Abstract
Purpose
Health-related quality of life (HRQOL) is an important outcome in economic evaluations of health care interventions for older adults. The aim of this study was to compare two commonly used preference-based utility measures, SF-6D and EQ-5D, to provide knowledge on their applicability when evaluating falls prevention interventions in primary health care.
Methods
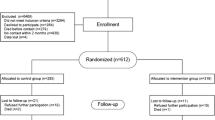
The study is a secondary analysis of longitudinal data from a randomised controlled trial, which included 155 older home care recipients participating in a falls prevention intervention in Norway. HRQOL was measured by SF-6D and EQ-5D. Physical function was measured by Berg Balance Scale, 4-m walk test, 30-s sit-to-stand and Falls Efficacy Scale International. Assessments were performed at baseline, 3 months and 6 months. The agreement between SF-6D and EQ-5D was examined using Bland–Altman plots and Spearman correlations. Elasticities from regression analysis were employed to compare the instruments’ responsiveness.
Results
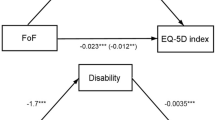
SF-6D and EQ-5D were strongly correlated (0.71), but there were differences in the instruments’ agreement and domains of HRQOL covered. Participants with a higher mean HRQOL and/or better physical function scored generally higher on EQ-5D. Participants with a lower mean HRQOL and/or poorer physical function achieved a relatively higher score on SF-6D. EQ-5D was more responsive to changes in physical function compared to SF-6D.
Conclusions
SF-6D and EQ-5D have both similarities and differences regarding sensitivity, domains covered and responsiveness to changes when evaluating a falls prevention intervention. Selecting the appropriate instrument depends on the characteristics of the participants and the intervention being evaluated.


Similar content being viewed by others
References
World Health Organization. (2015). World report on ageing and health. Geneva, Switzerland: World Health Organization.
Kannus, P., Sievänen, H., Palvanen, M., Järvinen, T., & Parkkari, J. (2005). Prevention of falls and consequent injuries in elderly people. The Lancet,366(9500), 1885–1893. https://doi.org/10.1016/S0140-6736(05)67604-0.
Stenhagen, M., Ekstrom, H., Nordell, E., & Elmstahl, S. (2014). Accidental falls, health-related quality of life and life satisfaction: A prospective study of the general elderly population. Archives of Gerontology and Geriatrics,58(1), 95–100. https://doi.org/10.1016/j.archger.2013.07.006.
Davis, J. C., Best, J. R., Dian, L., Khan, K. M., Hsu, C. L., Chan, W., et al. (2017). Are the EQ-5D-3L and the ICECAP-O responsive among older adults with impaired mobility? Evidence from the Vancouver Falls Prevention Cohort Study. Quality of Life Research,26(3), 737–747. https://doi.org/10.1007/s11136-016-1487-z.
Bjerk, M., Brovold, T., Skelton, D. A., & Bergland, A. (2018). Associations between health-related quality of life, physical function and fear of falling in older fallers receiving home care. BMC Geriatrics,18(1), 253. https://doi.org/10.1186/s12877-018-0945-6.
Fletcher, P. C., & Hirdes, J. P. (2004). Restriction in activity associated with fear of falling among community-based seniors using home care services. Age and Ageing,33(3), 273–279. https://doi.org/10.1093/ageing/afh077.
Hektoen, L. F., Aas, E., & Lurås, H. (2009). Cost-effectiveness in fall prevention for older women. Scandinavian Journal of Public Health,37(6), 584–589. https://doi.org/10.1177/1403494809341093.
Gillespie, L. D., Robertson, M. C., Gillespie, W. J., Sherrington, C., Gates, S., Clemson, L. M., et al. (2012). Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD007146.pub3.
El-Khoury, F., Cassou, B., Charles, M.-A., & Dargent-Molina, P. (2013). The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: Systematic review and meta-analysis of randomised controlled trials. BMJ,347, f6234. https://doi.org/10.1136/bmj.f6234.
Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., & Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes (4th ed.). Oxford, UK: Oxford University Press.
Brazier, J., Roberts, J., Tsuchiya, A., & Busschbach, J. (2004). A comparison of the EQ-5D and SF-6D across seven patient groups. Health Economics,13(9), 873–884. https://doi.org/10.1002/hec.866.
