Abstract
Over the past few decades, research has suggested that cognitive variables play a key role in sleep disorders, particularly, in insomnia. The SLOC (Sleep Locus of Control Scale) evaluates the sleep locus of control, which is associated with the degree to which an individual attributes her/his experiences of sleep to chance or internal causes. The aim of this study was to develop the first translation and adaptation of the SLOC into the European Portuguese, as well as to analyze its psychometric properties. In this study, it was recruited a sample of 2029 Portuguese Higher Education students, aged ≥ 18 years, where approximately 75% of the sample were women and 25% men. The results showed that the SLOC had acceptable internal consistency value (α = .64), considering that it is a measure with a reduced number of items. As in the original study, a principal component analysis with varimax rotation identified two components. A parallel analysis was also conducted, identifying two factors. The correlation between the two subscales “internal sleep locus of control” and “chance sleep locus of control” was positive albeit of low magnitude (r = .15). Through the analysis carried out, it was also observed that individuals with “insomnia”, relative to those without, had a more chance sleep locus of control. Overall, these findings show similarities with the original study. The SLOC seems to be a useful psychological assessment measure to be used in clinical and research settings.
Similar content being viewed by others
Introduction
Within sleep disorders, insomnia is the most prevalent one. It is characterized by dissatisfaction with the quality of sleep, associated with difficulty in falling asleep and/or maintaining sleep for three or more nights in a week, for at least 3 months, and by significant impairment in day-to-day functioning. Insomnia is heterogeneous, having different durations, typologies, and etiologies, and can be defined as episodic, persistent, or recurrent (American Academy of Sleep Medicine [AASM], 2014; American Psychiatric Association [APA], 2014;Lichstein et al., 2017; Ong et al., 2017). Approximately one-third of adults report symptoms of insomnia and 6–10% have symptoms that fulfill the diagnosis of insomnia disorder (Chaput et al., 2017; Morin et al., 2011). It is more common in women, the elderly, and people with psychiatric or chronic illnesses (Vaughn & D’Cruz, 2017).
Regarding the diagnosis of insomnia, the main assessment method used is the comprehensive clinical interview, and it is also possible to use other complementary methods, such as self-report measures, sleep diaries, and actigraphy (Marques et al., 2018). Insomnia treatment can be psychological, pharmacological or both. Cognitive-behavioral therapies (CBT) are the first-line treatment for insomnia and focuses on the psychological, behavioral, and cognitive factors that maintain or exacerbate sleep disorders (Morin et al., 2017; Riemann et al., 2017). A recent clinical practice guideline (Buysse et al., 2017) recommended eszopiclone, zaleplon, zolpidem, triazolam, temazepam, and ramelteon for sleep-onset insomnia in adults. For sleep-maintenance insomnia, suvorexant, eszopiclone, zolpidem, temazepam, and doxepin were recommended. Of note, none of trazodone, tiagabine, diphenydramine, melatonin, tryptophan, or valerian were recommended for either type of insomnia.
There are several etiopathogenic models of insomnia. The 3P Model of Spielman is based on the interaction between three factors related to the etiology and maintenance of insomnia—predisposing factors, precipitating factors, and perpetuating factors (Spielman et al., 1987). In addition, the Microanalytic Model of Morin also refers to four categories of maintenance factors of insomnia: arousal, dysfunctional beliefs, maladaptive behavior, and consequences of insomnia. According to this model, the occurrence of an insomnia episode contributes to the development of cognitions and behaviors that prolong the insomnia episode and increase the probability of recurrence (Morin, 1993). The Cognitive Model of Harvey takes a more faithful approach to the classic cognitive theories of psychopathology and is centered on cognitive aspects of insomnia such as excessive negatively toned cognitive activity, arousal and distress, selective attention and monitoring, distorted perception, counterproductive safety behaviors, erroneous beliefs, and real deficit. This model considers that cognitive processes operating during the day and night equally contribute to the maintenance of insomnia (Harvey, 2002). Lastly, according to the Hybrid Cognitive-Behavioral Model of Lundh and Broman, insomnia is the result of an interaction between sleep-interfering processes and sleep-interpreting processes. Despite this distinction, the authors suggest that there is a bidirectional relationship between these two processes. Also, among the sleep-interfering processes, the attribution is highlighted (Lundh & Broman, 2000).
