Abstract
The intervention “This is My Story” (TIMS) was previously developed and presented as a case study involving chaplains and support to non-communicative patients (Tracey et al in J Religion Health, 60(5):3282–3290, 2021). This further investigation aims to determine feasibility by looking at eight criteria: acceptability, demand, implementation, practicality, adaptation, integration, expansion, and limited-efficacy testing (Bowen et al in Am J Prev Med 36(5):452–457, 2009). Chaplains conducted recorded conversation with a patient’s loved one, then it was edited for brevity and succinctness, and uploaded to the patient’s medical chart and can be listened to at any time by medical providers. A completed interview, posted to the patient’s electronic medical record (EMR), and able to be listened to by the medical team, was found to be contingent upon two factors: proximity to time between referral to call completion and amount of clinical experience of the chaplain.
Similar content being viewed by others
Introduction
As the first wave of COVID-19 swept the USA in March 2020 (CDC Museum COVID-19 Timeline, 2022), we noticed a change in medical provider distress and communication with the patient’s loved ones. It was our experience that most hospitalized patients with the disease were moderately or severely ill, often requiring ICU level care, where they were intubated, sedated, and prone, without loved ones at their side due to hospital visitor restrictions policy. The medical intensive care unit (MICU) unit chaplain observed moral distress in the medical providers, with a lack of knowledge about their patients identified as the prominent cause. Clinicians were called upon to provide care including times when they needed to make difficult decisions without knowing about the patient or having reliable access to their family. As Morley et al. (2021) describe this “feeling responsible for patients in a professional capacity as their designated nurse (provider) and also on a personal level” (p. 9). It was the personal level of distress that had been affected in the clinician without access to knowledge about the patient as a person.
During discussions, one provider noted, “…We care for humans, with whole human lives and relationships but it can be so hard to see that when someone is intubated, sedated with minimal visitors (for COVID or other reasons)” (Attending physician, personal communication, March 2020). Caring for the “whole human” without necessary details fosters stress and isolation, as Drummond and Carey (2020) describe COVID-19 challenged healthcare workers with a sense of guilt, anguish, helplessness, uncertainty, and powerlessness when one is fighting something on such a powerful scale with limited resources and no definite end in sight.
In response, a chaplain in the (MICU) at the Johns Hopkins Hospital (JHH) developed a program to interview and record loved ones of patients with communications limitations, about the patient as a person. This interview was edited to two minutes or less. The audio file was posted to the patient’s chart to enable the medical team to know them a bit better as a person and was referred to as This is My Story (TIMS). See the table for a graphic representation of the process of the interviews (Table 1).
Through the interview “finding common ground and common language can be helpful for both the medical team and the family” (Harris, 2018, p. 671). The chaplain was poised in this setting of distress because, “the potential of chaplaincy care to provide a spiritual balm for the patient’s distress and/ or the caregivers' disquietude lies in the chaplain’s willingness and ability to form a relationship with the care recipient, a task which involves both risk and vulnerability” (Cooper, 2018, p. 157). In this instance, the distress was being experienced by the providers as well as loved ones, and the chaplain’s ability to develop a relationship as a proxy with the family and then relay that information was vital to mitigating the distress. Notable levels of distress also arose from the provider's inability to fully be the patient’s advocate. As one provider describes, “I always feel a little protective of the family because you’re the patient's advocate, and they are in bed and can’t make decisions and you want to protect them and be there for them” (Morley et al., 2021, p. 157). The chaplain was able to step into this role of being the advocate and this helped manage experienced distress. Our approach was based upon knowledge gained in previously presented case studies (Tracey et al., 2021). As Morrison and Alvarez (2019) states, “all people have some sort of spiritual life that deeply impacts every area of their life, and that all people deserve access to quality spiritual care.” Although the aim of this study was not a directed spiritual intervention, having the chaplain as the interviewer provided a compassionate space for the interviewee to tell the story of their loved one. This spiritual or emotional care was not included in the audio file posted but was available to the loved one when needed.