Haywood, K., Garratt, A., & Fitzpatrick, R. (2005). Quality of life in older people: A structured review of generic self-assessed health instruments. Quality of Life Research,14(7), 1651–1668. https://doi.org/10.1007/s11136-005-1743-0.
Gerard, K., Nicholson, T., Mullee, M., Mehta, R., & Roderick, P. (2004). EQ-5D versus SF-6D in an older, chronically ill patient group. Applied Health Economics and Health Policy,3(2), 91–102. https://doi.org/10.2165/00148365-200403020-00005.
Petrou, S., & Hockley, C. (2005). An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health Economics,14(11), 1169–1189. https://doi.org/10.1002/hec.1006.
van Stel, H. F., & Buskens, E. (2006). Comparison of the SF-6D and the EQ-5D in patients with coronary heart disease. Health and Quality of Life Outcomes,4(1), 20. https://doi.org/10.1186/1477-7525-4-20.
Cunillera, O., Tresserras, R., Rajmil, L., Vilagut, G., Brugulat, P., Herdman, M., et al. (2010). Discriminative capacity of the EQ-5D, SF-6D, and SF-12 as measures of health status in population health survey. Quality of Life Research,19(6), 853–864. https://doi.org/10.1007/s11136-010-9639-z.
Chen, J., Wong, C. K., McGhee, S. M., Pang, P. K., & Yu, W.-C. (2014). A comparison between the EQ-5D and the SF-6D in patients with chronic obstructive pulmonary disease (COPD). PLoS ONE,9(11), e112389. https://doi.org/10.1371/journal.pone.0112389.
Kontodimopoulos, N., Pappa, E., Papadopoulos, A. A., Tountas, Y., & Niakas, D. (2009). Comparing SF-6D and EQ-5D utilities across groups differing in health status. Quality of Life Research,18(1), 87–97. https://doi.org/10.1007/s11136-008-9420-8.
Lamers, L., Bouwmans, C., van Straten, A., Donker, M., & Hakkaart, L. (2006). Comparison of EQ-5D and SF-6D utilities in mental health patients. Health Economics,15(11), 1229–1236. https://doi.org/10.1002/hec.1125.
McDonough, C. M., & Tosteson, A. N. (2007). Measuring preferences for cost-utility analysis: How choice of method may influence decision-making. Pharmacoeconomics,25(2), 93–106. https://doi.org/10.2165/00019053-200725020-00003.
Joore, M., Brunenberg, D., Nelemans, P., Wouters, E., Kuijpers, P., Honig, A., et al. (2010). The impact of differences in EQ-5D and SF-6D utility scores on the acceptability of cost-utility ratios: Results across five trial-based cost–utility studies. Value in Health,13(2), 222–229. https://doi.org/10.1111/j.1524-4733.2009.00669.x.
Bjerk, M., Brovold, T., Skelton, D. A., & Bergland, A. (2017). A falls prevention programme to improve quality of life, physical function and falls efficacy in older people receiving home help services: Study protocol for a randomised controlled trial. BMC Health Services Research,17(1), 559. https://doi.org/10.1186/s12913-017-2516-5.
Bjerk, M., Brovold, T., Skelton, D. A., Liu-Ambrose, T., & Bergland, A. (2019). Effects of a falls prevention exercise programme on health-related quality of life in older home care recipients: A randomised controlled trial. Age and Ageing,48(2), 213–219. https://doi.org/10.1093/ageing/afy192.
von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gotzsche, P. C., Vandenbroucke, J. P., et al. (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. The Lancet,370(9596), 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X.
Loge, J. H., & Kaasa, S. (1998). Short Form 36 (SF-36) health survey: Normative data from the general Norwegian population. Scandinavian Journal of Public Health,26(4), 250–258. https://doi.org/10.1177/14034948980260040401.
Walters, S. J., & Brazier, J. E. (2005). Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Quality of Life Research,14(6), 1523–1532. https://doi.org/10.1007/s11136-004-7713-0.
The EuroQol Group. (1990). EuroQol - a new facility for the measurement of health-related quality of life. Health Policy,16(3), 199–208. https://doi.org/10.1016/0168-8510(90)90421-9.
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care,42, 851–859.