The cited models highlight cognitive factors as key aspects to consider in insomnia. The perception of control over sleep is one of these factors, and it can be operationalized through the concept of locus of control (LOC). The Social Learning Theory of Julian Rotter (1966) provides a theoretical basis for this concept. The locus of control is a psychological trait that determines the degree to which an individual understands what happens in life as a result of his actions. Rotter differentiates internal and external locus of control. When reinforcement is perceived by the individual as following some action of his own but not being entirely contingent upon his action (that is, reinforcement is perceived as the result of luck, chance, fate, under the control of powerful others, or as unpredictable), it represents a belief in external control. If the individual perceives that the event is contingent upon his own behavior or his own relatively permanent characteristics, is a belief in internal control. Locus of control is represented in a continuum with “internal” at one end and “external’ at the other (Rotter, 1966, 1975). Sleep can have an impact on the LOC orientation, as individuals who experience loss of sleep tend to exhibit, at an early stage, a more external locus of control, and with an improvement in the sleep quality, the internal locus of control tends to increase (Rucas & Miller, 2013; Vincent et al., 2010).
Considering the importance of locus of control related to sleep, Vincent et al. (2004) developed the “Sleep Locus of Control Scale”, composed by 8 items. The scale was validated through the study of two random samples, one composed of alumnae from the University of Manitoba (n = 425), and other composed of adults with chronic insomnia (n = 57). In this study, at a later stage, some of the insomnia group participants received cognitive behavioral treatment (CBT) for chronic insomnia and other received individual CBT for insomnia. According to the results, the SLOC showed acceptable internal consistency. Through the Principal Component Analysis (PCA) with varimax rotation, two components were found: “internal sleep locus of control” (items 1, 2, 5, 7, 8), and “chance sleep locus of control” (items 3, 4, 6). In the alumnae sample, the subscales showed a good internal consistency, with a Cronbach’s alpha of .73 and .59, respectively. For the insomnia sample, the subscales also showed a good internal consistency, with a Cronbach’s alpha of .62 and .47, respectively. An analysis of covariance procedure was used to examine whether groups differed on sleep locus of control, after controlling for age and gender, in which the results indicated that the insomnia group presented a great belief in chance sleep locus of control than did the alumnae group. Also, a logistic regression was conducted to assess whether the SLOC could discriminate between the two groups, and the results showed that both “internal sleep locus of control” and “age” significantly predicted group membership. The intercorrelation between the SLOC, SLOC factors, and other measures were also assessed, and the results showed that, in the insomnia sample, scores on the “internal” SLOC were significantly and positively associated with sleep-related anticipatory anxiety and a tendency to experience somatic symptoms. Also, in the alumnae sample, the reporting of depression or anxiety was significantly related to chance sleep locus of control. According to these results, the SLOC appears to be a potentially useful measure of expectations regarding the relationship between behavior and sleep.
SLOC has been used in some other studies. For example, in a study of Hantsoo et al. (2013) that had the purpose to identify predictors of pre-sleep arousal and trait hyperarousal from a set of variables that included the locus of control. The SLOC was used to assess this variable, which obtained a Cronbach’s alpha of .63.
Despite the paucity of studies on the SLOC until now, it seems to constitute an important measure for research and clinical practice, namely to offer hints for clinical intervention.
Hence, the current study aims to develop a European Portuguese version of the SLOC and to report the preliminary psychometric properties in a sample of Portuguese higher education students, including studies of reliability (internal consistency) and validity (convergent, criterion, and factor structure).
Methods
Participants
For this study, we collected a nonprobabilistic sample of 2029 higher education students. Participants were contacted via institutional e-mail or through social networks.
Participants were on average 24 years of age and were mostly women (75.4%), single (88.2%), pursuing a Bachelor’s degree (67.5%), from the areas of Sciences and Engineering and Social Sciences and Humanities, and full-time students (77.2%). Inclusion criteria included (1) attending a course in higher education, (2) having Portuguese nationality, and (3) voluntarily participating in the research (cf. Table 1).
Instruments
Sociodemographic Data. In order to characterize the sample, a sociodemographic sheet was prepared for the purposes of this study. Participants were asked about their age, sex, marital status, degree and field of study that they attended, and student status, which included the options “full-time student”, “working-student”, and “other”.
Self-reported insomnia. A self-reported question about insomnia was included (i.e., “Do you suffer from insomnia currently?”). This question has been used in several studies (e.g., Marques et al., 2021; Marques et al., 2016; Nóbrega et al., 2020).
