Abstract
Purpose
To identify the risk factors for 5-year cancer-specific (CSS) and overall survival (OS) and to compare the accuracy of logistic regression (LR) and artificial neural network (ANN) in the prediction of survival outcomes in T1 non-muscle-invasive bladder cancer.
Methods
This is a population-based analysis using the Surveillance, Epidemiology, and End Results database. Patients with T1 bladder cancer (BC) who underwent transurethral resection of the tumour (TURBT) between 2004 and 2015 were included in the analysis. The predictive abilities of LR and ANN were compared.
Results
Overall 32,060 patients with T1 BC were randomly assigned to training and validation cohorts in the proportion of 70:30. There were 5691 (17.75%) cancer-specific deaths and 18,485 (57.7%) all-cause deaths within a median of 116 months of follow-up (IQR 80–153). Multivariable analysis with LR revealed that age, race, tumour grade, histology variant, the primary character, location and size of the tumour, marital status, and annual income constitute independent risk factors for CSS. In the validation cohort, LR and ANN yielded 79.5% and 79.4% accuracy in 5-year CSS prediction respectively. The area under the ROC curve for CSS predictions reached 73.4% and 72.5% for LR and ANN respectively.
Conclusions
Available risk factors might be useful to estimate the risk of CSS and OS and thus facilitate optimal treatment choice. The accuracy of survival prediction is still moderate. T1 BC with adverse features requires more aggressive treatment after initial TURBT.
Similar content being viewed by others
Introduction
Bladder cancer (BC) is the tenth most common cancer worldwide with a significant morbidity burden associated with high recurrence and progression rates [1]. The majority of bladder tumours are diagnosed early—at the stage of non-muscle-invasive disease (NMIBC) [2]. Among NMIBC, T1 tumours which are recognized when cancer infiltrates the submucosa, constitute the most aggressive type, associated with a high progression risk and non-negligible mortality [3, 4]. T1 BC is an insidious disease, which might shortly progress to the muscle-invasive stage (up to 20% of patients progress) and the 5-year cancer-specific mortality (CSM) approximates 10% [3]. Transurethral resection of the bladder tumour (TURBT) with adjuvant intravesical Bacillus Calmette Guerin (BCG) therapy remains a standard treatment for T1 tumours and is most commonly chosen [2]. Such therapeutic approach can be insufficient to provide long-term disease-free survival [5]. Thus, definitive surgery (radical cystectomy) should be considered in T1 bladder cancer as it is characterized by higher efficacy in terms of disease eradication [2]. However non-negligible complication rate and morbidity constitute a major disadvantage of radical cystectomy (RC), thus it is still rarely chosen as a treatment option for T1 NMIBC [6]. Moreover, RC might be considered overtreatment in the majority of cases [7, 8]. On the other hand, deferred RC after NMIBC progression to muscle-invasive disease (MIBC) is associated with compromised survival compared to early RC in high-risk NMIBC [9, 10].
European Organisation for Research and Treatment of Cancer (EORTC) and Club Urologico Español de Tratamiento Oncologico (CUETO) scoring models are well-established tools for the estimation of recurrence- and progression-free survival in NMIBC [4, 11]. Currently used nomograms are based on machine learning techniques with Cox proportional hazards (CPH) [4, 11, 12]. Above tools provide moderate accuracy and new approaches to predict the disease course are awaited [2]. This includes the pursuit of novel molecular markers and new risk factors which affect the course of the disease, but also the implementation of novel prediction tools [5]. Moreover, overall- (OS) and cancer-specific survival (CSS) are not frequently studied endpoints in NMIBC and above scoring systems were not designed to be used in that setting [4, 11, 12].
