient in the prone postition; a renal puncture by Chiba needle into the desired calyx was done, followed by insertion of the guide-wire, the track was dilated using serial metallic Alken dilators followed by insertion of the Amplatz sheath. The irrigation fluids utilized throughout the procedure had been prewarmed to the body's temperature in the operating room. Pneumatic lithotripsy, utilizing Swiss lithoclast ®, was done, a nephrostomy tube was left after completion of the procedure, and the duration of the operation was determined from the moment the skin was first punctured until it was closed.
Postoperative laboratory investigations involved TLC, Hb, HCT % and serial serum creatinine at 12, 24 and 48 h were reassessed, and all standard blood samples were collected at 08:00 h. Calculation of 48 h of urine output was done for all cases. All patients were advised to maintain sufficient hydration by drinking 3.7 L (15.5 cups) of fluids per day in males and 2.7 L (11.5 cups) of fluids per day in females as advised by the U.S. National Academics of Sciences, Engineering and Medicine. The nephrostomy tube had been removed on the subsequent day after the surgery and the ureteric catheter was removed 2 days after removal of the nephrostomy tube.
The assessment of postoperative complications was conducted with the modified Clavien–Dindo grading scale which consists of 5 grades:
-
1)
Grade 1: Any deviation from the normal postoperative course with no surgical treatment, endoscopic or radiological interventions were required. Acceptable therapeutic regimens are drugs such as anti-emetics, antipyretics, analgesics, and diuretics.
-
2)
Grade 2: Pharmacological management other than grade 1. Blood transfusion and total parenteral nutrition are also included.
-
3)
Grade 3: Complications that require intervention. Grade 3 is subdivided into:
-
a)
Grade IIIa: Complications that require an intervention performed under local anaesthesia.
-
b)
Grade IIIb: Complications that require an intervention performed under general or epidural anaesthesia.
-
a)
-
4)
Grade IV: Life threatening complications requiring ICU admission. Grade 4 is subdivided into:
-
a)
Grade IVa: Single organ dysfunction (including dialysis).
-
b)
Grade IVb: Multiple organ dysfunction.
-
a)
-
5)
Grade V: Death of the patient.
Postoperative abdominal ultrasound and KUB were done for all patients before discharge to document stone clearance or the presence of any residual stones. Participants who had AKI after surgery were monitored by regularly measuring their creatinine levels and eGFR at 1, 3, 6, and 12 months. According to KDIGO, Chronic kidney disease (CKD) was defined by persistently reduced eGFR below 60 mL/min/1.73 m2, or persistent albuminuria [albumin–creatinine ratio {ACR} ≥ 30 mg/g {≥ 3 mg/mmol}], or both [15]. In this study, CKD was defined by an eGFR below 60 mL/min/1.73 m2 at the end of our follow-up period (one year).
Statistical analysis was done utilizing the SPSS version 24. Categorial variables were displayed as frequencies and percentages [n (%)] and were compared using the Chi-square test. Quantitative parameters were displayed as the median and interquartile range (IQR) and were contrasted utilizing Mann–Whitney U test (MW) (as the data was not normally distributed). Univariate linear regression analysis and multivariate logistic regression analysis were utilized to identify AKI risk factors. Receiver operating characteristic (ROC) Curves were utilized to detect the cutoff value, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the studied risk factors of AKI. P-values were deemed statistically significant at p < 0.05.
Aim of the study
The objectives of this study is to assess the incidence of postoperative AKI and to determine the independent risk factors forecasting its possible occurrence in patients undergoing PNL.
Results
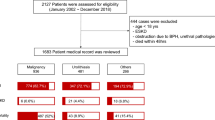
In this work, we assessed 479 individuals for eligibility. After exclusions, 418 patients were enrolled. Patients were allocated into 2 groups: group 1 included fifty-eight patients (13.9%) in whom AKI occurred, and group 2 included three hundred and sixty patients (86.1%) without AKI (non-AKI) (Fig.1).