Sleep Locus of Control Scale (SLOC) The Sleep Locus of Control Scale (Vincent et al., 2004; Portuguese adaptation: Marques et al., 2019) is a self-report instrument comprising 8 items, used to assess the sleep locus of control, which is associated with the degree to which an individual attributes her/his experiences of sleep to chance or internal causes. The SLOC is composed of two subscales, one that measures the “internal sleep locus of control” and other that measures the “chance sleep locus of control” (Vincent et al., 2004). The response scale may vary from strongly disagree (1) to strongly agree (6). Items 3, 4 and 6 are reversed. Total score may range from a minimum score of 8 and a maximum score of 48. Higher scores are associated with a more internal sleep locus of control, whereas lower scores are associated with a more chance sleep locus of control (Vincent et al., 2004).
Insomnia Severity Index (ISI) The ISI-PT is a brief self-report instrument used to measure insomnia and to estimate its severity (Bastien et al., 2001). This instrument is constituted by 7 items and the response scale ranges from 0 to 4. Total score may range from a minimum score of 0 and a maximum score of 28. Higher scores are associated with a greater severity of insomnia (Bastien et al., 2001; Morin, Belleville, et al., 2011; Morin, Leblanc, et al., 2011). For this study, the European Portuguese version by Clemente et al. (2021) was used and had acceptable internal consistency (Cronbach’s alpha = .83).
Glasgow Sleep Effort Scale (GSES). The GSES is a self-report measure used to assess sleep effort. The instrument comprises 7 items each associated with a component of the working model of sleep effort. The response scale covers the following options: not at all (0), to some extent (1), and very much (2), having as reference the sleep pattern over the last week. Total score may range from a minimum score of 0 to a maximum score of 14. Higher scores denote greater sleep effort (Broomfield & Espie, 2005). For this study, the European Portuguese version of the GSES was used (Meia-Via et al., 2016) achieving an acceptable internal consistency (Cronbach’s alpha = .77).
Hospital Anxiety and Depression Scale (HADS) The HADS is a brief self-report questionnaire used to measure anxiety and depression. This instrument is composed of two subscales, one that measures anxiety (HADS-A) with 7 items, and the other that measures depression (HADS-D) with 7 items. The two subscales are scored separately. The response scale ranges from 0 to 3, varying the options from item to item. Total score may range from a minimum score of 0 to a maximum score of 21, for each subscale (Zigmond & Snaith, 1983). For this study, the European Portuguese version of the HADS was used (Pais-Ribeiro et al., 2007), achieving an acceptable internal consistency (Cronbach’s alpha = .84 for the HADS-A, and .77 for the HADS-D).
Procedures
First, permission was requested to the original author of the SLOC for the translation and validation of the original scale into European Portuguese and to the Ethics and Deontology Committee (2019/No. 35) to obtain permission to conduct the study. Then, the instrument was translated by three researchers in the field of psychology. Subsequently, a consensual version was developed, having been reviewed by two external specialists with extensive experience in insomnia and adaptation of psychological assessment instruments.
Afterwards, the experimental version was applied to 20 individuals, of various age groups and education levels, through the “thinking aloud” method, in order to test whether the items were clear for the participants and check whether the participants had any suggestions. After some minor adjustments, a back-translation of the scale was performed by an independent translator without prior knowledge of the SLOC original version, and both were compared. No significant items modification was necessary. The final version was generated, which was labeled “Escala de Locus de Controlo do Sono” (SLOC).
Lastly, potential participants were invited to participate in the study through an email addressed to Higher Education institutions such as public and private Universities and Polytechnic Schools and through social networks (Facebook and Instagram). Informed consent was obtained on the homepage on the “FormsUA” online platform and the data was collected for about 1 month (28 February–30 March 2020). All participants voluntarily completed the online questionnaire, being aware that the data would be treated anonymously and confidentially. Since all the questions were mandatory, there were no missing values.