Artificial intelligence becomes an attractive option, with deep learning as a promising tool for pattern recognition and outcome prediction [13, 14]. Deep learning uncovers complex structures in large datasets by using the backpropagation algorithm to indicate how an algorithm should adjust its internal parameters that are used to compute the representation in each layer from the representation in the previous layer [14]. Deep learning-based techniques have been already shown to provide an accuracy advantage in bladder cancer recurrence and progression prediction [15]. Artificial neural network (ANN) constitutes one of the most commonly used methods of deep learning and provides many benefits (e.g. ability to implicitly detect complex nonlinear relationships between dependent and independent variables) but it is not devoid of limitations (e.g. the ‘black-box’ problem) [16]. One of the studies showed the accuracy benefit of ANN compared to the CPH model in the prediction of CSS, but not OS in bladder cancer patients treated with cystectomy [17]. There is a particular necessity to estimate the risk of progression and cancer-specific death in T1 BC to qualify patients, who are at risk, for more radical treatment—early RC [2]. This unmet need constituted the rationale to focus on mortality prediction in this particular group of bladder cancer patients, in whom therapeutic decisions are especially challenging. On the other hand, overall- and other-cause mortality is another outcome requiring attention to facilitate the selection of patients for more conservative management and thus avoiding overtreatment.
In this population-based study, we aimed to identify factors associated with OS and CSS in patients with T1 NMIBC treated with TURBT. Furthermore, we aimed to compare the utility of ANN and conventional machine learning tools – LR in the prediction of 5-year CSS and OS in patients with T1 NMIBC.
Methods
The Surveillance, Epidemiology, and End Results (SEER) database (2004–2015) which consists of seventeen different registries, lastly updated in November 2021 was used for this research. The SEER*Stat statistical software was used to select patients meeting the study criteria. A systematic search was performed to identify patients, who were diagnosed with T1 NMIBC between 2004 and 2015, in accordance with the 6Th Derived American Joint Committee on Cancer (AJCC) T edition (ICD-10 codes from C67.0 to C67.9 with the exclusion of C67.7—urachal tumour). In the further selection, only patients treated with TURBT were included in the analysis. We excluded patients with evidence of nodal involvement or distant metastases, with unknown metastatic status due to lack of imaging studies, previous radiotherapy for BC, previous evidence of muscle-invasive BC, missing tumour characteristics (e.g. grading), and unknown survival status.
The available data included information on the patient’s sociodemographics, tumour histopathological (e.g. T category, grading) and clinical characteristics (e.g. tumour size, location, history of the previous tumour defined as non-primary bladder malignancy), a therapy used (e.g. surgery type, chemotherapy) and survival outcomes (cancer and all-cause mortality during the follow-up). The 5-year OS and CSS was calculated for patients with sufficient follow-up as previously reported [18, 19].
The dataset was divided into training and validation cohorts in the proportion of 70 to 30. Group characteristics are presented in the respective table with the number of patients and percentage for categorical variables and medians, accompanied by the interquartile range (IQR) for continuous variables.
Statistical analysis
Statistical analyses were conducted in SAS software (Cary, NC, U.S.) version 9.4 and using R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria). Multivariable analyses using LR and CPH with stepwise selection of variables were performed in SAS software. Odds ratio (OR) and hazard ratio (HR) supplemented with a 95% confidence interval (95% CI) were derived from multivariable regression. For all statistical analyses, we considered a two-sided p value < 0.05 as statistically significant.
Artificial neural networks were developed using R language and ‘neuralnet’ package. A resilient backpropagation algorithm (‘Rprop + ’) was utilized with one layer and four hidden neurons (vertices) to predict 5-year survival outcomes. Only factors that were significantly associated with mortality in multivariable analyses with LR were used as input variables to build a neural network. Cross-entropy was used as a differentiable function for the calculation of the error. The threshold specifying the partial derivatives of the error function as stopping criteria in neural network creation was set as 0.1. Each learning process for ANN included two repetitions.
Separate predictive models for 5-year OS and 5-year CSS were developed using both LR and ANN in the training cohort. Then, all models were tested in the validation cohort. The area under the curve (AUC) for receiver operating characteristic (ROC) and model accuracy derived from the confusion matrix were calculated. Accuracy was defined as the proportion of correct predictions to all predictions.