This feasibility study aimed to determine if the TIMS interview would be reproducible by other experienced chaplains, those with four units or more of clinical pastoral education (CPE), and could be considered as a standard of care for chaplains in situations where a communication difficulty or visitor restriction occur. We approached the feasibility determination by looking at eight criteria: acceptability, demand, implementation, practicality, adaptation, integration, expansion, and limited-efficacy testing (Bowen et al., 2009). After completing this intervention for approximately 12 months, we found that it was feasible and that it met our rubric criteria well. Our Chaplaincy and Spiritual Care department could use it as another tool for providing care to patients/ loved ones and staff. For it to be feasible we desired to see a replicable interview process that would be requested by the providers on units as part of our standard of care and a cursory level assessment of the moral distress reduction that could be observed in the medical staff.
Methods
We based our interview on the development of TIMS in the MICU and developed a semi-structured interview for the loved ones of patients who are hospitalized in one of the participating units. We received approval from the Johns Hopkins Health System Institutional Review Board (Research Ethics Board) as an exempt determination, as this intervention was a survey and interview protocol where identifiable information would be kept as coded, and each subject was assigned a unique identifier and only two people would have access to the code that linked and once analysis was complete the code was destroyed. This study was able to proceed without written consent being obtained for the electronic medical record review to confirm eligibility or for the interview of the loved ones, however, we presented an information sheet before the discussions and requested verbal consent from the loved one. As the patient was unable to provide consent themselves, the loved one was considered their representative and if the patient regained capacity again, we would honor their choice to or not to participate in the study.
After consultation with legal counsel, there were specific safeguards in place to protect the privacy and confidentiality of the participants and their loved ones providing the interviews. Those performing the interview were acutely aware of the potential for sensitive information (e.g., abuse, illegal activities, self-harm, etc.) to be presented in the interview and monitored the recorded audio file for these details. If any of this information was presented the entire audio file was to be destroyed and not stored in the archive. If the risk of self-harm was presented, we had a two-pronged approach; for the patient, we could refer to the inhouse psychiatric services and for the loved ones we would refer them to a local provider.
From June 2020 through June 2021, the study team completed phone interviews with almost 200 adult patient loved ones from two urban, academic medical hospitals and across seven intensive care units and one medical step-down unit. Once the referral was made to the interviewing chaplains, the loved one was contacted by phone to get their consent to be interviewed and have the conversation recorded. The patient’s loved ones (emergency contacts) were chosen as they were the closest contact to the patient that we could conceivably speak with understanding that person’s story. This was not the optimal route in a few cases to use for contact since the person we spoke to only had a historical knowledge of the person, their childhood or early adulthood, but did not have current knowledge of the patient. However, with the patient not having the ability to direct who we contacted this was the most approachable route to complete interviews.
The semi-structured interview was developed in concert with the medical providers and unit chaplain to review and assess pertinent information that would be beneficial for everyone involved in care for the patient (Table 2). In some instances, this was used as a patient was having sedation withdrawn for reorientation or life support ended, they would be able to hear the voice of their loved one speaking with a message to them. We would ask the loved one what they would want to say to the patient if there were in front of them now, it also provided benefit to the clinicians as they could have a tangible reference to speak of during either of the two previous scenarios. Themes one and two were used as overall knowledge of the patient to help the providers to understand their passions or joys in life or circumstances that may have a bearing on medical care preferences. Themes three and four were for the benefit of the loved one being interviewed to allow them closure in what was often the death of the patient and in our experience, this allowed the medical providers to be more at peace with this death as they knew the loved ones were able to participate in the patient’s care. If there was a specific moment in the interview that the chaplain determined needed more discussion or care provided, they would return to this part, with the recording ending most of the time before this occurred. The conversation was ended with an offer to send a copy of the edited interview to the loved one to an email address they provided. No identifying information was included in the email text, only a brief appreciation for their time and the audio file that had names removed.
Once the interview was completed it was saved on HIPAA compliant digital storage and electronically sent to the Johns Hopkins School of Medicine students for editing. Each interview was edited from a typical 15–20 min in length into a file that was no more than 2 min in length. An ancillary outcome of this process was the opportunity for the medical students to hear and preserve a patient’s story. The students were guided through a brief training process of what to keep in the interview and what could be removed. Once edited, the interviewing chaplain listened to the file again to verify that the crucial portions of the conversation were included.