Data Analysis
All the data were analyzed using IBM SPSS Statistics v.26. Descriptive statistics such as mean, standard deviation, minimum, maximum and frequency were computed. To examine internal consistency of the measures, we calculated Cronbach’s alpha. For the SLOC, we also calculated mean and standard deviation for each item, item-total statistics and Cronbach’s alpha if item is excluded. Composite reliability was calculated, for which values equal to or greater than .7 are considered acceptable (Marôco, 2014; Raykov, 1997). Principal component analysis (PCA) with varimax rotation was also computed, along with an exploratory factor analysis with Principal Axis Factoring (PFA) using the program FACTOR (Ferrando & Lorenzo-Seva, 2017), which according to the literature is the most recommended program to perform a factor analysis (Cooper, 2018). For this procedure, we used a polychoric correlation matrix and Robust Diagonally Weighted Least Squares (RDWLS) extraction method (Asparouhov & Muthén, 2010). The number of factors was obtained through the Parallel Analysis method with random permutation of the observed data (Timmerman & Lorenzo-Seva, 2011) and the Normalized Varimax rotation was used. Pearson’s correlations matrices were calculated to study associations between the scales and subscales. The correlation effect sizes interpretation was based on Cohen’s guidelines: r = .1–.29 (small); r = .3–.49 (moderate); r = .5–1.0 (large). To explore differences between groups identifying as having “insomnia” and “no insomnia”, independent variables t-tests were performed. In order to prevent type I errors regarding multiple comparisons, Bonferroni corrections were applied. The effect size interpretation pertaining to differences between groups was based on Cohen’s guidelines: d = .2 (small); d = .5 (moderate); d = .8 (large) (Pallant, 2016).
Results
Descriptive statistics
Total mean score of the SLOC was 28.86 (SD = 5.07; Min. = 8; Max. = 48). For “internal sleep locus of control” subscale, the total mean score was 17.71 (SD = 3.94; Min. = 5; Max. = 30) and for “chance sleep locus of control” subscale was 11.15 (SD = 2.66; Min. = 3; Max. = 18). Pertaining to sex differences, total mean score for the SLOC for men was 30.19 (SD = 5.57) and for woman was 28.43 (SD = 4.82). This difference was statistically significant (t2027 = 6.83; p < .001; d = .34), although of low magnitude.
Total mean score of the ISI was 9.61 (SD = 5.30; Min. = 0; Max. = 27) which is in the sub-clinical range for insomnia. Regarding the GSES the total mean score was 4.83 (SD = 3.04; Min. = 0; Max. = 14). For the HADS-A, the total mean score was 8.36 (SD = 4.36); Min. = 0; Max. = 21), and for the HADS-D was 5.42 (SD = 3.58; Min. = 0; Max. = 18).
Pertaining to the insomnia self-reported item, approximately 31% of the participants answered “yes” and 69% answered “no”. It should be noted that the association of this self-reported insomnia question with the ISI cut-off groups was significant (χ2(1) = 558.472; p < .001; Cramer’s V = .526).
Reliability (Internal Consistency)
Through the inter-item correlation matrix, it was observed that the correlations had positive values, with some exceptions that would be expected according to the original study.
Cronbach’s alpha for total SLOC was .64. For “internal sleep locus of control” subscale, the Cronbach’s alpha was .70 and for “chance sleep locus of control” subscale was .52. Cronbach's alpha values are quite sensitive to the number of items, so in scales with a reduced number of items, it is common to observe low Cronbach's alpha values. Therefore, in these cases, it may be more suitable to report the average of the inter-item correlations (Pallant, 2016). Briggs and Cheek (1986) consider an optimum value between .2 and .4. In our study, the inter-item correlations mean was .18 for the SLOC, .32 for “internal sleep locus of control” and .28 for “chance sleep locus of control”. It was found that the exclusion of any item did not increase the level of internal consistency, except for item 5, although the difference is not substantial. The minimum corrected item-total correlation was .15 (item 5) and the maximum was .50 (item 8), as can be observed in Table 2.
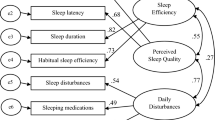
Structure of the SLOC
To examine the structure of the SLOC, it was verified if the data could be analyzed through a factor analysis using the Kaiser–Meyer–Olkin (KMO) value, which in this sample was .744 (> 06); the Bartlett’s sphericity test, which proved to be statistically significant (χ2(28) = 2446,661; p < .01); and the pattern of correlations (r), whose values were mostly higher than .30. In addition, the determinant value was .3 (> .00001), which indicates that there was no multicollinearity.
The results of PCA, as replicated from the original study, suggested a presence of two components according to the eigenvalue > 1 criterion, accounting for approximately 50% of the variance. Only component loadings ≥ .40 were extracted (Dancey & Reidy, 2017). The two components were labeled “internal sleep locus of control” (component I) and “chance sleep locus of control” (component II), as can be observed in Table 3.
Values above .70 are recommended (Marôco, 2014; Raykov, 1997) in the assessment of composite reliability. The values were .88 for the total SLOC score, .81 for the “internal sleep locus of control” component, which included 5 items, and .74 for the “chance sleep locus of control” component, which included 3 items.