Results
Clinicopathologic features
Overall 32,060 patients with T1 bladder cancer who underwent TURBT were included in the analysis, 22,442 patients were subjected to the training cohort and 9618 patients to the validation one respectively. Training and validation cohorts did not differ in the frequency of characteristics and outcomes (Table 1). The majority of patients were males (N = 25,049; 78%), of the white race (N = 28,587; 89%) and over 70 years of age (N = 19,955; 62%). High-grade tumours (N = 22,115; 69%), mostly of urothelial histology (N = 31,265; 97.5%) were predominant. The majority of tumours were located in the anterior/posterior or lateral bladder walls (N = 12,020; 37.5%) or the location was not specified (e.g. multiple location) (N = 13,722; 42.8%), less frequently tumours originated from the bladder neck or trigone (N = 2802; 8.7%), or extended through more than one area of the bladder (N = 3516; 11%). The vast majority of patients presented with primary T1 bladder tumour (N = 29,055; 90.6%) and 9.4% had a previous history of NMIBC.
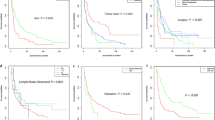
Survival outcomes
Cancer-specific deaths occurred in 22.6% of cases (N = 7230), whereas all-cause mortality exceeded 57.6% (N = 18,485) during the median follow-up of 116 months (IQR 80–153 months). The 5-year OS exceeded 58%. Noteworthy, 9028 patients, who were excluded from the prediction of 5-year CSS included those who were lost to follow-up (N = 2156; 6.7%) and those who died of other causes before 5 years of follow-up (cardiovascular diseases—2658 pts/ 8.3%; other cancer—1563 pts/4.9%; lung diseases and infections 759/2.3% and other mortality causes 1868 pts/5.8%). These exclusions were made due to competing event in the majority of cases and lost to follow-up in the minority. Comparison of included and excluded patients’ characteristics are shown in the supplementary table 1.
CSS prediction with LR and ANN
Multivariable analyses with LR were performed and revealed tumour grade (high-grade vs low-grade; HR = 2.07 95% CI 1.88–2.29 p < 0.001), size (≥ 3 cm vs < 3 cm; HR = 1.36 95% CI 1.19–1.56 p < 0.05), histology variant (squamous vs urothelial; HR = 5.56 95% CI 3.88–7.96 p < 0.001; other vs urothelial; HR = 3.38 95% CI 2.53–4.51 p < 0.001), location (lateral/posterior/anterior wall vs trigone/neck; HR = 0.78 95% CI 0.66–0.91 p < 0.001; more than one bladder area vs trigone/neck; HR = 1.20 95% CI 1.00–1.44 p < 0.001; not specified/multiple tumour location vs trigone/neck HR = 1.11 95% CI 0.95–1.44 p < 0.01), primary tumour character (recurrent vs primary; HR = 1.60 95% CI 1.40–1.83 p < 0.001), patient’s age (> 80 yr vs < 60 yr; HR = 7.35 95% CI 6.29–8.60 p < 0.001; 70–80 yr vs < 60 yr; HR = 2.50 95% CI 2.13–2.93 p < 0.05; 60–70 yr vs < 60 yr; HR = 1.48 95% CI 1.25–1.76 p < 0.01), race (black vs white; HR = 1.58 95% CI 1.33–1.88 p < 0.001; other vs white; HR = 0.83 95% CI 0.68–1.00 p < 0.001), marital status (married vs unmarried; HR = 0.68 95% CI 0.63–0.75 p < 0.001) and annual income (higher vs lower; HR = 0.90 95% CI 0.83–0.98 p < 0.05) as factors predicting 5-year CSS (Table 2). The discrimination of the LR-based model reflected by the area under the ROC curve was 73.4%, whereas the accuracy of prediction exceeded 79.5% in the validation cohort. Using the same variables ANN was created and achieved the same AUC and accuracy as LR in the validation cohort (72.5% and 79.4% respectively). Moreover, for both, LR and ANN predictions’ accuracy and AUC were comparable in the training and validation cohorts, which pinpoints the small risk of overfitting. Multivariable analyses performed using CPH and LR revealed the same risk factors for CSS (supplementary table 2).
