Abstract
Acute promyelocytic leukemia (APL) stands out as a distinctive form of acute leukemia, exhibiting a higher occurrence of thrombotic events when contrasted with other leukemia subtypes. Since thrombosis is a relatively rare but unfavorable condition with poor prognostic implications, it is crucial to determine the risk factors for thrombotic events in APL(thrombosis in large venous or arterial from onset to differentiation therapy in 30d). We performed a retrospective study involving 950 APL patients between January 2000 and October 2022, from which 123 were excluded by younger than 16 years of age, 95 were excluded by incomplete data, and 6 were excluded by thrombosis related to CVC or PICC. A total of 23 APL patients with thrombosis for inclusion in our analysis were performed a 1:5 ratio matching based on sex (perfect match) and age (within 5 years) to patients without thrombosis. These patients were continuously monitored in the outpatient department over a period of 5 years. We meticulously examined clinical and laboratory data to pinpoint the risk factors related to thrombotic events in APL. Our primary clinical endpoints were all-cause mortality and achieving complete remission, while secondary clinical outcomes included APL relapse. Thrombotic events were observed in 2.4% (23/950) of APL patients. Compared to patients without thrombosis, patients with thrombosis had higher lactate dehydrogenase (LDH) [313 (223, 486) vs. 233 (188, 367) U/L, p = 0.020], higher indirect bilirubin [11.2 (7.4, 18.6) vs.8.3 (6.0, 10.7) umol/L, p = 0.004], higher creatinine [72 (62, 85) vs. 63 (54, 74) umol/L, p = 0.026], higher CD2 expression (65.2 vs. 15.2%, p < 0.001), higher CD15 expression (60.9 vs. 24.3%, p = 0.001), and PML/RARαisoforms (p < 0.001). Multivariate-logistic-regression analysis revealed several factors that were markedly related to thrombosis, including LDH (OR≈1.003, CIs≈1.000–1.006, p = 0.021), indirect bilirubin (OR≈1.084, CIs≈1.000–1.188, p = 0.043), CD2 expression positive (OR≈16.629, CIs≈4.001–62.832, p < 0.001), and CD15 expression positive (OR≈7.747, CIs≈2.005–29.941, p = 0.003). The S-type (OR≈0.012, CIs≈0.000–0.310, p = 0.008) and L-type (OR≈0.033, CIs≈0.002–0.609, p = 0.022) PML/RARα isoforms were negatively associated with thrombosis. Kaplan–Meier curves indicated that the survival rates were remarkably varied between APL patients with and without thrombosis (HR:21.34, p < 0.001). LDH and indirect bilirubin are variables significantly associated with thrombosis in APL, S-type and L-type PML/RARαisoforms exhibit a negative association with thrombotic events. The thrombotic events of APL can predict the subsequent survival of thrombosis. The findings of our study have the potential to facilitate early detection of thrombosis and enhance the prognosis for individuals with APL who develop thrombosis. Further validation of our findings will be essential through future prospective or multicenter studies.
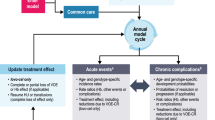
Graphical abstract




Similar content being viewed by others
Data Availability
The datasets presented in this article are not openly available because the data are part of an ongoing study at this centre.