The Exploratory Factor Analysis carried out using the Parallel Analysis method based on the “minimum rank factor analysis” and performed with normalized varimax rotation, constitutes a more rigorous and adequate technique to determine the number of factors when there are Likert-type items (Timmerman & Lorenzo-Seva, 2011). The results suggested a presence of two factors, which explained approximately 71% of the variance, as can be observed in Table 4.
It should be noted that when the “mean of random % of variance” table is considered, the results suggested a presence of two factors, which correspond to the “internal sleep control locus” (factor I) and the “chance sleep control locus” (factor II). However, when the “95 percentile of random % of variance” table is considered, the results suggested the presence of only one factor.
Regarding the composite reliability, the values obtained were .80 for the total SLOC score, .73 for the “internal sleep locus of control” factor, which included 5 items, and .58 for the “chance sleep locus of control” factor, which included 3 items.
Association Between SLOC, ISI, GSES, and HADS
Pearson’s correlation coefficients were calculated between total SLOC and its subscales, and ISI, GSES, HADS-A, and HADS-D. Overall, significant correlations were found between the variables. Specifically, regarding the correlation between SLOC and the other measures, the values were negative, except for the correlation between the two SLOC subscales, “Internal SLOC” and “Chance SLOC”. [The maximum value of correlation observed was between the SLOC and the “Internal SLOC” (r = .86, p < .001), and the minimum was between the “Internal SLOC” and the “Chance SLOC” (r = .15, p < .001)]. Table 5 shows the matrix of correlations between all variables.
Comparison of SLOC mean scores between groups (“insomnia” vs. “no insomnia”)
Considering the cut-off point of the ISI-PT version (> 14), two groups were created within the sample: “insomnia” (n = 481) and “sub-clinical or no insomnia” (n = 1548). Significant differences were found between groups, as can be observed in Table 6. The mean of the total SLOC score was 29.59 (SD = 4.80) for the group “sub-clinical or no insomnia”, which was indicative of a more internal sleep locus of control orientation, and 26.51 (SD = 5.20) for the “insomnia” Group. The difference between groups was significant, achieving a moderate effect size (t2027 = 12.06; p < .006; Cohen’s d = .62). All items showed significant differences with effect sizes ranging from small (items 2, 3, 6, 7, and 8) to moderate (items 1 and 4), except for item 5 which did not present a significant difference between both groups (cf. Table 6).
Discussion
The aim of this study was to adapt and validate the SLOC to the Portuguese population, and to study the preliminary properties of this version, using a large sample (n = 2029). The main finding of the study was that the SLOC seems to be an adequate measure of sleep locus of control that may be used either as unidimensional or bidimensional instrument. The internal consistency of the SLOC total score (α = .85), and subscales “internal SLOC” (α = .70) and “chance SLOC” (α = .52), were below the value recommended in the literature. However, when there are a small number of items in a scale, internal consistency can be quite low and it is recommended to report the mean inter-item correlations (Pallant, 2016). According to Briggs and Cheek (1986) criteria, the mean inter-item correlation values for SLOC total score (.18) and for the subscales “internal SLOC” (.32) and “chance SLOC” (.28) are indicative of a good internal consistency. These values are consistent with the original study (Vincent et al., 2004) and the study of Hantsoo et al. (2013).
The results showed that the number of factors comprising the SLOC depends on the analysis method. For example, there were two factors identified through a PCA with varimax rotation, and this is consistent with results from the original publication. Composite reliability was also calculated, which is a more accurate indicator of internal consistency. The composite reliability values for SLOC total score (.88) and for the subscales “internal SLOC” (.81) and “chance SLOC” (.74) are acceptable values and indicative of a good internal consistency. Additionally, there were two factors identified using EFA and the Parallel Analysis method (Timmerman & Lorenzo-Seva, 2011). Results suggest the presence of two factors if table “mean of random % of variance” is considered. However, if using the “95 percentile of random % of variance” the analysis suggests the presence of only one factor. Thus, there is evidence for the presence of one and two factors, depending on the criteria used, having both empirical support. A single factor model could be conceptualized on a continuum with “internal SLOC” and “chance SLOC” constituting the extremes.
Although PCA and EFA are two techniques with a similar objective of reducing a certain number of items to a smaller number of variables, they are based on different theoretical rationales. In this study, as expected, there was a higher factor loading of the items in the PCA compared to the EFA. Regarding the explained variance, it was expected that the components resulting from the PCA explained more variance than the factors resulting from EFA (Field, 2013), however this did not occur, since in the PCA the two components explained approximately 50% of the variance, while in the EFA the two factors explained approximately 71% of the variance.