OS prediction with LR and ANN
The following factors were significant predictors of 5-year OS: tumour grade, size, histology variant, location, patient’s age, race and gender, presence of other malignancy, marital status, annual income, and metropolitan citizenship (Table 3). AUC for the LR and ANN models were 74.3% and 74.2% respectively in the training cohort. Similarly, in the validation cohort, the LR-based model and ANN achieved the same AUC (73.7% vs 73.4% respectively) and same accuracy (69.1% vs 69.3% respectively) for the prediction of 5-year OS. Summarized values of accuracy and AUC for both ANN and LR-based models predicting CSS and OS are presented in the Table 4.
Discussion
In this population-based study involving 32 060 patients with T1 bladder cancer, we aimed to identify predictive factors for survival and compare the accuracy of 5-year CSS and OS predictions with the use of ANN and LR-based models. Firstly and most importantly, multiple factors are associated with unfavourable CSS including clinical and histopathological features: older age, higher histological grade, non-urothelial histology variants, tumour size ≥ 3 cm, recurrent tumour, tumour location, and sociodemographic features such as black race, non-married status and lower annual income.
Secondly, the analysis showed that ANN is a feasible prediction tool with acceptable, moderate accuracy in survival estimation. Thirdly, ANN and conventional machine learning method—LR-based model exhibit the same discrimination and prediction accuracy for 5-year CSS and OS in T1 NMIBC. Forth, pursuit for better prognostic tools in T1 BC is of great significance as the reported real-world survival outcomes remain poor.
The above results raise the question if the neural network is a valid approach for survival model creation. The accuracy was no better than the one of the conventional LR models. Moreover, identical prediction factors as for LR were provided for ANN and yielded the same accuracy. The obvious drawback of the ANN is the ‘black-box’ problem, which means that we cannot exactly know which factors play the most significant role and how the ANN learning process goes on. However, as ANN seem to be not inferior to LR it must be considered a valid approach to be used in future studies and web applications for clinical use. Perhaps the optimization (e.g. hyperparameters modification) might be a clue to the success and ANN models could become a valuable tool for clinical implementation. Disadvantages coming from the so-called ‘black-box’ problem are also possible to overcome as suggested by some authors [20]. Moreover, such black-box algorithms can allow the health system to leverage complex biological relationships well before those relationships are understood [21].
Artificial intelligence with the underscored role of deep-learning techniques such as neural networks has an undeniable role to play in current and future medicine [22]. It can assist pathologists and radiologists in image analysis or even replace specialists in some cases and spare human healthcare resources [22]. Current studies show very promising accuracy of image recognition, even more accurate than the assessment performed by physicians [23]. The benefits of neural networks can be also harnessed in the field of oncology for molecular studies, pharmacogenomics, microscopic assessment and prognosis prediction [24].
Widely used EORTC and CUETO risk scores or EAU risk groups were not designed to estimate the risk of cancer-specific or overall mortality. Above classifications were established to stratify patients according to the progression- and/or recurrence-free survival, but not CSS [4, 11, 12]. The studies predicting CSS in high-risk NMIBC, including the group of T1 bladder tumours are lacking. In our analysis, cancer-specific deaths were recorded in 22.5% of patients within a median follow-up of 166 months (IQR 80–153). A systematic review of prospective trials including 1183 high-risk NMIBC patients (mainly T1 stage) reported an average of 15% of CSM within shorter follow-up (median from 52 to 123 months, ranging between studies) [25]. Thus, we argue that due to its aggressiveness, T1 NMIBC should be also regarded as potentially deadly and risks of both progression and cancer-specific death should be estimated to aid clinical decision-making.
