Abstract
Purpose
Epilepsy is a global public health problem that causes a profound physical, psychological and social consequences. However, as such evidence in our country is limited, this study aimed to assess the health-related quality of life (HRQOL) and associated factors among patients with epilepsy.
Methods
An institution-based cross-sectional study was conducted on 370 patients with epilepsy. The Quality of Life in Epilepsy Inventory-31 (QOLIE-31) was used to measure HRQOL. Multiple linear regression was fitted to assess the association between HRQOL and the independent variables, and a P-value < 0.05 and a 95% confidence interval were used to declare statistical significance.
Results
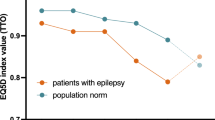
More than 55% of the participants were male, and the mean age of the participants was 29.64 (11.09) years. The overall HRQOL score was 55.81 (14.00). The scale scores ranged from 46.50 (15.55) to 64.98 (19.43). Out of the seven scales, the energy scale score was the lowest. Frequency of seizure, anxiety, depression, perceived stigma and adverse drug event were negatively associated with HRQOL, whereas social support had a significant positive association.
Conclusion
This study revealed that the HRQOL of patients was low and that its energy and emotional scales were the most affected. The presence of depression, anxiety and stigma adversely affected patient HRQOL. Therefore, healthcare professionals should be aware of the emotional state of the role it plays for HRQOL. Interventions aimed at reducing psychosocial problems and stigmatization are also needed to improve the patient HRQOL.
Similar content being viewed by others
Data Availability
The datasets supporting the conclusions of this article are available upon request to the corresponding author. Due to data protection restrictions and participant confidentiality, we do not make participants' data publicly available.
References
World Health Organization (2018). Epilepsy. https://www.who.int/news-room/fact-sheets/detail/epilepsy.
Paul, A., Adeloye, D., George-Carey, R., Kolčić, I., Grant, L., & Chan, K. Y. (2012). An estimate of the prevalence of epilepsy in Sub-Saharan Africa: A systematic analysis. Journal of Global Health, 2(2), 1–13. https://doi.org/10.7189/jogh.02.020405.
Worku, D. (2013). Review article: Epilepsy in Ethiopia (Vol. 333).
Kerr, M. P. (2012). The impact of epilepsy on patients' lives. Acta Neurologica Scandinavica, 126(S194), 1–9. https://doi.org/10.1111/ane.12014.
Kinyanjui, D. W. C., Kathuku, D. M., & Mburu, J. M. (2013). Quality of life among patients living with epilepsy attending the neurology clinic at kenyatta national hospital, Nairobi, Kenya: a comparative study. Health Qual Life Outcomes, 11(1), 98. https://doi.org/10.1186/1477-7525-11-98.
Mrabet, H., Mrabet, A., Zouari, B., & Ghachem, R. (2004). Health-related quality of life of people with epilepsy compared with a general reference population: a Tunisian study. Epilepsia, 45(7), 838–843.
Perucca, P., Gilliam, F. G., & Schmitz, B. (2009). Epilepsy treatment as a predeterminant of psychosocial ill health. Epilepsy & Behavior, 15(2), S46–S50.
Gurshaw, M., Agalu, A., & Chanie, T. (2014). Anti-epileptic drug utilization and treatment outcome among epileptic patients on follow-up in a resource poor setting. Journal of Young Pharmacists, 6(3), 47.
Ayalew, M. B., & Muche, E. A. (2018). Patient reported adverse events among epileptic patients taking antiepileptic drugs. SAGE Open Med, 6, 2050312118772471.
Calman Kc, E. (2019). Quality of life and health related quality of life – is there a difference?. Evidence Based Nursing 2014–2014.
Karimi, M., & Brazier, J. (2016). Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics, 34(7), 645–649.
Baskind, R., & Birbeck, G. L. (2005). Epilepsy-associated stigma in sub-Saharan Africa: the social landscape of a disease. Epilepsy & Behavior, 7(1), 68–73.
Baker, G. A. (2002). The psychosocial burden of epilepsy. Epilepsia, 43(6), 26–30. https://doi.org/10.1046/j.1528-1157.43.s.6.12.x.
Choi-Kwon, S., Chung, C., Kim, H., Lee, S., Yoon, S., Kho, H., et al. (2003). Factors affecting the quality of life in patients with epilepsy in Seoul South Korea. Acta Neurologica Scandinavica, 108(6), 428–434. https://doi.org/10.1046/j.1600-0404.2003.00151.x.
Endermann, M., & Zimmermann, F. (2009). Factors associated with health-related quality of life, anxiety and depression among young adults with epilepsy and mild cognitive impairments in short-term residential care. Seizure, 18(3), 167–175.
Tegegne, M. T., et al. (2014). Assessment of quality of life and associated factors among people with epilepsy attending at Amanuel Mental. Science Journal of Public Health, 2(5), 378–383.