The correlations between SLOC, ISI, GSES, and HADS support the convergent validity of the SLOC (Pallant, 2016). Overall, the correlations between SLOC and the other measures were negative and of small magnitude, albeit significant, according to Cohen's criteria (Pallant, 2016). Particularly, the correlation between the subscales “chance SLOC” and “internal SLOC” was positive, but of small magnitude (r = .15). These results may indicate that the two factors that compose the subscales are relatively independent. These findings, along with the low value of internal consistency, may indicate that it would be more suitable to rate the two subscales separately. In the original study (Vincent et al., 2004), the two subscales also showed a correlation of small magnitude (r = .22).
Through the comparison of SLOC mean scores between groups (“insomnia” vs. “sub-clinical or no insomnia”) it was found that the two subscales “internal SLOC” and “chance SLOC” have a moderate, and relatively equivalent, magnitude of effect (d = .47 and d = .48). For the total SLOC, the difference between both groups was statistically significant, with a moderate effect size (d = .62). To note that within each group the mean values are higher for the "sub-clinical or no insomnia" group compared to the “insomnia” group. That means that “insomnia” group has a higher level of external sleep locus of control which is in line with other studies (Vincent et al., 2004, 2010). As suggested by Rucas and Miller (2013), sleep can influence the orientation of locus of control, as individuals with sleep problems tend to exhibit, at an early stage, a more chance locus of control. This is in line with the result obtained, in which individuals with insomnia scored, on average, lower on the full scale SLOC, which is associated with a more chance sleep locus of control.
Although the results found are encouraging, some limitations must be outlined. One of the limitations of this study is that it was used an online investigation protocol, which despite the advantages associated, has some disadvantages such as difficulty in controlling the study, possible multiple submissions, and larger incomplete submissions (Ramos & Leal, 2019). Also, a sample composed of higher education students was used, which is not representative of the entire population. However, it is noteworthy that the experimental version was applied to individuals of various age groups and education levels, through the “thinking aloud” method, and no significant comprehension problems were detected. Plus, the translations were reviewed by experts with extensive clinical experience in the field of sleep medicine, who ensured the understanding of the SLOC for the general population. Other limitation was that the constitution of the “insomnia” and “sub-clinical or no insomnia” groups was based on a self-report measure, not on a clinical diagnosis. However, several authors use this method, placing in the “clinical group” those who score above a certain cut-off point on a clinical scale, since this group will eventually include individuals with the disorder or with a tendency to develop it (Marques et al., 2021). It is also important to take into account the fact that during the data collection period was declared a state of emergency in Portugal due to the Coronavirus (SARS-CoV-2) pandemic. The pandemic, the social distancing imposed, and the associated stress and anxiety may have led to an increase of sleep disorders (Morin et al., 2020). This may have had an impact on the proportion of individuals with insomnia in this sample and on the reporting of chance SLOC. Finally, the difficulty in the comparison process related to the SLOC, since there were few international studies, was also a limitation.
For future studies, it would be pertinent to perform a stability test (test–retest). It also would be pertinent to explore other psychometric properties, like perform a factor analysis with other samples and a confirmatory factor analysis, in order to confirm the factors extracted from the analysis (Pallant, 2016). Replicating the study with a clinical sample, other sleep disorders, and other community samples would also be interesting. Finally, the use of item response theory analysis, for example, may be relevant to verify which items are more informative.
In conclusion, the findings from the current study suggest that the Portuguese version of the SLOC has adequate psychometric properties. Thus, it seems to be a useful measure for clinical practice and for research in the field of sleep psychology in Portugal.
References
American Psychiatric Association. (2014). Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). American Psychiatric Association Publishing.
American Academy of Sleep Medicine. (2014). International classification of sleep disorders: diagnostic and coding manual (3rd ed.). One Westbrook Corporate Center.
