Abstract
Background and objectives
Contrast-induced nephropathy (CIN) is a relatively common complication following primary coronary angiography (CAG) or percutaneous coronary intervention (PCI), especially in at-risk patients. The goal of this study is to evaluate the role of pre-procedural serum osmolarity as a risk factor for CIN in patients undergoing elective CAG for stable coronary artery disease (CAD).
Materials and methods
A total of 356 stable CAD patients scheduled to undergo CAG or PCI were included in this two-center study. Serum osmolarity was calculated on admission. CIN was defined according to the KDIGO criteria.
Results
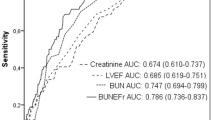
There were 45 (12.6%) patients who developed CIN 48–72 h after CAG or PCI. CIN patients had a higher prevalence of diabetes (51.1% in those with CIN vs 24.4% in those without CIN, p < 0.001), higher serum glucose (129 mg/dL in those with CIN vs 108 mg/dL in those without CIN, p < 0.001), blood urea nitrogen (22.4 mg/dL in those with CIN vs 19.0 mg/dL in those without CIN, p = 0.01) and serum osmolarity (294.2 mOsm in those with CIN vs 290.1 mOsm in those without CIN, p < 0.001) levels, had received a higher dose of contrast (250 mL in those with CIN vs 200 mL in those without CIN, p = 0.03) but had lower hemoglobin (12.9 g/dL in those with CIN vs 13.6 g/dL in those without CIN, p = 0.04) level. In multivariate analysis, serum osmolarity [odds ratio (OR) 1.11; 95% confidence interval (CI) 1.04–1.18 for each mOsm/L increase; p = 0.001], diabetes (OR 2.43, 95% CI 1.26–4.71; p = 0.01), C-reactive protein (OR 1.04, 95% CI 1.01–1.08 for each mg/dL increase; p = 0.02) and contrast volume (OR 34.66, 95% CI 1.25–962.22 for each L increase; p = 0.04) remained as independent predictors of CIN. Serum sodium, glucose and blood urea nitrogen contributed to the excess serum osmolarity of CIN patients.
Conclusion
Serum osmolarity is a cheap and widely available marker that can reliably predict CIN after CAG or PCI. Future research should focus on determining a clinically optimal cutoff for serum osmolarity that would warrant preventive interventions. Furthermore, later research may investigate the role of serum osmolarity not only as a risk factor but also as a pathogenetic mechanism underlying CIN.

Similar content being viewed by others
References
Fliser D, Laville M, Covic A, Fouque D, Vanholder R, Juillard L et al (2012) A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol Dial Transplant. 27(12):4263–4272
Lasser EC, Lyon SG, Berry CC (1997) Reports on contrast media reactions: analysis of data from reports to the U.S. Food and Drug Administration. Radiology 203(3):605–610
Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Berg KJ (2003) Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med. 348(6):491–499
Brar SS, Shen AY, Jorgensen MB, Kotlewski A, Aharonian VJ, Desai N et al (2008) Sodium bicarbonate vs sodium chloride for the prevention of contrast medium-induced nephropathy in patients undergoing coronary angiography: a randomized trial. JAMA 300(9):1038–1046
Heinrich MC, Haberle L, Muller V, Bautz W, Uder M (2009) Nephrotoxicity of iso-osmolar iodixanol compared with nonionic low-osmolar contrast media: meta-analysis of randomized controlled trials. Radiology 250(1):68–86
Rudnick MR, Davidson C, Laskey W, Stafford JL, Sherwin PF (2008) Nephrotoxicity of iodixanol versus ioversol in patients with chronic kidney disease: the Visipaque Angiography/Interventions with Laboratory Outcomes in Renal Insufficiency (VALOR) Trial. Am Heart J. 156(4):776–782