References
Wang ZY, Chen Z (2008) Acute promyelocytic leukemia: from highly fatal to highly curable. Blood 111(5):2505–2515. https://doi.org/10.1182/blood-2007-07-102798
Breccia M, Lo Coco F (2014) Thrombo-hemorrhagic deaths in acute promyelocytic leukemia. Thromb Res 133(Suppl 2):S112-116. https://doi.org/10.1016/S0049-3848(14)50019-9
Breccia M, Avvisati G, Latagliata R, Carmosino I, Guarini A, De Propris MS, Gentilini F, Petti MC, Cimino G, Mandelli F, Lo-Coco F (2007) Occurrence of thrombotic events in acute promyelocytic leukemia correlates with consistent immunophenotypic and molecular features. Leukemia 21(1):79–83. https://doi.org/10.1038/sj.leu.2404377
Chang H, Kuo MC, Shih LY, Wu JH, Lin TL, Dunn P, Tang TC, Hung YS, Wang PN (2013) Acute promyelocytic leukemia-associated thrombosis. Acta Haematol 130(1):1–6. https://doi.org/10.1159/000345833
Rashidi A, Silverberg ML, Conkling PR, Fisher SI (2013) Thrombosis in acute promyelocytic leukemia. Thromb Res 131(4):281–289. https://doi.org/10.1016/j.thromres.2012.11.024
Dally N, Hoffman R, Haddad N, Sarig G, Rowe JM, Brenner B (2005) Predictive factors of bleeding and thrombosis during induction therapy in acute promyelocytic leukemia-a single center experience in 34 patients. Thromb Res 116(2):109–114. https://doi.org/10.1016/j.thromres.2004.11.001
Zhang X, Guo X (2021) Risk factors of thrombosis in chinese subjects with acute promyelocytic leukemia. Thromb J 19(1):42. https://doi.org/10.1186/s12959-021-00294-7
Mitrovic M, Suvajdzic N, Elezovic I, Bogdanovic A, Djordjevic V, Miljic P, Djunic I, Gvozdenov M, Colovic N, Virijevic M, Lekovic D, Vidovic A, Tomin D (2015) Thrombotic events in acute promyelocytic leukemia. Thromb Res 135(4):588–593. https://doi.org/10.1016/j.thromres.2014.11.026
Choudhry A, DeLoughery TG (2012) Bleeding and thrombosis in acute promyelocytic leukemia. Am J Hematol 87(6):596–603. https://doi.org/10.1002/ajh.23158
Gando S, Levi M, Toh CH (2016) Disseminated intravascular coagulation. Nat Rev Dis Primers 2:16037. https://doi.org/10.1038/nrdp.2016.37
Sanz MA, Montesinos P (2020) Advances in the management of coagulopathy in acute promyelocytic leukemia. Thromb Res 191(Suppl 1):S63–S67. https://doi.org/10.1016/S0049-3848(20)30399-6
Chen L, Zhu HM, Li Y, Liu QF, Hu Y, Zhou JF, Jin J, Hu JD, Liu T, Wu DP, Chen JP, Lai YR, Wang JX, Li J, Li JY, Du X, Wang X, Yang MZ, Yan JS, Ouyang GF, Liu L, Hou M, Huang XJ, Yan XJ, Xu D, Li WM, Li DJ, Lou YJ, Wu ZJ, Niu T, Wang Y, Li XY, You JH, Zhao HJ, Chen Y, Shen Y, Chen QS, Chen Y, Li J, Wang BS, Zhao WL, Mi JQ, Wang KK, Hu J, Chen Z, Chen SJ, Li JM (2021) Arsenic trioxide replacing or reducing chemotherapy in consolidation therapy for acute promyelocytic leukemia (apl2012 trial). Proc Natl Acad Sci U S A 118(6):e2020382118. https://doi.org/10.1073/pnas.2020382118
Song YH, Qiao C, Xiao LC, Zhang R, Lu H (2018) Hyperfibrinolysis is an important cause of early hemorrhage in patients with acute promyelocytic leukemia. Med Sci Monit 24:3249–3255. https://doi.org/10.12659/MSM.909938
Rees D, Grimwade D, Langabeer S, Burnett A, Goldstone A (1997) Influence of genetic predisposition to thrombosis on natural history of acute promyelocytic leukaemia. MRC adult leukaemia working party. Br J Haematol 96(3):490–492. https://doi.org/10.1046/j.1365-2141.1997.d01-2063.x
Dawson DM, Goodfriend TL, Kaplan NO (1964) LACTIC dehydrogenases: functions of the two types rates of synthesis of the two major forms can be correlated with metabolic differentiation. Science 143(3609):929–933. https://doi.org/10.1126/science.143.3609.929
Butt AA, Michaels S, Kissinger P (2002) The association of serum lactate dehydrogenase level with selected opportunistic infections and HIV progression. Int J Infect Dis 6(3):178–181. https://doi.org/10.1016/s1201-9712(02)90107-4
Shah P, Mehta VM, Cowger JA, Aaronson KD, Pagani FD (2014) Diagnosis of hemolysis and device thrombosis with lactate dehydrogenase during left ventricular assist device support. J Heart Lung Transplant 33(1):102–104. https://doi.org/10.1016/j.healun.2013.07.013
Pelicano H, Martin DS, Xu RH, Huang P (2006) Glycolysis inhibition for anticancer treatment. Oncogene 25(34):4633–4646. https://doi.org/10.1038/sj.onc.1209597
