Abstract
Purpose/objective(s)
Tyrosine kinase inhibitors (TKIs) are commonly employed for patients with brain metastases from lung cancer and specific driver mutations. We sought to identify the correlation between intracranial tumor burden and outcomes in patients with brain metastases treated with TKIs.
Materials/methods
We identified and retrospectively reviewed cases of EGFR-mutant or ALK-rearranged lung cancer with brain metastases at any time during their cancer course. Clinical characteristics and treatment information were abstracted from the medical records. Brain metastases were contoured to calculate total volume of disease at diagnosis and after initial therapy. High intracranial burden was defined as either > 10 brain metastases, volume of brain metastases > 15 cc, or largest lesion > 3 cm. Intracranial response was determined according to Response Assessment in Neuro-Oncology (RANO) criteria on the patient level. We determined the correlation between clinical and imaging characteristics and intracranial progression free survival (IC-PFS) and overall survival (OS).
Results
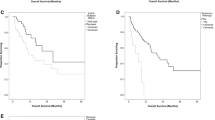
Fifty-seven patients with EGFR (n = 49) and ALK (n = 8) alterations were identified. Median follow-up from initial brain metastasis diagnosis was 17 months. Neurological symptoms were present in 54% at brain metastasis diagnosis. For those receiving TKIs alone or TKIs with radiation, at least a partial intracranial response (≥ 65% volume reduction) at 3 months from starting therapy was achieved in 94% and 58%. Progressive intracranial disease at 3 months occurred in 6.3% and 8.3%. Patients with high intracranial burden (n = 21) had a median 17 brain metastases, 6.5 cc volume, and 1.9 cm maximal tumor diameter. Median IC-PFS and OS for patients with high intracranial burden was 13.9 and 35.4 months. Patients with high intracranial burden and neurological symptoms at diagnosis had similar IC-PFS and OS compared to those with low burden and absence of neurological symptoms (p > 0.05 for each).
Conclusion
Most patients receiving TKIs as part of their initial therapy achieve an early and durable volumetric intracranial response, irrespective of presenting disease burden or neurologic symptoms.




Similar content being viewed by others
References
Mitra D, Chen YH, Li R et al (2019) EGFR mutant locally advanced non-small cell lung cancer is at increased risk of brain metastasis. Clin Transl Radiat Oncol 18:32–38
Rangachari D, Yamaguchi N, VanderLaan PA et al (2015) Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers. Lung Cancer 88(1):108–111
Chun SG, Choe KS, Iyengar P et al (2012) Isolated central nervous system progression on Crizotinib: an Achilles heel of non-small cell lung cancer with EML4-ALK translocation? Cancer Biol Ther 13(14):1376–1383
Yuan M, Huang LL, Chen JH et al (2019) The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct Target Ther 4:61
Gadgeel SM, Gandhi L, Riely GJ et al (2014) Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol 15(10):1119–1128
Reungwetwattana T, Nakagawa K, Cho BC et al (2018) CNS response to osimertinib versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-mutated advanced non-small-cell lung cancer. J Clin Oncol. https://doi.org/10.1200/JCO.2018.78.3118
Cho BC, Chewaskulyong B, Lee KH et al (2019) Osimertinib versus standard of care EGFR TKI as first-line treatment in patients with EGFRm advanced NSCLC: FLAURA Asian subset. J Thorac Oncol 14(1):99–106
NCCN (2020) Central Nervous System Cancers Version 1.2020. National Comprehensive Cancer Network
Magnuson WJ, Lester-Coll NH, Wu AJ et al (2017) Management of brain metastases in tyrosine kinase inhibitor-naive epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol 35(10):1070–1077
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70(2):510–514
Mahajan A, Ahmed S, McAleer MF et al (2017) Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1040–1048
Sperduto PW, Yang TJ, Beal K et al (2017) Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (lung-molGPA). JAMA Oncol 3(6):827–831
Johung KL, Yeh N, Desai NB et al (2016) Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J Clin Oncol 34(2):123–129
Services, U.S.D.o.H.a.H. (2017) Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. Accessed 27 Nov 2017
Lin NU, Lee EQ, Aoyama H et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270–e278
Ramalingam SS, Vansteenkiste J, Planchard D et al (2020) Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med 382(1):41–50
Peters S, Mok T, Gadgeel S et al (2020) Updated overall survival (OS) and safety data from the randomized, phase III ALEX study of alectinib (ALC) versus crizotinib (CRZ) in untreated advanced ALK + NSCLC. J Clin Oncol
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060
Dutta SW, Sheehan JP, Niranjan A et al (2018) Evolution in the role of stereotactic radiosurgery in patients with multiple brain metastases: an international survey. J Clin Neurosci 57:6–12
Oh Y, Taylor S, Bekele BN et al (2009) Number of metastatic sites is a strong predictor of survival in patients with nonsmall cell lung cancer with or without brain metastases. Cancer 115(13):2930–2938
Peters S, Bexelius C, Munk V et al (2016) The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer. Cancer Treat Rev 45:139–162
Gadgeel S, Peters S, Mok T et al (2018) Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK +) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol 29(11):2214–2222
Yap TA, Popat S (2017) Targeting MET Exon 14 skipping alterations: has lung cancer MET its match? J Thorac Oncol 12(1):12–14
Ackermann CJ, Stock G, Tay R et al (2019) Targeted therapy for RET-rearranged non-small cell lung cancer: clinical development and future directions. Onco Targets Ther 12:7857–7864
Drilon A (2019) TRK inhibitors in TRK fusion-positive cancers. Ann Oncol 30(8):viii23–viii30
Katayama R, Gong B, Togashi N et al (2019) The new-generation selective ROS1/NTRK inhibitor DS-6051b overcomes crizotinib resistant ROS1-G2032R mutation in preclinical models. Nat Commun 10(1):3604
Chinnaiyan P, Huang S, Vallabhaneni G et al (2005) Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva). Cancer Res 65(8):3328–3335
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Informed consent
Research data: Patient level data not allowed to be shared per IRB. Author responsible for statistical analysis: SWD.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutta, S.W., Mack, M.L., Aliotta, E. et al. Intracranial disease control for EGFR-mutant and ALK-rearranged lung cancer with large volume or symptomatic brain metastases. J Neurooncol 149, 357–366 (2020). https://doi.org/10.1007/s11060-020-03615-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03615-4