Solomon RJ, Mehran R, Natarajan MK, Doucet S, Katholi RE, Staniloae CS et al (2009) Contrast-induced nephropathy and long-term adverse events: cause and effect? Clin J Am Soc Nephrol. 4(7):1162–1169
Kanbay M, Covic A, Coca SG, Turgut F, Akcay A, Parikh CR (2009) Sodium bicarbonate for the prevention of contrast-induced nephropathy: a meta-analysis of 17 randomized trials. Int Urol Nephrol. 41(3):617–627
Nash K, Hafeez A, Hou S (2002) Hospital-acquired renal insufficiency. Am J Kidney Dis. 39(5):930–936
Mendi MA, Afsar B, Oksuz F, Turak O, Yayla C, Ozcan F et al (2017) Uric acid is a useful tool to predict contrast-induced nephropathy. Angiology 68(7):627–632
Kanbay M, Aslan G, Afsar B, Dagel T, Siriopol D, Kuwabara M et al (2018) Acute effects of salt on blood pressure are mediated by serum osmolality. J Clin Hypertens (Greenwich). 20(10):1447–1454
Kuwabara M, Hisatome I, Roncal-Jimenez CA, Niwa K, Andres-Hernando A, Jensen T et al (2017) Increased serum sodium and serum osmolarity are independent risk factors for developing chronic kidney disease; 5 year cohort study. PLoS ONE 12(1):e0169137
Glaser J, Lemery J, Rajagopalan B, Diaz HF, Garcia-Trabanino R, Taduri G et al (2016) Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 11(8):1472–1483
Hahn K, Kanbay M, Lanaspa MA, Johnson RJ, Ejaz AA (2017) Serum uric acid and acute kidney injury: a mini review. J Adv Res. 8(5):529–536
Kanbay M, Yilmaz S, Dincer N, Ortiz A, Sag AA, Covic A et al (2019) Antidiuretic hormone and serum osmolarity physiology and related outcomes: what is old, what is new, and what is unknown? J Clin Endocrinol Metab. 104(11):5406–5420
Johnson RJ, Rodriguez-Iturbe B, Roncal-Jimenez C, Lanaspa MA, Ishimoto T, Nakagawa T et al (2014) Hyperosmolarity drives hypertension and CKD—water and salt revisited. Nat Rev Nephrol. 10(7):415–420
Yildiz I, Yildiz PO, Rencuzogullari I, Karabag Y, Cagdas M, Burak C et al (2019) Association of Serum Osmolarity With Contrast-Induced Nephropathy in Patients With ST-Segment Elevation Myocardial Infarction. Angiology 70(7):627–632
Farhan S, Vogel B, Baber U, Sartori S, Aquino M, Chandrasekhar J et al (2019) Calculated serum osmolality, acute kidney injury, and relationship to mortality after percutaneous coronary intervention. Cardiorenal Med. 9(3):160–167
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med. 150(9):604–612
ACE Inhibitors in Diabetic Nephropathy Trialist Group (2001) Should all patients with type 1 diabetes mellitus and microalbuminuria receive angiotensin-converting enzyme inhibitors? A meta-analysis of individual patient data. Ann Intern Med 134(5):370–379
Bhagat CI, Garcia-Webb P, Fletcher E, Beilby JP (1984) Calculated vs measured plasma osmolalities revisited. Clin Chem 30(10):1703–1705
Rohla M, Freynhofer MK, Tentzeris I, Farhan S, Wojta J, Huber K et al (2014) Plasma osmolality predicts clinical outcome in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care 3(1):84–92
Tatlisu MA, Kaya A, Keskin M, Uzman O, Borklu EB, Cinier G et al (2017) Can we use plasma hyperosmolality as a predictor of mortality for ST-segment elevation myocardial infarction? Coron Artery Dis 28(1):70–76
Roussel R, Matallah N, Bouby N, El Boustany R, Potier L, Fumeron F et al (2015) Plasma copeptin and decline in renal function in a cohort from the community: the prospective D.E.S.I.R. study. Am J Nephrol 42(2):107–114