Posting the edited interview into the EMR required working with multiple teams from legal counsel, the electronic software development team, and marketing and communications. We were granted permission from our legal and privacy office to insert the audio file into the patient’s medical record as a temporary note that would self-delete once the patient was discharged. Once the link was connected to the chart, anyone on the medical team with access to the EMR could listen to the audio file. These audio files became an integral part of patient care rounds on participating clinical units at the hospital and could be accessed at any time by members of the medical care team through the EMR. A further look into the quantitative use of these files is being addressed in a follow-up study where staff use and impact are being specifically investigated.
For a participant to be included in this intervention they needed to meet three basic inclusion criteria: communication difficulty (e.g., intubation or capacity), length of stay 3 days or longer to allow a completed file to be posted, and visitation restrictions. Patients or loved ones who spoke languages other than English were accommodated with interpreters. The average turnaround time for recording the interview, editing, and posting to the EMR was approximately 2 days.
The patients selected for this study were at the request of a provider, unit administrator, or observation of the unit chaplain. All three sources of referral were aware of the inclusion criteria and only referred patients that satisfactorily met them. The approach for the interview was based upon grounded theory, as we developed our theory for distress mitigation or reduction for providers based upon our observations of them not being able to have a satisfactory level of knowledge of the patient. We began the intervention in conversations with the providers and continue to be more specific about the information that we glean from the patient’s loved ones (Koenig, 2011). In some cases, it is information that the provider had not initially thought to be useful but found to be helpful in their interactions with the patients and loved ones. One specific instance came from a nurse and in her comments, “I shared some of the information from the recording with the patient and he was nonverbal, but it put a big smile on his face” (Nurse, personal communication, May 2021). In these instances, for knowledge gained about the patient, in some instances without the capacity for consent, we left the determination and discretion to the medical providers on how or when to use these details for the most beneficial care of the patient. This is within our ethical approval as participants without the ability to consent were permitted to be enrolled. It also led to our goal of determining feasibility as we found the new utility of the intervention.
To better understand the practicality, integration, and efficacy testing we briefly interviewed the medical students that edited these audio files and the CPE students who initially performed the telephone interviews. For the medical students we asked them open-ended questions about their experience editing these audio files, what were the meaningful (personally and professionally) moments in this project, challenges they faced while participating and lastly how did this participation change their view of patients? The CPE students were less structured, and insights were assembled from their exit interview as they completed that specific unit of CPE. We didn’t specifically ask for the TIMS project to be addressed but as it was part of their learning objectives, to navigate methods for performing telechaplaincy, the end of unit comments reflected some of their insights.
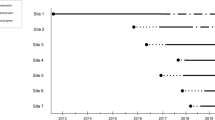
Site
The sites for this study were JHH, a level one trauma center with a 1,160-bed capacity, and Johns Hopkins Bayview Medical Center (BMC), a level 2 trauma center with a 420-bed capacity. At JHH, the study was conducted in the ICUs across approximately 84 beds: neurocritical critical care unit (NCCU), surgical ICU (SICU), and one medical step-down unit (MPCU). BMC utilized ICU locations as well as the burn ICU (BICU), medical ICU, cardiac ICU (CICU), and the neurocritical care unit (NCCU) with approximately 48 beds. Biocontainment protocols were in place and either no or severely restricted visitation was allowed.
Participant Population
After the patient’s eligibility was confirmed, the chaplain retrieved the emergency contact information from the EMR or through contact from one of the medical care providers. The study enrolled 387 subjects, average age of 60 years with ages ranging from 19 to 100 years. Adult subjects regardless of race or identified gender were included (Table 3). At the beginning of the interview with the loved one, they were given the option to decline participation and it was explained that the chaplain would still like to discuss their emotional or spiritual distress even if they didn’t choose to participate.
Staff
The staff conducting the audio interviews with the patient’s emergency contact varied throughout the year of data collection. Initially, CPE students were trained to make the calls as part of their ministry. It was later determined that it would be best practice to have a staff chaplain make the calls, based on experience as well as continuity.
Medical students were selected as editors, and it fulfilled two goals that at the time of the pandemic were not able to be achieved. The first was to provide them with experience with speaking to family members and obtaining valuable information for their care. This was incorporated into their educational outcomes for their academic learning. Second, as they were not able to be present on the medical unit, it allowed them to be an active participant in the patient’s care.