Ding J, Karp JE, Emadi A (2017) Elevated lactate dehydrogenase (ldh) can be a marker of immune suppression in cancer: interplay between hematologic and solid neoplastic clones and their microenvironments. Cancer Biomark 19(4):353–363. https://doi.org/10.3233/CBM-160336
García R, Hernández JM, Caballero MD, González M, Galende J, del Cañizo MC, Vázquez L, San Miguel JF (1993) Serum lactate dehydrogenase level as a prognostic factor in hodgkin’s disease. Br J Cancer 68(6):1227–1231. https://doi.org/10.1038/bjc.1993.509
De Stefano V, Sorà F, Rossi E, Chiusolo P, Laurenti L, Fianchi L, Zini G, Pagano L, Sica S, Leone G (2005) The risk of thrombosis in patients with acute leukemia: occurrence of thrombosis at diagnosis and during treatment. J Thromb Haemost 3(9):1985–1992. https://doi.org/10.1111/j.1538-7836.2005.01467.x
Kim DY, Lee JH, Lee JH, Kim SD, Lim SN, Choi Y, Lee YS, Kang YA, Seol M, Jeon M, Kim JY, Lee KH, Lee YJ, Lee KH (2011) Significance of fibrinogen, d-dimer, and LDH levels in predicting the risk of bleeding in patients with acute promyelocytic leukemia. Leuk Res 35(2):152–158. https://doi.org/10.1016/j.leukres.2010.05.022
Fattizzo B, Bortolotti M, Giannotta JA, Zaninoni A, Consonni D, Barcellini W (2022) Intravascular hemolysis and multitreatment predict thrombosis in patients with autoimmune hemolytic anemia. J Thromb Haemost 20(8):1852–1858. https://doi.org/10.1111/jth.15757
Ferraris AM, Giuntini P, Gaetani GF (1979) Serum lactic dehydrogenase as a prognostic tool for non-hodgkin lymphomas. Blood 54(4):928–932
Nadir Y (2015) Hemorrhage and thrombosis in acute promyelocytic leukemia: can we currently predict these manifestations. Thromb Res 135(4):573–574. https://doi.org/10.1016/j.thromres.2015.01.035
Cunha De Santis G, Tamarozzi MB, Sousa RB, Moreno SE, Secco D, Garcia AB, Lima AS, Faccioli LH, Falcão RP, Cunha FQ, Rego EM (2007) Adhesion molecules and differentiation syndrome: phenotypic and functional analysis of the effect of atra, as2o3, phenylbutyrate, and g-CSF in acute promyelocytic leukemia. Haematologica 92(12):1615–1622. https://doi.org/10.3324/haematol.10607
Funding
This work was supported by Peking University People's Hospital Research and Development Funds (RDJ2022-18) and the National Natural Science Foundation of China (grant no. 82270227 & 82070189).
Author information
Authors and Affiliations
Contributions
XS, CC, Ws and YL collectively formulated the study's overarching concept and design. WG, XS, and CC participated in acquiring the data. XS and CC conducted data analysis and interpretation. The initial manuscript draft was prepared by XS and CC. JZ and YW contributed their statistical expertise. All authors collaborated on substantial revisions of the article and contributed intellectually to its content.
Corresponding authors
Ethics declarations
Ethics
We received ethical approval from the same hospital (2023PHB178-001). Our research strictly adhered to the principles outlined in the Declaration of Helsinki. The funding entity had no influence over the study's implementation. Both patients and hospital personnel were not participants in or aware of the research. Due to our data sharing agreement and the approval of the research ethics board, we are unable to share the original data.
Conflict of interest
All authors are obligated to reveal any potential conflicts of interest, including commercial, financial, or other affiliations pertaining to the subject matter of this article. The authors have declared the absence of any such associations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• First study to explore the prognostic outcomes of acute promyelocytic leukemia patients with thrombotic events.
• APL patients with thrombosis had an elevated mortality rate, while there was no significant difference in relapse rates.
• Lactate dehydrogenase and indirect bilirubin may be risk factors for thrombotic events in APL patients, and hemolysis may be related to the formation of thrombosis in APL.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, X., Chi, C., Gao, W. et al. Biochemical risk factors and outcomes of acute promyelocytic leukemia patients with thrombotic events: a matched pair analysis. J Thromb Thrombolysis (2024). https://doi.org/10.1007/s11239-024-02988-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11239-024-02988-x