Abstract
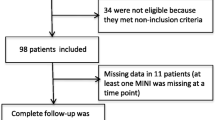
Depression is associated with heart failure independent of traditional cardiovascular disease risk factors. Enhanced platelet activation has been suggested as a potential mechanism and has been associated with negative inotropic effects that can affect left ventricular ejection fraction (LVEF). We examined 131 consecutive acute coronary syndrome (ACS) patients to assess whether depression increased the risk for developing LV dysfunction, and to determine the effects of platelet serotonin signaling in this relationship. Major depression was assessed using the Structured Clinical Interview and depressive symptoms were measured using the Beck Depression Inventory (BDI), with BDI ≥ 10 defined as abnormal. LV dysfunction was defined as LVEF ≤ 45%. Platelet serotonin response was measured by serotonin augmented platelet aggregation and platelet serotonin receptor density. Mean age of ACS participants was 59 years, 78.6% male and 74.0% Caucasian. 34.4% of patients had a reduced LVEF ≤ 45% on presentation. Almost half (47.0%) of patients had BDI ≥ 10 and 18.0% had major depressive disorder. Platelet serotonin response was found to be augmented in depressed patients with low LVEF compared to depressed patients with normal LVEF (p < 0.020). However, the presence of LV dysfunction was found to be similar in both depressed (32.3%) and non-depressed (36.2%) patients (p = 0.714). This suggests alternative factors contribute to poor cardiovascular outcomes in depressed patients that are independent of LV function in post ACS patients.

Similar content being viewed by others
Availability of data and material
Raw data available on open science framework https://osf.io/hyj69/?view_only=35a1d31edd8740309b24ae5d96502e7e.
Abbreviations
- ACS:
-
Acute coronary syndrome
- LVEF:
-
Left ventricular ejection fraction
- MDD:
-
Major depressive disorder
- BDI:
-
Beck Depression Inventory
- SCID:
-
Structured clinical inventory for depression
- IQR:
-
Interquartile range
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
References
Carney RM, Blumenthal JA, Catellier D et al (2003) Depression as a risk factor for mortality after acute myocardial infarction. Am J Cardiol 92(11):1277–1281
Carney RM, Rich MW, Freedland KE et al (1988) Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med 50:627–733
Frasure-Smith N, Lespérance F, Juneau M, Talajic M, Bourassa MG (1999) Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med 61(1):26–37
Musselman DL, Evans DL, Nemeroff CB (2003) The relationship of depression to cardiovascular disease. Arch Gen Psychiatry 55:580–592
Frasure-Smith N, Lespérance F, Talajic M (1995) Depression and 18-month prognosis after myocardial infarction. Circulation 91:99–1005
Ziegelstein RC (2001) Depression after myocardial infarction. Cardiol Rev 9(1):45–51
Carney RM, Freedland KE (2008) Depression in patients with coronary heart disease. Am J Med 121(11):S20–S27
Thombs BD, De Jonge P, Coyne JC et al (2008) Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA 300:2161–2171
Lespérance F, Frasure-Smith N, Juneau M, Théroux P (2000) Depression and 1-year prognosis in unstable angina. Arch Intern Med 160:1354–1360
Shimbo D, Child J, Davidson K et al (2002) Exaggerated serotonin-mediated platelet reactivity as a possible link in depression and acute coronary syndromes. Am J Cardiol 89(3):331–333
Morel-Kopp M, Mclean L, Chen Q et al (2009) The association of depression with platelet activation: evidence for a treatment effect. J Thromb Haemost 7(4):573–581
Musselman DL, Tomer A, Manatunga AK et al (1996) Exaggerated platelet reactivity in major depression. Am J Psychiatry 153(10):1313–1317
Ziegelstein RC, Parakh K, Sakhuja A, Bhat U (2009) Platelet function in patients with major depression. Intern Med J 39(1):38–43
Zafar MU, Paz-Yepes M, Shimbo D et al (2010) Anxiety is a better predictor of platelet reactivity in coronary artery disease patients than depression. Eur Heart J 31:1573–1582
Williams MS, Ziegelstein RC, McCann UD, Gould NF, Ashvetiya T, Vaidya D (2019) Platelet serotonin signaling in patients with cardiovascular disease and comorbid depression. Psychosom Med 81:352–362
Fujita S, Takeda Y, Kizawa S et al (2015) Platelet volume indices are associated with systolic and diastolic cardiac dysfunction, and left ventricular hypertrophy. BMC Cardiovasc Disord 15:52
Yazici HU, Poyraz F, Sen N et al (2011) Relationship between mean platelet volume and left ventricular systolic function in patients with metabolic syndrome and ST-elevation myocardial infarction. Clin Investig Med 34:E330
Jiang W, Boyle SH, Ortel TL et al (2015) Platelet aggregation and mental stress induced myocardial ischemia: results from the Responses of Myocardial Ischemia to Escitalopram Treatment (REMIT) study. Am Heart J 169:496–507
Angaran P, Dorian P, Ha ACT et al (2020) Association of left ventricular ejection fraction with mortality and hospitalizations. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2019.12.016
Miller AL, Dib C, Li L et al (2012) Left ventricular ejection fraction assessment among patients with acute myocardial infarction and its association with hospital quality of care and evidence-based therapy use. Circ Cardiovasc Qual Outcomes 5:662–667