We identified clinical, histopathological and sociodemographic factors that were independently associated with CSS. These included obvious factors such as high-grade tumour, history of previous NMIBC and non-urothelial histology variants. High-grade histology is the strongest risk factor for progression in NMIBC [26] and is most commonly reported for T1 tumours, which are almost always considered ‘high-risk’ as they infiltrate the submucosa of the bladder [27]. To date, the significance and prognosis of low-grade T1 tumours were enigmatic. However, recent multicenter retrospective studies showed that T1G1 are characterized by a significantly higher progression rate than TaG1 tumours [27] and T1LG conferred a better prognosis than T1HG [28]. Nonetheless, our analysis supports the rationale for cautious and precise grading assessment in T1 tumours (although being always ‘high-risk’, T1 is not always high-grade). Recognition of low-grade T1 is possible, necessary and rationalized by the distinct prognosis of T1 low-grade and high-grade tumours, which is also confirmed in our study. The history of previous NMIBC is a known risk factor for further recurrences and progression in T1, which was already mentioned in other studies [4, 11]. Finally, non-urothelial histology of BC confer a risk factor for progression [29]. Pure SCC is not responsive to BCG and characterized by higher progression rates and should be a priori treated with RC [30]. Therefore, T1 patients with SCC and other than pure urothelial variants of histology should be counselled on high progression risk following sole TURBT and informed on the benefits of RC. Other factors such as older age, large tumour size and multiple locations of the tumour are also underlined as predictors of progression in multiple studies [3, 4, 11, 12]. Especially challenging is the therapeutic strategy in elderly patients who on the one hand are at high risk for complications after cystectomy, but on the other hand, are at highest risk of progression when treated with bladder-sparing approach [12, 31, 32]. Perhaps optimization of adjuvant intravesical therapies is most desirable to prevent progression in elderlies, who are unfit for RC. Important, but tremendous conclusions come from the observation that sociodemographic features influence the CSS. The relationship between the lower than median annual income and worse CSS indicates the disparity in access to healthcare and treatment. Black race was shown to confer another risk factors which might result from genetic dependencies or again unequal access to healthcare providers [33]. The issue of being married as a protective factor has been already shown in other population-based studies in urothelial cancer [34, 35] and this might underline the role of supportive relatives and partners in the process of treatment and strict follow-up.
Factors influencing the OS were similar to those predicting CSS. The following factors were associated with worse OS: high-grade tumour, tumour size ≥ 3 cm, non-urothelial histology, tumour location, older age, black race, male gender, the presence of other malignancy, non-married status, lower annual income and non-metropolitan citizenship. Tumour-related factors such as high-grade histology, variants of histology, and large size contributed to worse OS, most probably due to their association with higher CSM. Older age and the presence of other malignancy increase the risk of all-cause mortality. The male gender was associated with worse OS, which supports the general rule of shorter life expectancy in men. Conversely, consistently other authors show poorer bladder cancer-specific survival in women than in men [36]. Importantly, non-metropolitan citizenship was related to worse survival and this might be attributed to worse accessibility to medical care in rural areas [37]. The association between the development of other primary malignancy and worse OS, underscores the need for other cancer awareness and the necessity to provide holistic care to the patient. Concomitant malignancies in patients with BC seem to originate most often from the prostate or the upper urinary tract [38, 39].
Limitations of the study include the lack of detailed data on the patient comorbidities, smoking habits, and some tumour characteristics (e.g. lymphovascular invasion) and most importantly the quality of surgery (e.g. detrusor muscle in the specimen, macroscopically radical resection) which all have been proven to influence the prognosis [2, 40]. The prediction of OS was mainly limited by the lack of the data on comorbidities. On the other hand, the use of sociodemographic factors (e.g. race, income) might not be reliable prognostic factors in everyday clinical practice. The information about the adjuvant use of intravesical therapies (e.g. BCG) was unreliable in most cases with only a few reports of BCG use despite clear indication for BCG in the majority of T1 BC patients. We might suppose that many patients received BCG, but it was not recorded in the SEER database and this must be considered an important, uncontrolled confounder. Survival outcomes were available for the majority of patients with acceptable median follow-up after surgery, but no relevant information about progression or recurrence could be received. Moreover, in our analysis we did not validate the reliability of EORTC risk tables in CSS prediction. Some variables, including the presence of concomitant carcinoma in situ, were not available, whereas the data on tumour multiplicity was inaccurate. The data about primary character of the tumour and its location in the bladder (according to ICD-10 coding) was available for all patients. Exact tumour diameter was available for the 45% of analysed patients and remaining 55% of patients were assigned as of unknown tumour size (Table 1). Above risk factors contributing to EORTC risk score calculation were therefore not fully available.