The recorded calls were specifically designed to further develop the loved one’s narrative of a hospitalized patient who is unable to relay this information themselves. It also provided reassurance to the family by reinstating social connectedness during their helpless situation of physical separation and consequent feelings of fear, anxiety, alienation, and abandonment. This loss of social connectedness was not a new phenomenon, as described by Drummond and Carey in their assessment of COVID-19’s overall impact. “The greatest reported impact has been in the social dimension. The loss of family contact and suspicion of fellow residents [those also hospitalized] being treated with droplet precautions has impacted feelings of connectedness and weakened relationships (Drummond & Carey, 2020).” It was in this social vacuum that the TIMS intervention was made and the connection to the social would help alleviate the provider's moral distress.
Results
Out of the 387 referrals received, 193 were completed, 15 died, 131 declined, 34 were discharged and 14 were discontinued as they moved to a non-ICU unit (Table 4). Once the call was made it would be categorized into one of five outcomes: completed, declined, discharged, discontinued, or death. Completed calls were completed within the three allotted attempts with an identified loved one.
Neither gender (p value = 0.343), race (p value = 0.925) nor age, in quartiles (p value = 0.837), was associated with the outcome of the interview. As displayed in Table 5, the participants were equally distributed among the potential categories. The most observed impact for death, discharge, and discontinuation was the speed at which the interview could be conducted from admission. If it was performed within 24 h of admission to the ICU it greatly increased the likelihood of it being posted. The average time between referral and first contact for calls with a completed outcome was 24 h. As for declining to participate, chaplain experience was the greatest factor. Interviews conducted with chaplains having completed four or more units of CPE had a 66% completion rate however, chaplains with two fewer units of CPE were completed at 33%.
Discussion
The idea of having recordings that included a loved one’s voice speaking about the patient is novel. Having the recording accessible to the medical team through the medical record was also innovative. This intervention was a result of previous experience of one of the study team’s experiences in patient advocacy through chaplaincy. The use of voice, particularly that of a loved one, was essential from the outset of the intervention. Other methods of conveying the information about the patient weren’t sufficient to convey emotion or practicable in the medical chart for wider distribution. As one provider explained, “It humanizes them incredibly, because you’re hearing a family member or friend talk about them in such an endearing way, more than if the patient were to tell you about themselves (Nurse, personal communication, June 2021).” In our discussions with the providers, listening to these audio files was a beneficial use of time where the resources such as time are limited and the applicability to the larger group, during rounds, was only available as an audio file.
Another value of the recorded narrative was that it was widely available to everyone who had access to the medical record. Any team member from any shift could listen, multiple times if they wished. Interpreters were used for non-English speakers. As noted by physicians at Brigham and Women’s Hospital, “Patients who didn't speak much, if any, English had a 35% greater chance of death during the initial phases of COVID-19 pandemic.” (Bebinger, 2021) This process allowed us to assist with the distress of the medical staff, again through the presentation of vital data about the patient as a person. Experience with electronic medical records and various other digital platforms was leveraged by several of the study team members.
The experience of staff chaplains conducting the interviews had a substantive impact on the completion rate of the interview and almost reduced by half the likelihood of a decline to participate. Our initial assessment is that it was linked to the number of CPE units that the chaplain had completed, where four or more units seemed to be the threshold. On our staff, five members had reached this marker among a CPE student in the 4th unit, three part-time (per diem) chaplains, and one unit chaplain. The initial assumption is that the completion of four units of CPE typically indicates pursuance of board certification (e.g., level II outcomes required) or at least a desire for a professional career in chaplaincy. Others that take CPE to meet ordination criteria or vocation exploration only take 1–2 units of CPE. The additional CPE units provide the student the avenue to reach what the certifying body references as “level II outcomes” which are required to pursue board certification. In the outcomes listed by the Association for Clinical Pastoral Education (ACPE), the one more pertinent to the success of this intervention is L2.3. It says the student must, “demonstrate a range of pastoral skills, including listening/attending, empathic reflection, conflict resolution/ transformation, confrontation, crisis management, and appropriate use of religious/spiritual resources” (Objectives and Outcomes for Level I/Level II CPE, 2022).