Berg, K. O., Maki, B. E., Williams, J. I., Holliday, P. J., & Wood-Dauphinee, S. L. (1992). Clinical and laboratory measures of postural balance in an elderly population. Archives of Physical Medicine and Rehabilitation,73(11), 1073–1080.
Peters, D., Fritz, S., & Krotish, D. (2013). Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. Journal of Geriatric Physical Therapy,36(1), 24–30. https://doi.org/10.1519/JPT.0b013e318248e20d.
Jones, C. J., Rikli, R. E., & Beam, W. C. (1999). A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport,70(2), 113–119. https://doi.org/10.1080/02701367.1999.10608028.
Helbostad, J. L., Taraldsen, K., Granbo, R., Yardley, L., Todd, C. J., & Sletvold, O. (2010). Validation of the falls efficacy scale-international in fall-prone older persons. Age and Ageing,39(2), 259. https://doi.org/10.1093/ageing/afp224.
Marques-Vieira, C. M. A., Sousa, L. M. M., Severino, S., Sousa, L., & Caldeira, S. (2016). Cross-cultural validation of the falls efficacy scale international in elderly: Systematic literature review. Journal of Clinical Gerontology and Geriatrics,7(3), 72–76. https://doi.org/10.1016/j.jcgg.2015.12.002.
Tombaugh, T. N., & McIntyre, N. J. (1992). The mini-mental state examination: A comprehensive review. Journal of the American Geriatrics Society,40(9), 922–935. https://doi.org/10.1111/j.1532-5415.1992.tb01992.x.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2013). Applied multiple regression/correlation analysis for the behavioral sciences. London: Routledge.
Greene, W. H. (2012). Econometric analysis. Boston: Pearson.
Karimi, M., & Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics,34(7), 645–649. https://doi.org/10.1007/s40273-016-0389-9.
Grund, S., Breitinger, E., Fricke, S., Alpers, G. W., Hundsdörfer, W., & Schäfer, H.-G. (2017). Health-related quality of life measurement inpatient geriatric rehabilitation: A comparison of the feasibility and suitability between the SF-36 and EQ-5D-5L questionnaires. Journal of Gerontology & Geriatric Research,6(6), 458. https://doi.org/10.4172/2167-7182.1000458.
Sørensen, J., Davidsen, M., Gudex, C., Pedersen, K. M., & Brønnum-Hansen, H. (2009). Danish EQ-5D population norms. Scandinavian Journal of Public Health,37(5), 467–474. https://doi.org/10.1177/1403494809105286.
van den Berg, B. (2012). Sf-6d population norms. Health Economics,21(12), 1508–1512. https://doi.org/10.1002/hec.1823.
Christiansen, T., Lauridsen, J. T., Kifmann, M., Lyttkens, C. H., Ólafsdóttir, T., & Valtonen, H. (2018). Healthcare, health and inequality in health in the Nordic countries. Nordic Journal of Health Economics,6(2), 10. https://doi.org/10.5617/njhe.5955.
Leegaard, M., Utne, I., Halvorsrud, L., Valeberg, B. T., Torbjørnsen, A., Bjørnnes, A. K., et al. (2018). A review of self-rated generic quality of life instruments used among older patients receiving home care nursing. Health and Social Care in the Community,26(3), e321–e328. https://doi.org/10.1111/hsc.12447.
Hickey, A., Barker, M., McGee, H., & O’boyle, C. (2005). Measuring health-related quality of life in older patient populations: A review of current approaches. Pharmacoeconomics,23(10), 971–993. https://doi.org/10.2165/00019053-200523100-00002.
Brazier, J. E., Walters, S. J., Nicholl, J., & Kohler, B. (1996). Using the SF-36 and Euroqol on an elderly population. Quality of Life Research,5(2), 195–204. https://doi.org/10.1007/BF00434741.
Funding
This study did not receive external funding. Internal funding is provided by the OsloMet – Oslo Metropolitan University. The institution had no role in the design, conduct of research or decision of publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The project proposal has been approved by The Regional Committee for Medical Research Ethics in South East Norway (Ref. 2014/2051).
Informed consent
Written informed consent was obtained from all participants before baseline testing.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bjerk, M., Brovold, T., Davis, J.C. et al. Evaluating a falls prevention intervention in older home care recipients: a comparison of SF-6D and EQ-5D. Qual Life Res 28, 3187–3195 (2019). https://doi.org/10.1007/s11136-019-02258-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02258-x