Abstract
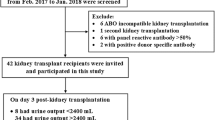
Background Mycophenolic acid is widely used immunosuppressive drug, associated with adverse effects which increase patient morbidity and decrease medication adherence. Objective To evaluate the adverse effects in renal transplant recipients under mycophenolate treatment with respect to gender. Setting University Clinical Centre of Nis, Clinic of Nephrology, Serbia. Method This research included 96 renal transplant recipients, who received immunosuppressive regimen, based on tacrolimus or cyclosporin A, prednisone and mycophenolic acid. The high-performance liquid chromatography method combined with protein precipitation was used for the analysis of mycophelate concentration in human plasma. Drug concentration and dose-adjusted concentration were determined with respect to the patients’ gender. An adverse effect scoring system developed by nephrologists within the University of Buffalo Nephrology/Transplant Program was used to monitor adverse effects of therapy. Main outcome measure Individual and scores of adverse effects in relation to the dosing regimen and gender. Results Results showed statistically lower dose and concentrations in men compared to the women in our investigation group. Also, female patients demonstrated higher mean scores (cumulative and subscores) within the same dosing regimens of mycophenolic acid. The gastrointestinal score was significantly higher in women who received a dose greater than 720 mg compared to men (0.20 ± 0.12 vs 0.12 ± 0.12). Women demonstrated higher individual adverse effects such as diarrhea and skin changes (41.7 vs 17.0; p = 0.038 and 62.5 vs 30.2; p = 0.037, respectively). Conclusions The results of our research showed that recipients’ gender may play an important role in pharmacokinetic profile of mycophenolic acid, suggesting that women had higher concentration of mycophenolic acid and more serious side effects.

Similar content being viewed by others
References
Halloran PF. Immunosuppressive drugs for kidney transplantation. N Engl J Med. 2004;351(26):2715–29.
Kamińska J, Głyda M, Sobiak J, Chrzanowska M. Pharmacokinetics of mycophenolic acid and its phenyl glucuronide metabolite in kidney transplant recipients with renal impairment. Arch Med Sci. 2012;8(1):88–96.
Patel CG, Ogasawara K, Akhlaghi F. Mycophenolic acid glucuronide (MPAG) is transported by multidrug resistance-associated protein 2 (MRP2) and this transport is not inhibited by cyclosporine, tacrolimus or sirolimus. Xenobiotica. 2013;43(3):229–35.
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9(Suppl 3):S1–155.
Dobbels F, Moons P, Abraham I, Larsen CP, Dupont L, De Geest S. Measuring symptom experience of side-effects of immunosuppressive drugs: the Modified Transplant Symptom Occurrence and Distress Scale. Transpl Int. 2008;21(8):764–73.
Fiebiger W, Mitterbauer C, Oberbauer R. Health-related quality of life outcomes after kidney transplantation. Health Qual Life Out. 2004;2:2.
Chisholm MA, Lance CE, Mulloy LL. Patient factors associated with adherence to immunosuppressant therapy in renal transplant recipients. Am J Health Syst Pharm. 2005;62(17):1775–81.
Pinsky BW, Takemoto SK, Lentine KL, Burroughs TE, Schnitzler MA, Salvalaggio PR. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Am J Transplant. 2009;9(11):2597–606.
Shaw LM, Figurski M, Milone MC, Trofe J, Bloom RD. Therapeutic drug monitoring of mycophenolic acid. Clin J Am Soc Nephrol. 2007;2(5):1062–72.
Jeong H, Kaplan B. Therapeutic monitoring of mycophenolate mofetil. Clin J Am Soc Nephrol. 2007;2:184–91.
Miura M, Niioka T, Kato S, Kagaya H, Saito M, Habuchi T, et al. Monitoring of mycophenolic acid predose concentrations in the maintenance phase more than one year after renal transplantation. Ther Drug Monit. 2011;33(3):295–302.
Shaw LM, Korecka M, Venkataramanan R, Goldbergc L, Bloom R, Brayman KL. Mycophenolic acid pharmacodynamics and pharmacokinetics provide a basis for rational monitoring strategies. Am J Transplant. 2003;3:534–42.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin Pharmacokinet. 2007;46:13–58.
