Abstract
Introduction
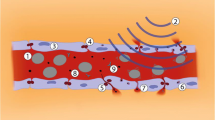
Glioblastoma (GBM) is the most common and aggressive primary brain cancer in adults. Few cytotoxic chemotherapies have been shown to be effective against GBM, due in part to the presence of the blood–brain barrier (BBB), which reduces the penetration of chemotherapies from the blood to the brain. Ultrasound-induced BBB opening (US-BBB) has been shown to increase the penetration of multiple chemotherapeutic agents in the brain in animal models. In the current study, the anti-tumor activity of carboplatin chemotherapy with and without US-BBB was investigated in several GBM mouse models.
Methods
First, the IC50 of two commercial (U87 and U251) and six patient-derived GBM cell lines (PDCL) to carboplatin was measured. Next, U87 was subcutaneously grafted to a nude mouse model to test the in vivo response of the tumor to carboplatin in the absence of the BBB. Lastly, nude mice bearing orthotopically xenografted GBM cell lines (U87 or a PDCL) were randomized to four experimental groups: (i) untreated, (ii) US-BBB alone, (iii) carboplatin alone and, (iv) carboplatin + US-BBB. Mice were treated once weekly for 4 weeks and monitored for toxicity, tumor growth, and survival.
Results
Carboplatin plus US-BBB enhanced survival (p = 0.03) and delayed tumor growth (p < 0.05) of GBM-bearing mice compared to carboplatin alone, with a 4.2-fold increase of carboplatin penetration in the brain, without evidence of significant neurological or systemic toxicity.
Conclusions
Carboplatin efficacy was enhanced in GBM mouse models with US-BBB and appears to be a promising chemotherapy for this approach.





Similar content being viewed by others
References
Ostrom QT, Bauchet L, Davis FG et al (2014) The epidemiology of glioma in adults: a “state of the science” review. Neuro-Oncol 16:896–913. https://doi.org/10.1093/neuonc/nou087
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. https://doi.org/10.1056/NEJMoa043330
Vanderbeek AM, Rahman R, Fell G et al (2018) The clinical trials landscape for glioblastoma: is it adequate to develop new treatments? Neuro-Oncol 20:1034–1043. https://doi.org/10.1093/neuonc/noy027
Dréan A, Goldwirt L, Verreault M et al (2016) Blood–brain barrier, cytotoxic chemotherapies and glioblastoma. Expert Rev Neurother. https://doi.org/10.1080/14737175.2016.1202761
Hynynen K, McDannold N, Vykhodtseva N, Jolesz FA (2001) Noninvasive MR imaging-guided focal opening of the blood–brain barrier in rabbits. Radiology 220:640–646. https://doi.org/10.1148/radiol.2202001804
Raymond SB, Skoch J, Hynynen K, Bacskai BJ (2007) Multiphoton imaging of ultrasound/optison mediated cerebrovascular effects in vivo. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 27:393–403. https://doi.org/10.1038/sj.jcbfm.9600336
Sheikov N, McDannold N, Vykhodtseva N et al (2004) Cellular mechanisms of the blood–brain barrier opening induced by ultrasound in presence of microbubbles. Ultrasound Med Biol 30:979–989. https://doi.org/10.1016/j.ultrasmedbio.2004.04.010
Beccaria K, Canney M, Goldwirt L et al (2015) Ultrasound-induced opening of the blood–brain barrier to enhance temozolomide and irinotecan delivery: an experimental study in rabbits. J Neurosurg. https://doi.org/10.3171/2015.4.JNS142893
Goldwirt L, Canney M, Horodyckid C et al (2016) Enhanced brain distribution of carboplatin in a primate model after blood–brain barrier disruption using an implantable ultrasound device. Cancer Chemother Pharmacol 77:211–216. https://doi.org/10.1007/s00280-015-2930-5
Treat LH, McDannold N, Zhang Y et al (2012) Improved anti-tumor effect of liposomal doxorubicin after targeted blood–brain barrier disruption by MRI-guided focused ultrasound in rat glioma. Ultrasound Med Biol 38:1716–1725. https://doi.org/10.1016/j.ultrasmedbio.2012.04.015
Chen P-Y, Liu H-L, Hua M-Y et al (2010) Novel magnetic/ultrasound focusing system enhances nanoparticle drug delivery for glioma treatment. Neuro-Oncol 12:1050–1060. https://doi.org/10.1093/neuonc/noq054
Horodyckid C, Canney M, Vignot A et al (2017) Safe long-term repeated disruption of the blood–brain barrier using an implantable ultrasound device: a multiparametric study in primates. J Neurosurg 126:1351–1361
Downs ME, Buch A, Sierra C et al (2015) Long-term safety of repeated blood–brain barrier opening via focused ultrasound with microbubbles in non-human primates performing a cognitive task. PLoS ONE 10:e0125911. https://doi.org/10.1371/journal.pone.0125911
