Abstract
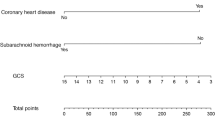
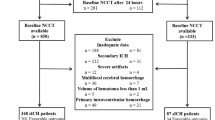
Cerebral white matter lesions (WMLs) increase the risk of bleeding after intravenous thrombolysis (IVT) but are also considered to require IVT. Its risk factors and predictive models are still poorly studied. The aim of this study is to develop a clinically applicable model for post-IVT haemorrhage. It offers the possibility to prevent symptomatic intracranial hemorrhage (sICH) in patients with IVT in severe WMLs. A large single-center observational study conducted a retrospective analysis of IVT in patients with severe WMLs from January 2018 to December 2022. Univariate and multi-factor logistic regression results were used to construct nomogram model, and a series of validations were performed on the model. More than 2,000 patients with IVT were screened for inclusion in this study after cranial magnetic resonance imaging evaluation of 180 patients with severe WMLs, 28 of whom developed sICH. In univariate analysis, history of hypertension (OR 3.505 CI 2.257–4.752, p = 0.049), hyperlipidemia (OR 4.622 CI 3.761- 5.483, p < 0.001), the NIHSS score before IVT (OR 41.250 CI 39.212–43.288, p < 0.001), low-density lipoprotein levels (OR 1.995 CI 1.448–2.543, p = 0.013), cholesterol levels (OR 1.668 CI 1.246–2.090, p = 0.017), platelet count (OR 0.992 CI 0.985–0.999, p = 0.028), systolic blood pressure (OR 1.044 CI 1.022–1.066, p < 0.001), diastolic blood pressure (OR 1.047 CI 1.024–1.070, p < 0.001) were significantly associated with sICH. In a multifactorial analysis, the NIHSS score before IVT (OR 94.743 CI 92.311–97.175, p < 0.001), and diastolic blood pressure (OR 1.051 CI 1.005–1.097, p = 0.033) were considered to be significantly associated with sICH after IVT as risk factors for the occurrence of sICH. The four most significant factors from logistic regression are subsequently fitted to create a predictive model. The accuracy was verified using ROC curves, calibration curves, decision curves, and clinical impact curves, and the model was considered to have high accuracy (AUC 0.932, 95% 0.888–0.976). The NHISS score before IVT and diastolic blood pressure are independent risk factors for sICH after IVT in patients with severe WMLs. The models based on hyperlipidemia, the NIHSS score before IVT, low-density lipoprotein and diastolic blood pressure are highly accurate and can be applied clinically to provide a reliable predictive basis for IVT in patients with severe WMLs.





Similar content being viewed by others
Availability of data and material
All relevant data are described within the paper. Deidentified data can be requested. Data can be requested by all interested researchers, who can be contacted via the corresponding author.
References
Sahuc-Rodrigues P, Sagui E, Wybrecht D et al (2018) Intravenous thrombolytic therapy for acute anterior ischemic stroke: experience at the French Military Teaching Hospital in Toulon from 2003 to 2014. Rev Neurol (Paris) 174(3):125–136
Ji B, Zhou F, Han L et al (2017) Sodium tanshinone IIA sulfonate enhances effectiveness Rt-PA treatment in acute ischemic stroke patients associated with ameliorating blood-brain barrier damage. Transl Stroke Res 8(4):334–340
Jauch EC, Saver JL, Adams HP Jr et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44(3):870–947
Berge E, Whiteley W, Audebert H, et al (2021) European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J 6(1):I–lxii
Tanne D, Kasner SE, Demchuk AM et al (2002) Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: the Multicenter rt-PA Stroke Survey. Circulation 105(14):1679–1685
Neumann-Haefelin T, Hoelig S, Berkefeld J et al (2006) Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke. Stroke 37(10):2463–2466
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9(7):689–701
Lin Q, Li Z, Wei R, Lei Q, Liu Y, Cai X (2016) Increased risk of post-thrombolysis intracranial hemorrhage in acute ischemic stroke patients with leukoaraiosis: a meta-analysis. PLoS ONE 11(4):e0153486
Wardlaw JM, Smith C, Dichgans M (2013) Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol 12(5):483–497
Curtze S, Haapaniemi E, Melkas S et al (2015) White matter lesions double the risk of post-thrombolytic intracerebral hemorrhage. Stroke 46(8):2149–2155
Ariës MJ, Uyttenboogaart M, Vroomen PC, De Keyser J, Luijckx GJ (2010) tPA treatment for acute ischaemic stroke in patients with leukoaraiosis. Eur J Neurol 17(6):866–870
Liu L, Chen W, Zhou H et al (2020) Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol 5(2):159–176
Miyamoto S, Ogasawara K, Kuroda S et al (2022) Japan Stroke Society Guideline 2021 for the treatment of stroke. Int J Stroke 17(9):1039–1049
Shen Y, Li D, Tang B, Cao Q, Hou Z, Xu L (2022) Factors associated with symptomatic intracranial haemorrhage after intravenous thrombolysis in severe white matter lesions: a retrospective analysis. Postgrad Med J 98(1165):842–847
Liu L, Ding J, Leng X et al (2018) Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol 3(3):117–130
Strbian D, Engelter S, Michel P et al (2012) Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol 71(5):634–641