Parodi G, Antoniucci D (2010) Left ventricular remodeling after primary percutaneous coronary intervention. Am Heart J 160:S11–S15
Mendis S, Thygesen K, Kuulasmaa K et al (2011) World Health Organization definition of myocardial infarction: 2008-09 revision. Int J Epidemiol 40:139–146
Yancy CW, Jessup M, Bozkurt B et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American college of cardiology foundation/American Heart Association task force on practice guidelines. Circulation 128:1810–1852
Hsu JJ, Ziaeian B, Fonarow GC (2017) Heart failure with mid-range (borderline) ejection fraction. JACC Heart Fail 5:763–771
First MB, Spitzer RL, Gibbon M, Williams JBW (2002) Structured clinical interview for DSM-IV axis I disorders, research version, patient edition (SCID-I/P). Biometrics Research, New York State Psychiatric Institude, New York
Beck AT, Steer RA, Brown GK (1996) Manual for the Beck Depression Inventory-II. TX Psychol Corp, San Antonio
Arranz B, Rosel P, Sarró S et al (2003) Altered platelet serotonin 5-HT2A receptor density but not second messenger inositol trisphosphate levels in drug-free schizophrenic patients. Psychiatry Res 118:165–174
Lv J, Liu F (2017) The role of serotonin beyond the central nervous system during embryogenesis. Front Cell Neurosci 11:74
Ayme-Dietrich E, Aubertin-Kirch G, Maroteaux L, Monassier L (2017) Cardiovascular remodeling and the peripheral serotonergic system. Arch Cardiovasc Dis 110(1):51–59
Williams MS (2012) Platelets and depression in cardiovascular disease: a brief review of the current literature. World J Psychiatry 2:114–123
Mendelson SD (2000) The current status of the platelet 5-HT(2A) receptor in depression. J Affect Disord 57:13–24
Hrdina PD, Bakish D, Chudzik J, Ravindran A, Lapierre YD (1995) Serotonergic markers in platelets of patients with major depression: upregulation of 5-HT2 receptors. J Psychiatry Neurosci 20:11–19
Sheline YI, Bardgett ME, Jackson JL, Newcomer JW, Csernansky JG (1995) Platelet serotonin markers and depressive symptomatology. Biol Psychiatry 37:442–447
Rao ML, Hawellek B, Papassotiropoulos A, Deister A, Frahnert C (1998) Upregulation of the platelet serotonin(2A) receptor and low blood serotonin in suicidal psychiatric patients. Neuropsychobiology 38:84–89
Berger JS, Becker RC, Kuhn C, Helms MJ, Ortel TL, Williams R (2013) Hyperreactive platelet phenotypes: relationship to altered serotonin transporter number, transport kinetics and intrinsic response to adrenergic co-stimulation. Thromb Haemost 109:85
Lett H, Ali S, Whooley M (2008) Depression and cardiac function in patients with stable coronary heart disease: findings from the heart and soul study. Psychosom Med 70:444–449
Spijkerman TA, Van Den Brink RHS, Jansen JHC, Crijns HJGM, Ormel J (2005) Who is at risk of post-MI depressive symptoms? J Psychosom Res 58(5):425–432
Lespérance F, Frasure-Smith N, Talajic M (1996) Major depression before and after myocardial infarction: its nature and consequences. Psychosom Med 58(2):99–110
Strik JJMH, Lousberg R, Cheriex EC, Honig A (2004) One year cumulative incidence of depression following myocardial infarction and impact on cardiac outcome. J Psychosom Res 56:59–66
Bush DE, Ziegelstein RC, Tayback M et al (2001) Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 88:337–341
Kim Y-H, Kim SH, Lim SY et al (2012) Relationship between depression and subclinical left ventricular changes in the general population. Heart 98(18):1378–1383
Carney RM, Freedland KE, Veith RC (2005) Depression, the autonomic nervous system, and coronary heart disease. Psychosom Med 67(SUPPL. 1):S29–S33
Kent LK, Shapiro PA (2009) Depression and related psychological factors in heart disease. Harv Rev Psychiatry 17(6):377–388
Denollet J, de Jonge P, Kuyper A et al (2009) Depression and type D personality represent different forms of distress in the Myocardial INfarction and Depression—Intervention Trial (MIND-IT). Psychol Med 39(05):749–756
Welin C, Lappas G, Wilhelmsen L (2000) Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med 247:629–639
Funding
MW was funded by Grant RO1 HL096694 from the United States National Heart, Lung, and Blood Institute (Bethesda, MD). D.V. was supported by the Johns Hopkins Biostatistics, Epidemiology and Data Management Core.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of the manuscript significantly and are in agreement with the content. Material preparation and data collection were performed by MW and JS. DV performed statistical analysis. The first draft of manuscript written by JS and all authors commented on previous versions of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MW serves on the speaker’s bureau of Maryland State Medical Society and Rockpointe Corporation that is supported by an unrestricted educational grant from AstraZeneca. The other authors report no conflicts of interest.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethics approval
This study was approved by the Johns Hopkins institutional review board
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sama, J., Vaidya, D., Mukherjee, M. et al. Effects of clinical depression on left ventricular dysfunction in patients with acute coronary syndrome. J Thromb Thrombolysis 51, 693–700 (2021). https://doi.org/10.1007/s11239-020-02268-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02268-4