Details of the demographics of the patients and stone characteristics were collected. Statistically significant variations were found among both groups regarding age [54 (47–58) vs 36 (29–45); p < 0.001], smoking status, BMI, presence of DM and hypertension, utilization of ACEI, preoperative Hb, creatinine, eGFR, and serum uric acid. No statistically significant variations existed regarding the characteristics of the stones except for the stone burden, which was more in the AKI group (p < 0.001) (Table 1).
Regarding the intraoperative data, statistically significant variations were found among both groups regarding tract size (p = 0.003), operative time [80 (70–94) vs 68.5 (64–74) minutes; p < 0.001), need for intraoperative blood transfusion (37.9% vs 0.6%; p < 0.001), occurrence of intraoperative bleeding and hypotension (24.1% vs 0.6% and 20.7% vs 0% correspondingly; p < 0.001). No statistically substantial variations existed regarding the puncture site and the number of punctures (Table 2).
Using univariate linear regression analysis, we found that diabetes, hypertension, high baseline serum creatinine, low baseline eGFR, high levels of serum uric acid and intra-operative bleeding were the predictive factors of AKI (Table 3). Multivariate analysis of logistic regression showed that older age, smoking, high BMI, diabetes, hypertension, use of ACEI, lower preoperative haemoglobin, high baseline creatinine, low baseline eGFR, high serum uric acid level, large stone volume, large tract size, long operative time, and intra-operative bleeding were the factors predicting the occurrence of AKI (Table 4).
The adjusted Clavien-Dindo grading system was used to record postoperative complications (Table 5). Thirty-two cases developed postoperative low-grade fever, all managed by IV paracetamol. Twelve cases developed mild to moderate haematuria; eight were managed conservatively by IV fluids and haemostatic drugs, and four needed blood transfusion. Four cases complained of leakage from the site of the nephrostomy tube site after removing the ureteric catheter. Postoperative non-enhanced CT was done for these cases, and it revealed a stone in the middle third ureter in 3 cases and the lower third in one case; all were treated by ureteroscopy with double J stent insertion. Two cases developed a postoperative pneumothorax (in these cases, the supracostal puncture was done), and were managed by inserting an intercostal tube.
The duration of hospitalization was substantially longer in patients with AKI compared to patients without AKI (3.2 days ± 0.45 vs 2.1 ± 0.42, p < 0.001).
The amount of 48-h postoperative urine output had been substantially decreased in patients with AKI compared to those without AKI [2450 (2350–2575) ml vs 5100 (4862–5250) ml, p < 0.001]. Postoperative serum creatinine values at 48 h follow-up were substantially higher in AKI patients than those without AKI [1.95 (1.7–2.1) vs 1.16 (1–1.26), p < 0.001] (Table 6).
Following 1 year of follow-up of individuals who developed AKI, we found no statistically significant variations between the preoperative and one-year postoperative values of serum creatinine and eGFR [1.52 (1.3–1.6) vs 1.48 (1.33–1.59), p = 0.981, 59.6 (56.5–69.5) vs 60.5 (55.2–69.1), p = 0.907, respectively] (Table 7). All patients with AKI were managed conservatively with no need for renal replacement treatment. In the AKI group, six patients had preoperative eGFR < 60 mL/min/1.73 m2 and continued as patients with CKD. At the end of one year of follow-up, ten new patients (17.2%) in the AKI group with preoperative eGFR > 60 mL/min/1.73 m2 developed CKD [eGFR = 49 (45.1–53.5) mL/min/1.73m2, minimum = 38.2 mL/min/1.73 m2, and maximum = 54.4 mL/min/1.73 m2), and all were managed conservatively.