Hacke W, Kaste M, Fieschi C et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 352(9136):1245–1251
van Straaten EC, Fazekas F, Rostrup E et al (2006) Impact of white matter hyperintensities scoring method on correlations with clinical data: the LADIS study. Stroke 37(3):836–840
Shen Y, Li D, Hu M et al (2022) Retinal nerve fiber layer thickness and visual aura mechanism in patients with vestibular migraine with or without white matter lesions. Neurology Asia 27(3):709–716
Kapeller P, Barber R, Vermeulen RJ et al (2003) Visual rating of age-related white matter changes on magnetic resonance imaging: scale comparison, interrater agreement, and correlations with quantitative measurements. Stroke 34(2):441–445
Riley RD, Ensor J, Snell KIE et al (2020) Calculating the sample size required for developing a clinical prediction model. BMJ 368:m441
Guy S, Sermon-Cadd AM, Shepherd FM, Kitchen S, Bowyer AE (2019) A cost-effective approach to factor assay calibration using a truncated live calibration curve. Int J Lab Hematol 41(5):679–683
Park SH, Goo JM, Jo CH (2004) Receiver operating characteristic (ROC) curve: practical review for radiologists. Korean J Radiol 5(1):11–18
Tissue plasminogen activator for acute ischemic stroke (1995) N Engl J Med 333(24):1581–1587
Shobha N, Buchan AM, Hill MD (2011) Thrombolysis at 3–4.5 hours after acute ischemic stroke onset—evidence from the Canadian Alteplase for Stroke Effectiveness Study (CASES) registry. Cerebrovasc Dis 31(3):223–228
Kurre W, Berkefeld J, Brassel F et al (2010) In-hospital complication rates after stent treatment of 388 symptomatic intracranial stenoses: results from the INTRASTENT multicentric registry. Stroke 41(3):494–498
Hao Y, Liu W, Wang H et al (2019) Prognosis of asymptomatic intracranial hemorrhage after endovascular treatment. J Neurointerv Surg 11(2):123–126
Ho BL, Chen CF, Lin RT, Liu CK, Chao AC (2016) Clinical implication of hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator. Neurol Sci 37(11):1799–1805
Lokeskrawee T, Muengtaweepongsa S, Patumanond J et al (2017) Prediction of symptomatic intracranial hemorrhage after intravenous thrombolysis in acute ischemic stroke: the Symptomatic Intracranial Hemorrhage Score. J Stroke Cerebrovasc Dis 26(11):2622–2629
Xu X, Li C, Wan T et al (2017) Risk factors for hemorrhagic transformation after intravenous thrombolysis in acute cerebral infarction: a retrospective single-center study. World Neurosurg 101:155–160
Grueter BE, Schulz UG (2012) Age-related cerebral white matter disease (leukoaraiosis): a review. Postgrad Med J 88(1036):79–87
Simão F, Ustunkaya T, Clermont AC, Feener EP (2017) Plasma kallikrein mediates brain hemorrhage and edema caused by tissue plasminogen activator therapy in mice after stroke. Blood 129(16):2280–2290
Dobrivojević M, Špiranec K, Sinđić A (2015) Involvement of bradykinin in brain edema development after ischemic stroke. Pflugers Arch 467(2):201–212
Lu BY, Thanawala SU, Zochowski KC, Burke MJ, Carroll WL, Bhatla T (2016) Decitabine enhances chemosensitivity of early T-cell precursor-acute lymphoblastic leukemia cell lines and patient-derived samples. Leuk Lymphoma 57(8):1938–1941
Yang N, Lin M, Wang BG et al (2016) Low level of low-density lipoprotein cholesterol is related with increased hemorrhagic transformation after acute ischemic cerebral infarction. Eur Rev Med Pharmacol Sci 20(4):673–678
Saito I, Yamagishi K, Kokubo Y et al (2017) Association of high-density lipoprotein cholesterol concentration with different types of stroke and coronary heart disease: the Japan Public Health Center-based prospective (JPHC) study. Atherosclerosis 265:147–154
Funding
The work was supported by the National Natural Science Foundation of China (No.81460199, 82160252 and 82271439), Natural Science Foundation of Jiangxi province (20202BAB206029 and 20224ACB206015), Science and technology project of Jiangxi Health Commission (202110028), and Double thousand talents program of Jiangxi province (jxsq2019101021).
Author information
Authors and Affiliations
Contributions
YS and DH designed this study and wrote the initial draft of this paper. YS, YX and QC contributed to the analysis and interpretation of data and assisted in the preparation of this paper. YS, QC, WX, BT, YX, LW, YY and NQ contributed to data collection and interpretation of this paper. All of the authors approved the final version of this paper and agree to be accountable for all aspects of this paper. DH is the guarantor.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have declared no conflicts of interest.
Ethics approval
The research was approved by ethics committee of the second affiliated hospital of Nanchang University (No. [2016] 096).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, Y., Xiong, Y., Cao, Q. et al. Construction and validation of a nomogram model to predict symptomatic intracranial hemorrhage after intravenous thrombolysis in severe white matter lesions. J Thromb Thrombolysis 56, 111–120 (2023). https://doi.org/10.1007/s11239-023-02828-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02828-4