Analysis of 5-year OS and CSS required the exclusion of patients with insufficient follow-up which must be regarded as bias. Since both cancer-specific and overall mortality are time-dependent variables, analysing them as binary end-point might raise some methodological concerns and it should be clearly reported as a limitation. We have, however, performed consecutive analyses to confirm the utility of such an approach. Performed CPH analysis yielded the same predictors for CSS as LR. Among patients excluded from survival prediction, only 6.7% were lost to follow-up before 60 months. Other patients which were excluded from CSS analysis, died from other diseases than BC as reported in the results section. The bias of excluding the patients who did not reach the 5-year follow-up was limited by the performed comparison between the analyzed and excluded patients (supplementary table 1). The only main clinically significant difference between included and excluded patients was more advanced age in the latter ones contributing to higher other-cause mortality (supplementary table 1). A binary endpoint (5-year CSM) seems therefore acceptable for the comparison of LR and ANN performance. The accuracy of prediction in the training and validation datasets was very similar which indicates a rather small risk of model overfitting.
To conclude, available predictive factors for CSS and OS might be useful to estimate the risk of 5-year CSS and OS in patients with T1 BC. The accuracy of mortality prediction is still moderate, also when ANN is applied. Patients with T1 BC and adverse features should receive more aggressive treatment after initial TURBT.
Data availability
The datasets analysed during the current study are available from the US National Cancer Institute upon request.
References
Saginala K, Barsouk A, Aluru JS, Rawla P, Padala SA, Barsouk A (2020) Epidemiology of Bladder Cancer. Med Sci (Basel) 8(1):15
Ślusarczyk A, Zapała P, Zapała Ł, Piecha T, Radziszewski P (2019) Prediction of BCG responses in non-muscle-invasive bladder cancer in the era of novel immunotherapeutics. Int Urol Nephrol 51(7):1089–1099
Cambier S, Sylvester RJ, Collette L, Gontero P, Brausi MA, van Andel G et al (2016) EORTC Nomograms and Risk Groups for Predicting Recurrence, Progression, and Disease-specific and Overall Survival in Non-Muscle-invasive Stage Ta-T1 Urothelial Bladder Cancer Patients Treated with 1–3 Years of Maintenance Bacillus Calmette-Guérin. Eur Urol 69(1):60–69
Sylvester RJ, van der Meijden APM, Oosterlinck W, Witjes JA, Bouffioux C, Denis L et al (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49(3):466–465
Ślusarczyk A, Piotr Z, Garbas K, Zapała Ł, Borkowski T, Radziszewski P. Blood count-derived inflammatory markers predict time to Bacillus Calmette-Guérin failure in high-risk non-muscle-invasive bladder cancer. Arch Med Sci [Internet]. 2021 May 5 [cited 2021 Jun 15]; Available from: https://www.archivesofmedicalscience.com/Blood-count-derived-inflammatory-markers-predict-time-to-Bacillus-Calmette-Guerin,130303,0,2.html
Zapała Ł, Ślusarczyk A, Korczak B, Kurzyna P, Leki M, Lipiński P et al (2022) The view outside of the box: reporting outcomes following radical cystectomy using pentafecta from a multicenter retrospective analysis. Front Oncol 12:841852
Jordan B, Meeks JJ (2019) T1 bladder cancer: current considerations for diagnosis and management. Nat Rev Urol 16(1):23–34
De Berardinis E, Busetto GM, Antonini G, Giovannone R, Gentile V (2011) T1G3 high-risk NMIBC (non-muscle invasive bladder cancer): conservative treatment versus immediate cystectomy. Int Urol Nephrol 43(4):1047–1057