As TIMS has continued to be used in the hospital on ICU, step-down and other medical units we have only had chaplains that meet the four or more unit criteria conducting the interviews. Factors such as death, discharge, and discontinuation are beyond mitigation with chaplain experience. This discovery and implementation have led us to focus on the listening and interviewing skills of the chaplain as a predominant factor when selecting persons to do this function.
The participating students had varying levels of experience with hospital ministry and CPE. Of the six students, three were in their initial unit of CPE, two were in a second unit and the sixth student was in the fourth and final unit of CPE. The three experienced students had previously completed a unit of CPE with a prominent telechaplaincy component, due to the impacts of the COVID-19 pandemic on program design.
The six students expressed various levels of resistance to participating in the project. Several expressed that making phone calls to family members felt “invasive” and “disrespectful.” Two students, who immigrated to the USA as adults, expressed fears that they would be perceived as attempting to phish for information when they called patient family members. In addition, students struggled with the recording technology, even after additional training was provided.
Students also reported feeling disconnected from the TIMS project and expressed doubt that their recordings were utilized by the interdisciplinary care team. They reported mixed learning outcomes in their final self-evaluations. No student identified the TIMS project as a key source of learning during their CPE Unit. However, their educator noted that interns became more comfortable and more skilled in conducting interviews.
While we recognized that CPE students have generally less experience initiating a pastoral conversation, the overall context also had an impact. When the pandemic began, many CPE students and CPE faculty were seeking new ways to offer ministry during heightened anxiety and uncertainty, especially as the hospital’s policies around visitation tightened. This project was born under these strained conditions for both the hospital and the CPE program, and it propelled the current CPE group of interns into a new ministry format that they did not expect or plan to learn. In addition, making phone calls with a script was not easily translated into a chaplain approach for the CPE students, despite efforts to broaden their perspectives. These factors also likely contributed to the higher rate of decline than those of more experienced chaplains.
This intervention occurred during many of the student’s first unit of CPE and there is a preliminary lack of comfortability in asking direct questions, but as the educator observed, they became more comfortable as the unit progressed. Moving forward the pairing of a student with an experienced interviewer would be able to mitigate some of this anxiety for making the calls, and as explored previously more experience with providing care is also essential for comfortability. As for their doubt of use for the audio files, the use was tracked and evaluated, this is further discussed in the demand section on feasibility determination, and it was demonstrated that the files were being listen to by providers. However, a disconnect between students and providers existed because the students were not regularly rounding on the units during the initial phase of the pandemic. They were only speaking to patient, families, and providers via telephone or other electronic communications. They were not permitted to be involved with COVID-positive patients by the institution and this contributed to the lack of a feedback loop required for new interventions and their learning.
Five medical student editors were most closely involved in the program, and all five were interviewed regarding their experience. They all reported editing TIMS files as very valuable in helping them to view patients more holistically, as well as providing them with perspective on what living with chronic and/or serious illness is like. One fourth-year student was able to see how the medical team responded to TIMS files on the unit: “It was a pause, a moment when we could all focus on the person rather than the patient and the disease,” she says. “It’s about honoring that patient, that person who’s in front of you.”
Editors who weren’t on clinical rotations yet explained that they could see how TIMS files would increase both their empathy and compassion for patients and families. To describe TIMs, they used adjectives such as “meaningful,” “hopeful,” “nuanced,” and “revealing complexity.” All have agreed to continue editing in upcoming studies, with one editor confiding, “it was something I looked forward to.”
The data collected from the medical editors and CPE students were reviewed qualitatively and common themes or outcomes were grouped. Given the small number of participants (n = 11), this was not a particularly diverse or expansive sample and would only reflect those individuals who have already coalesced thought patterns as a functioning group before their introduction to the TIMS intervention. Additionally, as these responses were not anonymized the results may have been more positive than if they were able to respond freely.
As explored earlier in the introduction we used eight criteria to assess feasibility: acceptability, demand, implementation, practicality, adaptation, integration, expansion, and limited-efficacy testing. Admittedly, we also realize that, “The drawback of experimental feasibility studies is that they have relatively limited external validity” (Bowen et al., 2009, p. 4). The determination that this intervention is feasible and should proceed to a more rigorous examination and assessment has led to an incremental review of this study that has continued to progress with a review of the impact or effect on the perceived moral distress of staff and then is progressing to satisfaction with communication or psychiatric confounders with the loved ones.