Asparouhov, T., & Muthén, B. (2010). Simple second order chi-square correction. Statmodel. http://www.statmodel.com/download/WLSMV_new_chi21.pdf
Bastien, C. H., Vallières, A., & Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. https://doi.org/10.1016/S1389-9457(00)00065-4
Briggs, S. R., & Cheek, J. M. (1986). The role of factor analysis in the development and evaluation of personality scales. Journal of Personality, 54(1), 106–148. https://doi.org/10.1111/j.1467-6494.1986.tb00391.x
Broomfield, N. M., & Espie, C. A. (2005). Towards a valid, reliable measure of sleep effort. Journal of Sleep Research, 14(4), 401–407. https://doi.org/10.1111/j.1365-2869.2005.00481.x
Buysse, D., & Harvey, A. (2017). Insomnia: Recent developments and future directions. In M. Kryger, T. Roth, & W. Dement (Eds.), Principles and practice of sleep medicine (6th ed., pp. 757–760). Elsevier.
Chaput, J. P., Wong, S. L., & Michaud, I. (2017). Duration and quality of sleep among Canadians aged 18–79. Health Reports, 28(9), 28–33.
Clemente, V., Marques, D., Miller-Mendes, M., Morin, C. M., Serra, J., & Allen Gomes, A. (2021). The European Portuguese version of the insomnia severity index. Journal of Sleep Research, 30(1), e13198. https://doi.org/10.1111/jsr.13198
Cooper, C. (2018). Psychological testing: Theory and practice. Routledge.
Dancey, C., & Reidy, J. (2017). Statistics without maths for psychology (7th ed.). Pearson Education Limited.
Ferrando, P. J., & Lorenzo-Seva, U. (2017). Program FACTOR at 10: Origins, development and future directions. Psicothema, 29(2), 236–241. https://doi.org/10.7334/psicothema2016.304
Field, A. (2013). Discovering statistics using IBM SPSS Statistics (4th ed.). SAGE Publications.
Hantsoo, L., Khou, C. S., White, C. N., & Ong, J. C. (2013). Gender and cognitive–emotional factors as predictors of pre-sleep arousal and trait hyperarousal in insomnia. Journal of Psychosomatic Research, 74(4), 283–289. https://doi.org/10.1016/j.jpsychores.2013.01.014
Harvey, A. G. (2002). A cognitive model of insomnia. Behaviour Research and Therapy, 40(8), 869–893. https://doi.org/10.1016/S0005-7967(01)00061-4
Lichstein, K., Taylor, D., McCrae, C., & Petrov, M. (2017). Insomnia: Epidemiology and risk factors. In M. Kryger, T. Roth, & W. Dement (Eds.), Principles and practice of sleep medicine (6th ed., pp. 761–768). Elsevier.
Lundh, L. G., & Broman, J. E. (2000). Insomnia as an interaction between sleep-interfering and sleep-interpreting processes. Journal of Psychosomatic Research, 49(5), 299–310. https://doi.org/10.1016/S0022-3999(00)00150-1
Marôco, J. (2014). Análise de equações estruturais: Fundamentos teóricos, software & aplicações (2ª ed.). ReportNumber.
Marques, D., Clemente, V., Gomes, A., & Azevedo, M. H. (2018). Profiling insomnia using subjective measures: Where are we and where are we going. Sleep Medicine, 43, 103–104. https://doi.org/10.1016/j.sleep.2017.12.006
Marques, D. R., Gomes, A. A., & Azevedo, M. H. P. (2021). Utility of studies in community based populations. Sleep and Vigilance, 5, 161–162. https://doi.org/10.1007/s41782-021-00135-7
Marques, D., Gomes, A., Ferreira, M., & Azevedo, M. H. (2016). Don’t worry, sleep well: Predictors of sleep loss over worry. Sleep and Biological Rhythms, 14(3), 309–318. https://doi.org/10.1007/s41105-016-0060-z
Marques, D., Vieira, P., & Silva, J. (2019). Escala do locus de controlo do sono (SLOC). Universidade de Aveiro.
Meia-Via, M. S., Marques, D. R., Espie, C. A., Silva, C. F., & Gomes, A. A. (2016). Psychometric properties of Glasgow sleep effort scale in portuguese language. Psychological Assessment, 28(3), e12–e18. https://doi.org/10.1037/pas0000178
Morin, C. (1993). Insomnia: Psychological assessment and management. The Guilford Press.
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. https://doi.org/10.1093/sleep/34.5.601
Morin, C. M., Carrier, J., Bastien, C., & Godbout, R. (2020). Sleep and circadian rhythm in response to the COVID-19 pandemic. Canadian Journal of Public Health, 111(5), 654–657. https://doi.org/10.17269/s41997-020-00382-7
Morin, C. M., Davidson, J. R., & Beaulieu-Bonneau, S. (2017). Cognitive behavior therapies for insomnia I: Approaches and efficacy. In M. Kryger, T. Roth, & W. Dement (Eds.), Principles and practice of sleep medicine (6th ed., pp. 804–813). Elsevier.