Denzinger S, Fritsche HM, Otto W, Blana A, Wieland WF, Burger M (2008) Early versus deferred cystectomy for initial high-risk pT1G3 urothelial carcinoma of the bladder: do risk factors define feasibility of bladder-sparing approach? Eur Urol 53(1):146–152
Grossmann NC, Rajwa P, Quhal F, König F, Mostafaei H, Laukhtina E et al (2022) Comparative outcomes of primary versus recurrent high-risk non–muscle-invasive and primary versus secondary muscle-invasive bladder cancer after radical cystectomy: results from a retrospective multicenter study. Eur Urol Open Sci 1(39):14–21
Fernandez-Gomez J, Madero R, Solsona E, Unda M, Martinez-Piñeiro L, Gonzalez M et al (2009) Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with bacillus Calmette-Guerin: the CUETO scoring model. J Urol 182(5):2195–2203
Sylvester RJ, Rodríguez O, Hernández V, Turturica D, Bauerová L, Bruins HM et al (2021) European Association of Urology (EAU) prognostic factor risk groups for non-muscle-invasive bladder cancer (NMIBC) incorporating the WHO 2004/2016 and WHO 1973 classification systems for grade: an update from the EAU NMIBC guidelines panel. Eur Urol 79(4):480–488
Tufail AB, Ma YK, Kaabar MKA, Martínez F, Junejo AR, Ullah I et al (2021) Deep Learning in cancer diagnosis and prognosis prediction: a minireview on challenges, recent trends, and future directions. Comput Math Methods Med 31(2021):9025470
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521(7553):436–444
Jobczyk M, Stawiski K, Kaszkowiak M, Rajwa P, Różański W, Soria F et al (2022) Deep learning-based recalibration of the CUETO and EORTC prediction tools for recurrence and progression of non-muscle-invasive bladder cancer. Eur Urol Oncol 5(1):109–112
Tu JV (1996) Advantages and disadvantages of using artificial neural networks versus logistic regression for predicting medical outcomes. J Clin Epidemiol 49(11):1225–1231
Bhambhvani HP, Zamora A, Shkolyar E, Prado K, Greenberg DR, Kasman AM et al (2021) Development of robust artificial neural networks for prediction of 5-year survival in bladder cancer. Urol Oncol 39(3):193.e7-193.e12
Bassi P, Sacco E, De Marco V, Aragona M, Volpe A (2007) Prognostic accuracy of an artificial neural network in patients undergoing radical cystectomy for bladder cancer: a comparison with logistic regression analysis. BJU Int 99(5):1007–1012
Snow PB, Kerr DJ, Brandt JM, Rodvold DM (2001) Neural network and regression predictions of 5-year survival after colon carcinoma treatment. Cancer 91(S8):1673–1678
Zhang Z, Beck MW, Winkler DA, Huang B, Sibanda W, Goyal H (2018) Opening the black box of neural networks: methods for interpreting neural network models in clinical applications. Ann Transl Med 6(11):216
Price WN (2018) Big data and black-box medical algorithms. Sci Transl Med. 10(471):eaao5333
Topol EJ (2019) High-performance medicine: the convergence of human and artificial intelligence. Nat Med 25(1):44–56
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL (2018) Artificial intelligence in radiology. Nat Rev Cancer 18(8):500–510
Tran KA, Kondrashova O, Bradley A, Williams ED, Pearson JV, Waddell N (2021) Deep learning in cancer diagnosis, prognosis and treatment selection. Genome Med 13(1):152
van den Bosch S, Alfred WJ (2011) Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: a systematic review. Eur Urol 60(3):493–500
van Rhijn BWG, Hentschel AE, Bründl J, Compérat EM, Hernández V, Čapoun O et al (2021) Prognostic value of the WHO1973 and WHO2004/2016 classification systems for grade in primary Ta/T1 non-muscle-invasive bladder cancer: a multicenter European Association of Urology Non-muscle-invasive Bladder Cancer Guidelines Panel Study. Eur Urol Oncol 4(2):182–191
Beijert IJ, Hentschel AE, Bründl J, Compérat EM, Plass K, Rodríguez O et al (2022) T1G1 bladder cancer: prognosis for this rare pathological diagnosis within the non-muscle-invasive bladder cancer spectrum. Eur Urol Focus S2405–4569(22):00110–00119