ROC curves were constructed for the parameters, which included age, BMI, hemoglobin %, serum creatinine, eGFR, serum uric acid, and size of stone to generate a cutoff value for the significant factors identified by both univariate and multivariate analysis, with clinical and statistical significance. The cutoff value for age was > 46.5 years (79.3% sensitivity, 77.8% specificity, 78.1% PPV and 78.9% NPV, p < 0.001); for BMI, it was > 28.5 kg/m2 (75.9% sensitivity, 86.1% specificity, 84.5% PPV and 78.1% NPV, p < 0.001), for hemoglobin level, it was < 10.8 gm/dl (55.2% sensitivity, 78.9% specificity, 72.3% PPV and 63.8% NPV, p = 0.002), for serum creatinine, it was > 1.41 mg/dl (82.8% sensitivity, 89.4% specificity, 88.7% PPV and 83.8% NPV, p < 0.001), for eGFR, it was < 65.2 ml/min/1.73 m2 (85.7% sensitivity, 85% specificity, 85.1% PPV and 85.6% NPV, p < 0.001), for serum uric acid, it was > 5.2 mg/dl (79.3% sensitivity, 85% specificity, 84.1% PPV and 80.4% NPV, p < 0.001), and for the stone volume, it was > 1748 mm3 (68.9% sensitivity, 60% specificity, 63.3% PPV and 65.8% NPV, p < 0.001).
Discussion
Although the main target in managing renal stones is to improve kidney function, this management may sometimes lead to adverse effects, which may occur at all levels of procedures from ESWL to PNL and open surgery. The prevalence of postoperative AKI following significant urological surgeries ranges from 6.7 to 38.2% [5, 9,10,11]. Few studies report AKI after PNL [12, 16, 17]; this may be explained as impairment of renal function without substantial perioperative problems seems minor and may pass unnoticed. AKI may increase postoperative morbidity, mortality, need for postoperative ICU admission, and demand for renal replacement treatment, so every attempt to accurately define the predictors of AKI should be made.
In the current work, we found that the incidence of AKI after PNL was 13.9%, which is consistent with the incidence described in the existing literature [5, 9,10,11, 18]. Age, smoking, BMI, diabetes, hypertension, use of ACEI, low preoperative haemoglobin, high baseline Creatinine, low baseline eGFR, high serum uric acid level, larger stone volume, large tract size, long operative time, and intra-operative bleeding were the predictive factors of AKI.
Renal function is affected by age as elderly patients usually suffer from associated comorbidities such as hypertension, DM, and coronary diseases; also, aging affects the cellular repairing process and decreases the ability to protect against cellular injuries, so these age-related changes may increase the susceptibility of AKI in elderly patients [19,20,21]. A work done by Sunil et al. demonstrated that aging is a risk indicator of AKI, which is in accordance with the current study [22].
The use of ACEI or angiotensin II inhibitors may cause renal hypoperfusion, so the use of these drugs should be considered as a risk factor for AKI. ACEI and angiotensin II receptor blockers may induce intraoperative hypotension by reducing the sensitivity to catecholamines in the renin-angiotensin system when under general anaesthesia, therefore, it is recommended to discontinue the usage of these medications on the day of the surgery [22, 23]. A work done by Sunil et al. demonstrated that the use of ACEI or angiotensin II inhibitors is a risk factor for AKI risk, which is in accordance with the current study [22].
Diabetes is recognized to possess negative impacts on the renal parenchyma and is usually associated with autonomic neuropathy that may cause some perioperative hemodynamic changes [24]. Studies performed by Sunil et al., Fayad et al., and Odzen et al. define diabetes as a risk factor for AKI [22, 25, 26].
Hypertension has a negative impact on renal function. It increases the incidence of intraoperative anaesthetic complications and intraoperative bleeding. Studies by Sunil et al. and Fayad et al. found that hypertension is a risk factor for AKI [22, 25].
This research found that low preoperative haemoglobin and high serum creatinine levels were predictive factors for postoperative AKI, especially in individuals with preoperative Hb < 10.8 g/dl and individuals who had a preoperative creatinine > 1.41 mg/dl. Research by Fulla et al., Sunil et al., and Fayad et al. defined the same factors as predictors of AKI [16, 22, 25].
Elevated levels of serum uric acid lead to the initiation of a proinflammatory process that, in turn, leads to malfunction of the endothelial cells. This dysfunction impairs autoregulation causing constriction of blood vessels in the kidneys and reduced blood flow [27, 28]. Research conducted by Yu et al. and Sunil et al. identified that elevated levels of serum uric acid are predictors of AKI [12, 22].