Morin, C. M., Leblanc, M., Bélanger, L., Ivers, H., Mérette, C., & Savard, J. (2011). Prevalence of insomnia and its treatment in Canada. The Canadian Journal of Psychiatry, 56(9), 540–548. https://doi.org/10.1177/070674371105600905
Nóbrega, C., Correia, A. L., Gomes, A., Azevedo, M. H., & Marques, D. (2020). European Portuguese validation of the thought control questionnaire insomnia-revised (TCQI-R). Journal of Rational-Emotive Cognitive-Behavior Therapy, 39, 355–374. https://doi.org/10.1007/s10942-020-00377-w
Ong, J., Arnedt, J. T., & Gehrman, P. (2017). Insomnia diagnosis, assessment, and evaluation. In M. Kryger, T. Roth, & W. Dement (Eds.), Principles and practice of sleep medicine (6th ed., pp. 785–793). Elsevier.
Pais-Ribeiro, J., Silva, I., Ferreira, T., Martins, A., Meneses, R., & Baltar, M. (2007). Validation study of a Portuguese version of the hospital anxiety and depression scale. Psychology, Health & Medicine, 12(2), 225–235. https://doi.org/10.1080/13548500500524088
Pallant, J. (2016). SPSS survival manual (6th ed.). McGraw-Hill Education.
Ramos, M. M., & Leal, I. (2019). Protocolos de investigação online: Vantagens e desvantagens. In I. Patrão & I. Leal (Eds.), Intervenção em Ciberpsicologia (pp. 3–15). PACTOR.
Raykov, T. (1997). Estimation of composite reliability for congeneric measures. Applied Psychological Measurement, 21(2), 173–184. https://doi.org/10.1177/01466216970212006
Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Groselj, L. D., Ellis, J. G., Espie, C. A., Garcia-Borreguero, D., Gjerstad, M., Gonçalves, M., Hertenstein, E., Jansson-Fröjmark, M., Jennum, P. J., Leger, D., Nissen, C., Parrino, L., Paunio, T., Pevernagie, D., Verbraecken, J., & Spiegelhalder, K. (2017). European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research, 26(6), 675–700. https://doi.org/10.1111/jsr.12594
Rotter, J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied, 80(1), 1–28. https://doi.org/10.1037/h0092976
Rotter, J. B. (1975). Some problems and misconceptions related to the construct of internal versus external control of reinforcement. Journal of Consulting and Clinical Psychology, 43(1), 56–67. https://doi.org/10.1037/h0076301
Rucas, S. L., & Miller, A. A. (2013). Locus of control and sleep in evolutionary perspective. Journal of Social, Evolutionary, and Cultural Psychology, 7(2), 79–96. https://doi.org/10.1037/h0099208
Spielman, A. J., Caruso, L. S., & Glovinsky, P. B. (1987). A behavioral perspective on insomnia treatment. Psychiatric Clinics of North America, 10(4), 541–553. https://doi.org/10.1016/s0193-953x(18)30532-x
Timmerman, M. E., & Lorenzo-Seva, U. (2011). Dimensionality assessment of ordered polytomous items with parallel analysis. Psychological Methods, 16(2), 209–220. https://doi.org/10.1037/a0023353
Vaughn, B. V., & D’Cruz, O. F. (2017). Cardinal manifestations of sleep disorders. In M. Kryger, T. Roth, & W. Dement (Eds.), Principles and practice of sleep medicine (6th ed., pp. 576–586). Elsevier.
Vincent, N., Sande, G., Read, C., & Giannuzzi, T. (2004). Sleep locus of control: Report on a new scale. Behavioral Sleep Medicine, 2(2), 79–93. https://doi.org/10.1207/s15402010bsm0202_1
Vincent, N., Walsh, K., & Lewycky, S. (2010). Sleep locus of control and computerized cognitive-behavioral therapy (cCBT). Behaviour Research and Therapy, 48(8), 779–783. https://doi.org/10.1016/j.brat.2010.05.006
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Acknowledgements
The authors would like to thank all the students who participated in the study.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vieira, P., Silva, J., Gomes, A.A. et al. Psychometric Properties of the Sleep Locus of Control (SLOC) Scale in a Portuguese Sample. J Rat-Emo Cognitive-Behav Ther 41, 193–208 (2023). https://doi.org/10.1007/s10942-022-00462-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10942-022-00462-2