McDannold N, Arvanitis CD, Vykhodtseva N, Livingstone MS (2012) Temporary disruption of the blood–brain barrier by use of ultrasound and microbubbles: safety and efficacy evaluation in rhesus macaques. Cancer Res 72:3652–3663. https://doi.org/10.1158/0008-5472.CAN-12-0128
Carpentier A, Canney M, Vignot A et al (2016) Clinical trial of blood–brain barrier disruption by pulsed ultrasound. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aaf6086
Idbaih A, Canney M, Belin L et al (2019) Safety and feasibility of repeated and transient blood–brain barrier disruption by pulsed ultrasound in patients with recurrent glioblastoma. Clin Cancer Res Off J Am Assoc Cancer Res. https://doi.org/10.1158/1078-0432.CCR-18-3643
Aryal M, Vykhodtseva N, Zhang Y-Z et al (2013) Multiple treatments with liposomal doxorubicin and ultrasound-induced disruption of blood-tumor and blood–brain barriers improve outcomes in a rat glioma model. J Control Release Off J Control Release Soc 169:103–111. https://doi.org/10.1016/j.jconrel.2013.04.007
Yang F-Y, Horng S-C (2013) Ultrasound mediated delivery of liposomal doxorubicin in mice with glioma. Engineering 04:68. https://doi.org/10.4236/eng.2012.410B018
Kovacs Z, Werner B, Rassi A et al (2014) Prolonged survival upon ultrasound-enhanced doxorubicin delivery in two syngenic glioblastoma mouse models. J Control Release 187:74–82. https://doi.org/10.1016/j.jconrel.2014.05.033
Rosenberg S, Verreault M, Schmitt C et al (2016) Multi-omics analysis of primary glioblastoma cell lines shows recapitulation of pivotal molecular features of parental tumors. Neuro-Oncol. https://doi.org/10.1093/neuonc/now160
Agarwal S, Manchanda P, Vogelbaum MA et al (2013) Function of the blood–brain barrier and restriction of drug delivery to invasive glioma cells: findings in an orthotopic rat xenograft model of glioma. Drug Metab Dispos Biol Fate Chem 41:33–39. https://doi.org/10.1124/dmd.112.048322
Shin J, Kong C, Cho JS et al (2018) Focused ultrasound–mediated noninvasive blood–brain barrier modulation: preclinical examination of efficacy and safety in various sonication parameters. Neurosurg Focus 44:E15. https://doi.org/10.3171/2017.11.FOCUS17627
White E, Bienemann A, Taylor H et al (2012) A phase I trial of carboplatin administered by convection-enhanced delivery to patients with recurrent/progressive glioblastoma multiforme. Contemp Clin Trials 33:320–331. https://doi.org/10.1016/j.cct.2011.10.010
Prados MD, Warnick RE, Mack EE et al (1996) Intravenous carboplatin for recurrent gliomas. A dose-escalating phase II trial. Am J Clin Oncol 19:609–612
Acknowledgements
This research was funded in part by: Investissements d’avenir ANR-10-IAIHU-06, Institut Universitaire de Cancérologie, Fondation ARC pour la recherche sur le cancer, Association pour la Recherche sur les Tumeurs Cérébrales, Ligue Nationale Contre le Cancer, and support from CarThera (Paris, France). INCA-DGOS-Inserm_12560 SiRIC CURAMUS is financially supported by the French National Cancer Institute, the French Ministry of Solidarity and Health and INSERM and CarThera.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ahmed Idbaih reports receiving travel funding from CarThera (June 2018); Guillaume Bouchoux, Charlotte Schmitt, Michael Canney, and Frédéric Sottilini are employees of CarThera. Michael Canney and Alexandre Carpentier are paid consultants of CarThera. Alexandre Carpentier, Michael Canney, and Frédéric Sottilini have ownership interest in CarThera.
Ethical approval
All protocols involving live animals were reviewed and approved by a local animal ethics committee for welfare of animals (Ministère de l’Enseignement Supérieur et de la Recherche, Paris, France, Protocol #0113.02). PDCLs were obtained with signed patient consent form and stored in the certified OncoNeuroTek tissue bank.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2019_3204_MOESM1_ESM.pptx
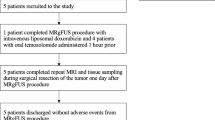
Online Resource 1 diagram of experiments. Each figure is represented in the discontinuous-line boxes with their number. (PPTX 36 kb)
Rights and permissions
About this article
Cite this article
Dréan, A., Lemaire, N., Bouchoux, G. et al. Temporary blood–brain barrier disruption by low intensity pulsed ultrasound increases carboplatin delivery and efficacy in preclinical models of glioblastoma. J Neurooncol 144, 33–41 (2019). https://doi.org/10.1007/s11060-019-03204-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03204-0