van de Putte EEF, Bosschieter J, van der Kwast TH, Bertz S, Denzinger S, Manach Q et al (2018) The World Health Organization 1973 classification system for grade is an important prognosticator in T1 non-muscle-invasive bladder cancer. BJU Int 122(6):978–985
Gofrit ON, Yutkin V, Shapiro A, Pizov G, Zorn KC, Hidas G et al (2016) The Response of variant histology bladder cancer to intravesical immunotherapy compared to conventional cancer. Front Oncol 6:43
Lonati C, Afferi L, Mari A, Minervini A, Krajewski W, Borghesi M et al (2022) Immediate radical cystectomy versus BCG immunotherapy for T1 high-grade non-muscle-invasive squamous bladder cancer: an international multi-centre collaboration. World J Urol 40(5):1167–1174
Froehner M, Brausi MA, Herr HW, Muto G, Studer UE (2009) Complications following radical cystectomy for bladder cancer in the elderly. Eur Urol 56(3):443–454
Ślusarczyk A, Garbas K, Zapała P, Zapała Ł, Radziszewski P (2021) Oncological outcomes of high-grade T1 non-muscle-invasive bladder cancer treatment in octogenarians. Int Urol Nephrol. https://doi.org/10.1007/s11255-021-02870-2
Kotha NV, Kumar A, Qiao EM, Qian AS, Voora RS, Nalawade V et al (2022) Association of health-care system and survival in African American and non-Hispanic white patients with bladder cancer. J Natl Cancer Inst 114(4):600–608
Wang W, Liu J, Liu L (2021) Development and validation of a prognostic model for predicting overall survival in patients with bladder cancer: a SEER-based study. Front Oncol 11:692728
Li K, Wang F, Wang J, Fan C, Sun J (2021) Marital status independently predicts survival of patients with upper urinary tract urothelial carcinoma: a population-based study. J Cancer Res Ther 17(7):1709–1717
Dobruch J, Daneshmand S, Fisch M, Lotan Y, Noon AP, Resnick MJ et al (2016) Gender and bladder cancer: a collaborative review of etiology, biology, and outcomes. Eur Urol 69(2):300–310
Deuker M, Stolzenbach LF, Collà Ruvolo C, Nocera L, Tian Z, Roos FC et al (2021) Bladder cancer stage and mortality: urban vs. rural residency. Cancer Causes Control 32(2):139–145
van Doeveren T, van de Werken HJG, van Riet J, Aben KKH, van Leeuwen PJ, Zwarthoff EC et al (2020) Synchronous and metachronous urothelial carcinoma of the upper urinary tract and the bladder: are they clonally related? A systematic review. Urol Oncol Semin Orig Investig 38(6):590–598
Lopez-Beltran A, Cheng L, Montorsi F, Scarpelli M, Raspollini MR, Montironi R (2017) Concomitant bladder cancer and prostate cancer: challenges and controversies. Nat Rev Urol 14(10):620–629
Ślusarczyk A, Zapała P, Zapała Ł, Radziszewski P (2022) The impact of smoking on recurrence and progression of non-muscle invasive bladder cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-04464-6
Funding
The authors declare that no funds, grants, or other financial support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AŚ and PZ: contributed to the study conception and design. Material preparation, data collection and analysis were performed by AŚ and ZO-Ś. The first draft of the manuscript was written by AŚ and all authors (AŚ, PZ, ZO-Ś, PR) edited and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Due to the study character no Ethics Committee approval was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ślusarczyk, A., Zapała, P., Olszewska-Ślusarczyk, Z. et al. The prediction of cancer-specific mortality in T1 non-muscle-invasive bladder cancer: comparison of logistic regression and artificial neural network: a SEER population-based study. Int Urol Nephrol 55, 2205–2213 (2023). https://doi.org/10.1007/s11255-023-03655-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03655-5