Tasevska I, Enhorning S, Christensson A, Persson M, Nilsson PM, Melander O (2016) Increased levels of copeptin, a surrogate marker of arginine vasopressin, are associated with an increased risk of chronic kidney disease in a general population. Am J Nephrol. 44(1):22–28
El Boustany R, Tasevska I, Meijer E, Kieneker LM, Enhorning S, Lefevre G et al (2018) Plasma copeptin and chronic kidney disease risk in 3 European cohorts from the general population. JCI Insight 3:13
Nijssen EC, Rennenberg RJ, Nelemans PJ, Essers BA, Janssen MM, Vermeeren MA et al (2017) Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): a prospective, randomised, phase 3, controlled, open-label, non-inferiority trial. Lancet 389(10076):1312–1322
Kanbay M, Solak Y, Afsar B, Nistor I, Aslan G, Caglayan OH et al (2017) Serum uric acid and risk for acute kidney injury following contrast. Angiology 68(2):132–144
McCullough PA (2008) Contrast-induced acute kidney injury. J Am Coll Cardiol. 51(15):1419–1428
Roncal-Jimenez CA, Milagres T, Andres-Hernando A, Kuwabara M, Jensen T, Song Z et al (2017) Effects of exogenous desmopressin on a model of heat stress nephropathy in mice. Am J Physiol Renal Physiol. 312(3):F418–F426
Yancey PH, Clark ME, Hand SC, Bowlus RD, Somero GN (1982) Living with water stress: evolution of osmolyte systems. Science 217(4566):1214–1222
Seeliger E, Lenhard DC, Persson PB (2014) Contrast media viscosity versus osmolality in kidney injury: lessons from animal studies. Biomed Res Int 2014:15
Stolker JM, McCullough PA, Rao S, Inzucchi SE, Spertus JA, Maddox TM et al (2010) Pre-procedural glucose levels and the risk for contrast-induced acute kidney injury in patients undergoing coronary angiography. J Am Coll Cardiol. 55(14):1433–1440
Trivedi HS, Moore H, Nasr S, Aggarwal K, Agrawal A, Goel P et al (2003) A randomized prospective trial to assess the role of saline hydration on the development of contrast nephrotoxicity. Nephron Clin Pract 93(1):C29–34
Jurado-Roman A, Hernandez-Hernandez F, Garcia-Tejada J, Granda-Nistal C, Molina J, Velazquez M et al (2015) Role of hydration in contrast-induced nephropathy in patients who underwent primary percutaneous coronary intervention. Am J Cardiol 115(9):1174–1178
Luo Y, Wang X, Ye Z, Lai Y, Yao Y, Li J et al (2014) Remedial hydration reduces the incidence of contrast-induced nephropathy and short-term adverse events in patients with ST-segment elevation myocardial infarction: a single-center, randomized trial. Intern Med 53(20):2265–2272
Brar SS, Aharonian V, Mansukhani P, Moore N, Shen AY, Jorgensen M et al (2014) Haemodynamic-guided fluid administration for the prevention of contrast-induced acute kidney injury: the POSEIDON randomised controlled trial. Lancet 383(9931):1814–1823
Hoffman RS, Smilkstein MJ, Howland MA, Goldfrank LR (1993) Osmol gaps revisited: normal values and limitations. J Toxicol Clin Toxicol. 31(1):81–93
Acknowledgements
MK gratefully acknowledges use of the services and facilities of the Koc University Research Center for Translational Medicine (KUTTAM), funded by the Presidency of Turkey, Presidency of Strategy and Budget. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Presidency of Strategy and Budget.
Funding
This study was not funded by any grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanbay, M., Siriopol, D., Ozdogan, E. et al. Serum osmolarity as a potential predictor for contrast-induced nephropathy following elective coronary angiography. Int Urol Nephrol 52, 541–547 (2020). https://doi.org/10.1007/s11255-020-02391-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02391-4