Multiple punctures and a larger tract size result in substantial nephron injury, increase the operative time and the possibility for perioperative complications and were identified as risk factors of AKI [17, 29]. However, we did not find the number of tracts to be an independent risk factor in this work, as all our cases were done through 1–2 punctures.
Stone factors such as large stones and stones with high density increase the complexity and the operative time of the procedure, with the increased possibility of perioperative blood loss and infectious complications leading to a higher risk of AKI. Multiple previous studies defined these stone factors as predictors of AKI [16, 17, 30].
Intraoperative hypotension (defined as mean arterial blood pressure of less than 70mm Hg for more than 5 min), can cause about 2/3 of cases of acute tubular necrosis and may lead to postoperative AKI. This may explain why intraoperative blood loss, perioperative blood transfusion or low preoperative haemoglobin levels are risk factors for AKI [31]. A work by Yu et al. detected that intraoperative hypotension was a major risk factors for AKI [12].
AKI results in an extended duration of hospitalization. In our work, the mean time of hospital stay was significantly longer in patients with AKI than those without AKI (3.2 days ± 0.45 vs 2.1 ± 0.42, p < 0.001).
Limitations of the study
This work had some limitations including relatively small number of patients, short follow-up period, and proteinuria, as a KDIGO criterion for CKD, was not assessed.
Conclusions
In the current study, we found that age, smoking, BMI, diabetes, hypertension, use of ACEI, low preoperative haemoglobin, high baseline creatinine, low baseline eGFR, high uric acid level, large stone volume, large tract size, long operative time, and intra-operative bleeding were the predictive factors of AKI. 13.9% of our cohort patients developed AKI, so identification and optimization of these risk factors and meticulous technique during the PNL procedures have to be taken into consideration to avoid and lower the incidence of postoperative AKI.
Data availability
All available data were included in the figures and tables.
References
Olbert PJ, Hegele A, Schrader AJ et al (2007) Pre and perioperative predictors of short-term clinical outcomes in patients undergoing percutaneous nephrolitholapaxy. Urol Res 35:225–230
Miller NL, Lingeman JE (2007) Management of kidney stones. BMJ 334:468–472
Caddeo G, Williams ST, McIntyre CW, Selby NM (2013) Acute kidney injury in urology patients: incidence, causes and outcomes. Nephrourol Mon 5(5):955–961
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Okusa MD, Davenport A (2014) Reading between the (guide) lines: The KD IGO practice guideline on acute kidney injury in the individual patient. Kidney Int 85:39–48
Bonventre JV (2010) Pathophysiology of AKI: injury and normal and abnormal repair. Contrib Nephrol 165:9–17
Tokas T, Herrmann TRW, Skolarikos A et al (2019) Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol 37(1):125–131
Joung KW, Choi SS, Kong YG et al (2015) Incidence and risk factors of acute kidney injury after radical cystectomy: importance of preoperative serum uric acid level. Int J Med Sci 12:599–604
Caddeo G, Williams ST, McIntyre CW et al (2013) Acute kidney injury in urology patients: incidence, causes and outcomes. Nephrourol Mon 5:955–961
Chertow GM, Burdick E, Honour M et al (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Hobson C, Ozrazgat-Baslanti T, Kuxhausen A et al (2015) Cost and mortality associated with postoperative acute kidney injury. Ann Surg 261:1207–1214
Yu J, Park HK, Kwon H-J et al (2018) Risk factors for acute kidney injury after percutaneous nephrolithotomy: Implications of intraoperative hypotension. Medicine (Baltimore) 97(30):e11580–e11580
Bilen CY, Inci K, Kocak B, Tan B, Sarikaya S, Sahin A (2008) Impact of percutaneous nephrolithotomy on estimated glomerular filtration rate in patients with chronic kidney disease. J Endourol 22(5):895–900