Many of the feasibility criteria can be reviewed at a superficial level, however, they are individually being assessed in future explorations. Acceptability was most prominent in qualitative or anecdotal responses where the medical providers and loved ones provided positive affirmations of the intervention. The observed acceptedness was not always in the manner that we predicted but contributed in a small way to humanized patient care in the time when it seemed almost impossible with the tempo of the pandemic, one provider shared “as it gives me things to talk about with my intubated patients who can't tell me what they are interested in at home or like to do and it can help me pick a TV show to put on for my patient to watch, something they may find some interest in (Nurse, personal communication, June 2021).
Demand was looked at as we were able to track the use of the file; when and how many times providers clicked on the link to listen to the audio file and how long they listened. The timing of the use typically was based upon handoff, when the previous shift transfers care to the incoming provider. The participating chaplains also rounded with physicians and individually met with staff to discuss their use of the files.
Implementation of the TIMS intervention is the most widely looked at factor in this process, as we changed approaches many times in the early conducting of the study. As we expanded the intervention from one ICU to many and step-downs each unit required a slight alteration to make it more flexible to fit into the existing culture and workflow of the unit. The timing for posting the interview and introducing the staff to the intervention would be revised.
Practicality is another element that was changed quickly in the early implementation, the use of CPE students was found to not be effective and we needed to use experienced staff. This meant not only pivoting some of their current duties but having the financial ability for compensation for the additional hours worked. For units where there was not an adequate engagement, lack of interest from the providers, we discontinued use of the intervention on these units after the period for this study was concluded.
Adaptation was the primary catalyst for many of the changes made; change in personnel conducting the interview, which demographic information should be collected to be able to draw preliminary conclusions, how to introduce this to new units without disrupting their workflow, and logistical obstacles from typically performing 2–3 a week to now 10–15. Our population also shifted as we progressed into the step-down units. The participants were not always sedated, intubated, or prone but could speak for themselves. We did not interview them and continued to interview family members, as we didn’t want to distort our initial aim and we were exploring an interview with the patient in the next iteration of the study.
Integration posed the greatest initial complication however, once overcome it was conducted with greater ease than the other feasibility considerations. It was overcome by working with the other teams such as legal counsel and the EMR helpdesk support to understand the limitations and what could practicably be done to facilitate the interview posting and listening within these confines. The ability to pend a note in the EMR with an audio link caused practical issues, there is no hyperlink feature and only plain text, and other concerns such as a voice recording of a loved one in which legal counsel had concern for its ability to be continually accessed post-discharge. We were able to mitigate these with a few changes, largely the change for the chaplain was minimal as they now had a more structured discussion and it was recorded. Outside of their routine duties, they experienced few changes, as the editing and posting were done by two people on the study who have regular interactions with these processes.
Expansion is the impetus that began this formal investigation; the moving of an already successful, quasi-experimental, intervention of capturing someone’s story from one ICU to the other ICUs and step-down units. It was clear from our previous experience in the MICU that provider use and demonstrable need for this intervention would likely predict efficacy. The intervention in its current form is more useful in the ICU were limited to no communication with the patient or loved ones is present, however, future iterations are being investigated that could be presented to the patient themselves as a companion to the EMR data.
Limited-efficacy testing was the aim of this study as we used a convenience sample for participants and worked with medical providers that were well known to the unit chaplains. As such, we were also more interested in the overall outcomes and not specificity to deal with elements that might negate our limited statistical power.
With all eight of these criteria reviewed, the feasibility of this intervention has been determined. This perfunctory level investigation of the intervention warrants many deeper assessments into the many factors at hand in the recording and medical team use of the audio file. Those were not the aim of this study, as it was simply to see if it could be done amid an unprecedented shift in medical care and level of loved one’s interaction with decision making and discussions with providers.
Limitations
It was observed that units with less education and interaction with a TIMS representative were the least likely to use the intervention or provide referrals. This also led to a less productive discussion with the family member as most of the time was spent explaining how this was used in conjunction with current medical care and in a few instances, it was initially viewed as a criticism of the medical care being provided.