Lee, S. J., Kim, J. E., Seo, J. G., Won, Y., Lee, J. J., Moon, H. J., et al. (2014). Predictors of quality of life and their interrelations in Korean people with epilepsy A MEPSY study. Seizure European Journal of Epilepsy, 23(9), 762–768.
Meldolesi, G. N., Picardi, A., Quarato, P. P., Grammaldo, L. G., Esposito, V., Mascia, A., et al. (2006). Factors associated with generic and disease-specific quality of life in temporal lobe epilepsy. Epilepsy research, 69(2), 135–146. https://doi.org/10.1016/j.eplepsyres.2006.01.010.
Melikyan, E., & Guekht, A. (2012). Health-related quality of life in Russian adults with epilepsy: The effect of socio-demographic and clinical factors. Epilepsy and Behavior, 25(4), 670–625.
Chen, H.-F., Tsai, Y.-F., Hsi, M.-S., & Chen, J.-C. (2016). Factors affecting quality of life in adults with epilepsy in Taiwan: a cross-sectional, correlational study. Epilepsy & Behavior, 58, 26–32.
Ayenalem, A. E., Tiruye, T. Y., & Muhammed, M. S. (2017). Impact of Self Stigma on Quality of Life of People with Mental Illness at Dilla University Referral Hospital, South Ethiopia. American Journal of Health Research, 5(5), 125–130.
Yue, L., Yu, P., et al. (2011). Determinants of quality of life in people with epilepsy and their gender differences. Epilepsy and Behavior, 22(4), 692–696. https://doi.org/10.1016/j.yebeh.2011.08.022.
George, J., Kulkarni, C., Epilepsy, C. C., & Sarma, G. R. K. (2015). Antiepileptic drugs and quality of life in patients with epilepsy : a tertiary care hospital-based study. Value in Health Regional Issues, 6, 1–6.
Nabukenya, A. M., Matovu, J. K. B., Wabwire-Mangen, F., Wanyenze, R. K., & Makumbi, F. (2014). Health-related quality of life in epilepsy patients receiving anti-epileptic drugs at National Referral Hospitals in Uganda: A cross-sectional study. Health Qual Life Outcomes, 12(1), 1–8. https://doi.org/10.1186/1477-7525-12-49.
Canuet, L., Ishii, R., Iwase, M., Ikezawa, K., Kurimoto, R., Azechi, M., et al. (2009). Factors associated with impaired quality of life in younger and older adults with epilepsy. Epilepsy research, 83(1), 58–65.
Djibuti, M., & Shakarishvili, R. (2003). Influence of clinical, demographic, and socioeconomic variables on quality of life in patients with epilepsy: findings from Georgian study. Journal of Neurology, Neurosurgery & Psychiatry, 74(5), 570–573.
Alanis-Guevara, I., Peña, E., Corona, T., López-Ayala, T., López-Meza, E., & López-Gómez, M. (2005). Sleep disturbances, socioeconomic status, and seizure control as main predictors of quality of life in epilepsy. Epilepsy and Behavior, 7(3), 481–485. https://doi.org/10.1016/j.yebeh.2005.06.010.
Shetty, P. H., Naik, R. K., Saroja, A., & Punith, K. (2011). Quality of life in patients with epilepsy in India. Journal of Neurosciences in Rural Practice, 2(1), 33–38. https://doi.org/10.4103/0976-3147.80092.
Gebre, A. K. (2018). Sociodemographic, clinical variables, and quality of life in patients with epilepsy in Mekelle City, Northern Ethiopia. Behavioral Neurology, 2018, 1–6.
Shiferaw, D., & Hailu, E. (2015). Quality of Life Assessment among Adult Epileptic Patients Taking Follow Up Care at Jimma University Medical Center, Jimma, South West Ethiopia: Using Quality of Life in Epilepsy Inventory-31instrument. Global Jourenal of Medical Research, 18(3).
RAND HEALTH CARE Quality of Life in Epilepsy Inventory-31 (QOLIE-31) https://www.rand.org/content/dam/rand/www/external/health/surveys_tools/qolie/qolie31_survey.pdf
RAND HEALTH CARE Quality of Life in Epilepsy Inventory-31 (QOLIE-31) Scoring Instructions. https://www.rand.org/content/dam/rand/www/external/health/surveys_tools/qolie/qolie31_scoring.pdf
Dalgard, O. S., Dowrick, C., Lehtinen, V., Vazquez-Barquero, J. L., Casey, P., Wilkinson, G., et al. (2006). Negative life events, social support and gender difference in depression. Social Psychiatry and Psychiatric Epidemiology, 41(6), 444–451.
Mbuba, C. K., Abubakar, A., Odermatt, P., Newton, C. R., & Carter, J. A. (2012). Development and validation of the Kilifi Stigma Scale for Epilepsy in Kenya. Epilepsy and Behavior : E&B, 24(1), 81–85. https://doi.org/10.1016/j.yebeh.2012.02.019.
Fanta, T., Azale, T., Assefa, D., & Getachew, M. (2015). Prevalence and factors associated with perceived stigma among patients with epilepsy in Ethiopia. Psychiatry Journal, 2015, 1–7.
Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the Hospital Anxiety and Depression Scale. Journal of Psychosomatic Research. https://doi.org/10.1016/s0022-3999(01)00296-3.
Agency, C. S. (2016). Addis Ababa, Ethiopia, and Rockville (p. 2016). Maryland, USA: CSA and ICF.
Mutluay, F. K., Gunduz, A., Tekeoglu, A., Oguz, S., & Yeni, S. N. (2016). Health related quality of life in patients with epilepsy in Turkey. Journal of Physical Therapy Science, 28(1), 240–245. https://doi.org/10.1589/jpts.28.240.
Steiger, B. K., & Jokeit, H. (2017). Why epilepsy challenges social life. Seizure, 44, 194–198. https://doi.org/10.1016/j.seizure.2016.09.008.
Bifftu, B. B., Dachew, B. A., & Tiruneh, B. T. (2015). Perceived stigma and associated factors among people with epilepsy at Gondar University Hospital , Northwest Ethiopia : a cross-sectional institution based study. African health science, 15(4).
Shibre Teshome, A. A., Redda, T.-H., Girmay, M., & Lars, J. (2006). Perception of stigma among family members of patients epilepsy and their relatives in Butajira. Ethiopia. Ethiop J Health Dev., 20(3), 170–176.
Fernandes, P. T., Salgado, P. C. B., Noronha, A. L. A., Barbosa, F. D., Souza, E. A. P., Sander, J. W., et al. (2007). Prejudice towards chronic diseases: Comparison among epilepsy AIDS and diabetes. Seizure, 16(4), 320–323. https://doi.org/10.1016/j.seizure.2007.01.008.
Ormel, J., Lindenberg, S., Steverink, N., & Vonkorff, M. (1997). Quality of life and social production functions: A framework for understanding health effects. Social Science and Medicine, 45(7), 1051–1063.
Haritomeni, P., Aikaterini, T., Theofanis, V., Elizabeth, D., Ioannis, H., Konstantinos, V., et al. (2006). The Greek version of the quality of life in epilepsy inventory (QOLIE-31). Quality of life research, 15(5), 833–839.
Kubota, H., & Awaya, Y. (2010). Assessment of health-related quality of life and influencing factors using QOLIE-31 in Japanese patients with epilepsy. Epilepsy and Behavior, 18(4), 381–387.
Pimpalkhute, S. A., Bajait, C. S., Dakhale, G. N., Sontakke, S. D., Jaiswal, K. M., & Kinge, P. (2015). Assessment of quality of life in epilepsy patients receiving anti-epileptic drugs in a tertiary care teaching hospital. Indian Journal of Pharmacology, 47(5), 551–554. https://doi.org/10.4103/0253-7613.165198.
Salih, M. H., & Landers, T. (2019). The concept analysis of stigma towards chronic illness patient. Hospice and Palliative Medicine International Journal, 3(4), 132–136. https://doi.org/10.15406/hpmij.2019.03.00166.
Baker, G. A., Jacoby, A., Buck, D., Stalgis, C., & Monnet, D. (1997). Quality of life of people with epilepsy: A European study. Epilepsia, 38(3), 353–362. https://doi.org/10.1111/j.1528-1157.1997.tb01128.x.
Loring, D. W., Meador, K. J., & Lee, G. P. (2004). Determinants of quality of life in epilepsy. Epilepsy and Behavior, 5(6), 976–980. https://doi.org/10.1016/j.yebeh.2004.08.019.
Acknowledgements
We are very thankful to the University of Gondar for the approval of the ethical issue and its technical and financial support. We forward our appreciation to the hospital managers for allowing us to conduct this research and their cooperation. Finally, we would like to thank study participants for their volunteer participation and also data collectors and supervisors for their genuineness and quality of work during data collection.
Funding
This is part of a master thesis funded by the University of Gondar. The funders had no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained from the Ethical Review Board of the Institute of Public Health, College of Medicine and Health Science, University of Gondar (Ref. No.: IPH/180/2019). Permission letters were obtained from the University of Gondar comprehensive specialized hospital. All study participants were oriented on the objectives and purpose of the study before study participation. Confidentiality and anonymity were explained. Patients at health facilities and sick individuals were informed that participation had no impact on the provision of their health care. Written informed consent was obtained, and study team members safeguarded the confidentiality and anonymity of study participants throughout the entire study. Interviews were conducted in quiet areas, enclosed whenever possible, to ensure participant privacy. In order to protect the identities of the study participants, each participant was given a unique identification number (ID). Participation in the study was voluntary and individuals were free to withdraw or stop the interview at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Addis, B., Minyihun, A. & Aschalew, A.Y. Health-related quality of life and associated factors among patients with epilepsy at the University of Gondar comprehensive specialized hospital, northwest Ethiopia. Qual Life Res 30, 729–736 (2021). https://doi.org/10.1007/s11136-020-02666-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02666-4