Takekuma Y, Kakiuchi H, Yamazaki K, Miyauchi S, Kikukawa T, Kamo N, et al. Difference between pharmacokinetics of mycophenolic acid (MPA) in rats and that in humans is caused by different affinities of MRP2 to a glucuronized form. J Pharm Pharm Sci. 2007;10(1):71–85.
Tornatore KM, Meaney CJ, Wilding GE, Chang SS, Gundroo A, Cooper LM, et al. Influence of sex and race on mycophenolic acid pharmacokinetics in stable African American and Caucasian renal transplant recipients. Clin Pharmacokinet. 2015;54(4):423–34.
Savvidaki E, Papachristou E, Kazakopoulos P, Papasotiriou M, Vardoulaki M, Goumenos DS. Gastrointestinal disorders after renal transplantation. Transplant Proc. 2014;46(9):3183–6.
van Hest RM, van Gelder T, Vulto AG, Mathot RA. Population pharmacokinetics of mycophenolic acid in renal transplant recipients. Clin Pharmacokinet. 2005;44(10):1083–96.
Buckley DB, Klaassen CD. Tissue- and gender-specific mRNA expression of UDP-glucuronosyltransferases (UGTs) in mice. Drug Metab Dispos. 2007;35(1):121–7.
Gallagher CJ, Balliet RM, Sun D, Chen G, Lazarus P. Sex differences in UDP- glucuronosyltransferase 2B17 expression and activity. Drug Metab Dispos. 2010;38(12):2204–9.
Mathis AS, Egloff G, Ghin HL. Calcineurin inhibitor sparing strategies in renal transplantation, part one: late sparing strategies. World J Transplant. 2014;4(2):57–80.
Musuamba FT, Mourad M, Haufroid V, De Meyer M, Capron A, Delattre IK, et al. Statistical tools for dose individualization of mycophenolic acid and tacrolimus co-administered during the first month after renal transplantation. Br J Clin Pharmacol. 2013;75(5):1277–88.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70.
Džodić P, Veličković-Radovanović R, Šmelcerović A, Catić-Đorđević A, Stefanović N, Spasić A, et al. Validation of HPLC method for the determination of mycophenolic acid in human plasma obtained from renal transplant recipients. Acta Med Medianae. 2016;55(4):28–36.
Meaney CJ, Arabi Z, Venuto RC, Consiglio JD, Wilding GE, Tornatore KM. Validity and reliability of a novel immunosuppressive adverse effects scoring system in renal transplant recipients. BMC Nephrol. 2014;15:88.
De Winter BC, van Gelder T, Sombogaard F, Shaw LM, van Hest RM, Mathot RA. Pharmacokinetic role of protein binding of mycophenolic acid and its glucuronide metabolite in renal transplant recipients. J Pharmacokinet Pharmacodyn. 2009;36:541–64.
Langone A, Shihab F, Pankewycz O, Doria C, Wiland A, McCague K, et al. Long-term dosing patterns of enteric-coated mycophenolate sodium or mycophenolate mofetil with tacrolimus after renal transplantation. Clin Transplant. 2014;28(9):961–7.
Staatz CE, Tett SE. Pharmacology and toxicology of mycophenolate in organ transplant recipients: an update. Arch Toxicol. 2014;88(7):1351–89.
Veličković-Radovanović R, Mikov M, Paunović G, Djordjević V, Stojanović M, Cvetković T, et al. Gender differences in pharmacokinetics of tacrolimus and their clinical significance in kidney transplant recipients. Gend Med. 2011;8(1):23–31.
Veličković-Radovanović R, Mikov M, Catić-Đorđević A, Stefanović N, Stojanović M, Jokanović M, et al. Tacrolimus as a part of immunosuppressive treatment in kidney transplantation patients: sex differences. Gend Med. 2012;9(6):471–80.
Pescovitz MD, Guasch A, Gaston R, Rajagopalan P, Tomlanovich S, Weinstein S, et al. Equivalent pharmacokinetics of mycophenolate mofetil in African-American and Caucasian male and female stable renal allograft recipients. Am J Transplant. 2003;3(12):1581–6.