Because of the focused referral process, patient gender, race, and age may not have been representative of the unit’s demographic composition during the 12 months this study had been conducted.
Conclusion
Some of the positive ancillary outcomes from this study included capitalizing upon the listening and interviewing skills of a chaplain, teaching medical students to listen for key components of a person’s story, developing a model of outreach by phone, providing spiritual and emotional support to families who could not visit the hospital and providing an easily accessed audio file for the medical team to use in rounds and in their professional capacity. Ultimately, “the inclusion of the chaplain on the team becomes non-negotiable, and the provision of spiritual and religious care shifts to become a vital part of the overall plan of care” (Cooper, 2018).
The study team concludes that the intervention is feasible, based upon the criteria listed earlier, and that it has become a repeatable part of the spiritual care interventions that chaplains can utilize in instances when there is not an in-person mechanism for the patient’s loved ones to communicate with the medical providers. While there was limited-efficacy testing on the intervention, the initial assessment is that it can be implemented practically, adapting to changes in the institution, be integrated with the daily workflow, expanded into additional units/ settings, and will ultimately be requested by providers on units where this has not previously been available.
Data Availability
Available as requested.
References
Bebinger, M. (2021). The pandemic imperiled Non-English speakers in a hospital. NPR. Retrieved March 27, 2022, from https://www.npr.org/sections/health-shots/2021/04/23/989928262/the-pandemic-imperiled-non-english-speakers-in-a-hospital
Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., Bakken, S., Kaplan, C. P., Squiers, L., Fabrizio, C., & Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. https://doi.org/10.1016/j.amepre.2009.02.002
Centers for Disease Control and Prevention. (2022). CDC Museum Covid-19 Timeline. Centers for Disease Control and Prevention. Retrieved February 13, 2022, from https://www.cdc.gov/museum/timeline/covid19.html#:~:text=January%2020%2C%202020%20CDC,18%20in%20Washington%20state
Cooper, R. S. (2018). The palliative care chaplain as story catcher. Journal of Pain and Symptom Management, 55(1), 155–158. https://doi.org/10.1016/j.jpainsymman.2017.03.035
Drummond, D. A., & Carey, L. B. (2020). Chaplaincy and spiritual care response to COVID-19: An Australian case study – the McKellar centre. Health and Social Care Chaplaincy, 8(2), 165–179. https://doi.org/10.1558/hscc.41243
Harris, S. (2018). Chaplains’ roles as mediators in critical clinical decisions. AMA Journal of Ethics, 20(7), 670–674. https://doi.org/10.1001/amajethics.2018.670
Koenig, H. (2011). Spirituality & health research: methods, measurements. Templeton Press.
Morley, G., Bradbury-Jones, C., & Ives, J. (2021). The moral distress model: An empirically informed guide for moral distress interventions. Journal of Clinical Nursing. https://doi.org/10.1111/jocn.15988
Morrison, C. M., & Alvarez, A. (2019). The priority list: An evidence-based approach to selecting patients for chaplain visits. Journal of Pastoral Care and Counseling, 73(4), 238–243. https://doi.org/10.1177/1542305019890357
Objectives and Outcomes for Level I/Level II CPE. (2022). Retrieved from ACPE; The standard for spiritual care and education: https://www.manula.com/manuals/acpe/acpe-manuals/2016/en/topic/objectives-and-outcomes-for-level-i-level-ii-cpe
Tracey, E., Crowe, T., Wilson, J., Ponnala, J., Rodriguez-Hobbs, J., & Teague, P. (2021). An introduction to a novel intervention, “This is My Story”, to support interdisciplinary medical teams delivering care to non-communicative patients. Journal of Religion and Health, 60(5), 3282–3290. https://doi.org/10.1007/s10943-021-01379-3
Funding
Funding was received by Johns Hopkins COVID Relief Fund Grant Number ($50,000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have complied with all ethical standards in conducting this research and we have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilson, J., Tracey, E., Ponnala, J. et al. An ICU Expansion of a Novel Chaplain Intervention, “This is My Story,” to Support Interdisciplinary Medical Teams Delivering Care to Non-Communicative Patients in an Academic Medical Center. J Relig Health 62, 83–97 (2023). https://doi.org/10.1007/s10943-022-01567-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-022-01567-9