Inker LA et al (2021) New creatinine- and cystatin c-based equations to estimate gfr without race. N Engl J Med 385(19):1737–1749
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group (2022) KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int 102(5S):S1-S127
Fulla J, Calle J, Elia M, Wright H, Li I (2020) MP22–03 Acute kidney injury and percutaneous nephrolithotomy: Frequency and predictive factors. J Urol 203(Suppl. 4):e328
El-Nahas AR, Taha DE, Ali HM, Elshal AM, Zahran MH, El-Tabey NA, El-Assmy AM, Harraz AM, Moawad HE, Othman MM (2017) Othman Acute kidney injury after percutaneous nephrolithotomy for stones in solitary kidneys. Scand J Urol 51:165–169
Thongprayoon C, Cheungpasitporn W, Akhoundi A, Ahmed AH, Kashani KB (2014) Actual versus ideal body weight for acute kidney injury diagnosis and classification in critically Ill patients. BMC Nephrol 15:176
Chronopoulos A, Rosner MH, Cruz DN, Ronco C (2010) Acute kidney injury in the elderly: a review. Contrib Nephrol 165:315–321
Rosner M (2009) The pathogenesis of susceptibility to acute kidney injury in the elderly. Curr Aging Sci 2(2):158–164
Chao C-T, Tsai H-B, Wu C-Y et al (2015) Cumulative cardiovascular polypharmacy is associated with the risk of acute kidney injury in elderly patients. Medicine 94(31):e1251
Pillai S, Kriplani A, Chawla A, Somani B, Pandey A, Prabhu R, Choudhury A, Pandit S, Taori R, Hegde P (2021) Acute kidney injury post-percutaneous nephrolithotomy (pnl): prospective outcomes from a university teaching hospital. J Clin Med 10(7):1373
Comfere T, Sprung J, Kumar MM et al (2005) Angiotensin system inhibitors in a general surgical population. Anesth Analg 100:636–644
Oakley I, Emond L (2011) Diabetic cardiac autonomic neuropathy and anesthetic management: review of the literature. AANA J 79:473–479
Fayad AS, Elsheikh MG, Mosharafa A, El-Sergany R, Abdel-Rassoul MA, Elshenofy A et al (2014) Effect of multiple access tracts during percutaneous nephrolithotomy on renal function: evaluation of risk factors for renal function deterioration. J Endourol 28(7):775–779
Ozden E, Mercimek MN, Bostanci Y et al (2012) Long-term outcomes of percutaneous nephrolithotomy in patients with chronic kidney disease: a single-center experience. Urology 79(5):990–994
Cheungpasitporn W, Thongprayoon C, Harrison AM, Erickson SB (2016) Admission hyperuricemia increases the risk of acute kidney injury in hospitalized patients. Clin Kidney J 9:51–56
Ejaz AA, Johnson RJ, Shimada M, Mohandas R, Alquadan KF, Beaver TM, Lapsia V, Dass B (2019) The role of uric acid in acute kidney injury. Nephron 142:275–283
Rashid AO, Fakhulddin SS (2016) Risk factors for fever and sepsis after percutaneous nephrolithotomy. Asian J Urol 3:82–87
De la Rosette J, Zuazu JR, Tsakiris P, Elsakka AM, Zudaire JJ, Laguna MP, de Reijke TM (2008) Prognostic factors and percutaneous nephrolithotomy morbidity: A multivariate analysis of a contemporary series using the Clavien classification. J Urol 180:2489–2493
Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, Liu KD, Mehta RL, Pannu N, Van Biesen W, Vanholder R (2013) Acute kidney injury: an increasing global concern. Lancet 382(9887):170–179
Acknowledgements
I would like to acknowledge my patients for their contribution to the study
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research received no external funding.
Author information
Authors and Affiliations
Contributions
AMH: Concept, protocol, data collection, manuscript writing AMR: revision of the manuscript, data collection MARA: data analysis, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest related to this publication.
Institutional review board
Institutional ethics committee approval: SVU-MED-URO0016-4-22-5-403.
Informed consent
Informed consent was obtained from all participants involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hasan, A.M., Riyad, A.M. & Ahmed, M.A. Predictors of acute kidney injury after percutaneous nephrolithotomy in adult patients: prospective observational study. Int Urol Nephrol 56, 1843–1850 (2024). https://doi.org/10.1007/s11255-024-03960-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-024-03960-7