Shaw LM, Korecka M, Aradhye S, Grossman R, Bayer L, Innes C, et al. Mycophenolic acid area under the curve values in African American and Caucasian renal transplant patients are comparable. J Clin Pharmacol. 2000;40(6):624–33.
Sterneck M, Settmacher U, Ganten T, Sarrazin C, Speidel N, Broering D. Improvement in gastrointestinal and health-related quality of life outcomes after conversion from mycophenolate mofetil to enteric-coated mycophenolate sodium in liver transplant recipients. Transplant Proc. 2014;46(1):234–40.
Xu L, Cai M, Shi BY, Li ZL, Li X, Jin HL. A prospective analysis of the effects of enteric-coated mycophenolate sodium and mycophenolate mofetil co-medicated with a proton pump inhibitor in kidney transplant recipients at a single institute in China. Transplant Proc. 2014;46(5):1362–5.
Vanhove T, Kuypers D, Claes KJ, Evenepoel P, Meijers B, Naesens M, et al. Reasons for dose reduction of mycophenolate mofetil during the first year after renal transplantation and its impact on graft outcome. Transpl Int. 2013;26(8):813–21.
Lucan VC, Berardinelli L. Gastrointestinal side effects of post-transplant therapy. J Gastrointestin Liver Dis. 2016;25(3):367–73.
Momper JD, Misel ML, McKay DB. Sex differences in transplantation. Transplant Rev. 2017;31(3):145–50.
Liapis G, Boletis J, Skalioti C, Bamias G, Tsimaratou K, Patsouris E, et al. Histological spectrum of mycophenolate mofetil-related colitis: association with apoptosis. Histopathology. 2013;63(5):649–58.
Morissette P, Albert C, Busque S, St-Louis G, Vinet B. In vivo higher glucuronidation of mycophenolic acid in male than in female recipients of a cadaveric kidney allograft and under immunosuppressive therapy with mycophenolate mofetil. Ther Drug Monit. 2001;23(5):520–5.
Bunnapradist S, Ambuhl PM. Impact of gastrointestinal-related side effects on mycophenolate mofetil dosing and potential therapeutic strategies. Clin Transplant. 2008;22(6):815–21.
Zhang H, Liu L, Li J, Fu Q, Wan J, Deng R, et al. The efficacy and safety of intensified enteric-coated mycophenolate sodium with low exposure of calcineurin inhibitors in Chinese de novo kidney transplant recipients: a prospective study. Int J Clin Pract. 2016;70(S185):22–30.
Mahé E, Morelon E, Lechaton S, Sang KH, Mansouri R, Ducasse MF, et al. Cutaneous adverse events in renal transplant recipients receiving sirolimus-based therapy. Transplantation. 2005;79(4):476–82.
Zaza G, Tomei P, Ria P, Granata S, Boschiero L, Lupo A. Systemic and nonrenal adverse effects occurring in renal transplant patients treated with mTOR inhibitors. Clin Dev Immunol. 2013;2013:403280.
Sinangil A, Celik V, Barlas S, Sakaci T, Koc Y, Basturk T, et al. New-onset diabetes after kidney transplantation and pretransplant hypomagnesemia. Prog Transplant. 2016;26(1):55–61.
Mourad G, Glyda M, Albano L, Viklický O, Merville P, Tydén G, et al. Incidence of posttransplantation diabetes mellitus in de novo kidney transplant recipients receiving prolonged-release tacrolimus-based immunosuppression with 2 different corticosteroid minimization strategies: advance, a randomized controlled trial. Transplantation. 2017;101(8):1924–34.
Acknowledgements
The authors would like to thank Dr. Rocco Venuto, who gave us the support to apply the immunosuppressive adverse effects scoring system to our patients.
Funding
This study was supported by a grant from the Ministry of Education, Science and Technological Development of the Republic of Serbia—Project Nos. 41018 and 172044.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spasić, A., Catić-Đorđević, A., Veličković-Radovanović, R. et al. Adverse effects of mycophenolic acid in renal transplant recipients: gender differences. Int J Clin Pharm 41, 776–784 (2019). https://doi.org/10.1007/s11096-019-00837-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00837-z