Abstract
After the onset of the COVID-19 pandemic in 2020, Asian Americans in the United States have experienced a surge in anti-Asian crimes, leading to heightened psychological distress among this community. Consequently, the mental well-being of Asian Americans demands greater attention than ever. Regrettably, Asians tend to underutilize or delayed mental health care treatments. This study examines the conventional and alternative mental health service utilization among Asians in the United States according to their English proficiency. From the 2015–2018 National Survey on Drug Use and Health, this study examined 3,424 self-identified non-Hispanic Asians aged 18–64 with Kessler score of at least 5. Stratified bivariate analysis and multivariable logistic regression analysis were conducted. Regardless of English proficiency, Asians did not utilize alternative mental health service more than conventional mental health service. However, those with limited English proficiency consistently utilize care less than those with English proficiency. Need factors, such as mental distress severity and self-rated health status, were significant factors associated with their mental health service utilization. English proficiency remains a structural factor in preventing Asians from utilizing mental health services regardless of the nature of services. Due to the COVID-19 pandemic, more Asians have been experiencing mental distress. This study demonstrates a particular need for mental health services that are culturally specific and Asian language friendly.
Similar content being viewed by others
Notes
Asians are defined as individuals having origins in Asia. They might be U.S. citizens, permanent residents, or undocumented. Due to the nature of these attacks, some might not have origins in Asia, but were attacked due to their Asian-like appearance.
References
Dhanani LY, Franz B. Unexpected public health consequences of the COVID-19 pandemic: a national survey examining anti-asian attitudes in the USA. Int J Public Health. 2020;65(6):747–54. https://doi.org/10.1007/s00038-020-01440-0.
Wu C, Qian Y, Wilkes R. Anti-asian discrimination and the asian-white mental health gap during COVID-19. Ethnic and Racial Studies. 2021;44(5):819–35. https://doi.org/10.1080/01419870.2020.1851739.
Cheah CSL, Wang C, Ren H, Zong X, Cho HS, Xue X. COVID-19 racism and Mental Health in chinese american families. Pediatrics. 2020;146(5). https://doi.org/10.1542/peds.2020-021816.
Lee S, Waters SF. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: impacts on health outcomes and the buffering role of social support. Stigma and Health. 2021;6(1):70–8. https://doi.org/10.1037/sah0000275.
Ali MM, Lackey S, Mutter R, McKeon R. The Relationship between Perceived Unmet Mental Health Care needs and suicidal ideation and attempt. Adm Policy Mental Health Mental Health Serv Res. 2018;45(5):709–15. https://doi.org/10.1007/s10488-018-0856-z.
Abe-Kim J, Takeuchi DT, Hong S, et al. Use of Mental Health–Related Services among immigrant and US-Born asian Americans: results from the national latino and asian american study. Am J Public Health. 2007;97(1):91–8. https://doi.org/10.2105/AJPH.2006.098541.
Le Meyer O, Zane N, Cho YI, Takeuchi DT. Use of Specialty Mental Health Services by Asian Americans with Psychiatric Disorders. J Consult Clin Psychol. 2009;77(5):1000–5. https://doi.org/10.1037/a0017065.
Lee S, Matejkowski J. Mental health service utilization among noncitizens in the United States: findings from the national latino and asian american study. Adm Policy Ment Health. 2012;39(5):406–18. https://doi.org/10.1007/s10488-011-0366-8.
Augsberger A, Yeung A, Dougher M, Hahm HC. Factors influencing the underutilization of mental health services among asian american women with a history of depression and suicide. BMC Health Serv Res. 2015;15(1):542. https://doi.org/10.1186/s12913-015-1191-7.
Jang Y, Kim MT. Limited English proficiency and Health Service Use in Asian Americans. J Immigr Minor Health. 2019;21(2):264–70. https://doi.org/10.1007/s10903-018-0763-0.
Montemitro C, D’Andrea G, Cesa F, et al. Language proficiency and mental disorders among migrants: a systematic review. Eur Psychiatry. 2021;64(1):e49. https://doi.org/10.1192/j.eurpsy.2021.2224.
Derr AS. Mental Health Service Use among Immigrants in the United States: a systematic review. Psychiatr Serv. 2016;67(3):265–74. https://doi.org/10.1176/appi.ps.201500004.
Kim G, Aguado Loi CX, Chiriboga DA, Jang Y, Parmelee P, Allen RS. Limited English proficiency as a barrier to mental health service use: a study of latino and asian immigrants with psychiatric disorders. J Psychiatr Res. 2011;45(1):104–10. https://doi.org/10.1016/j.jpsychires.2010.04.031.
Kleinman A. Culture and Depression. N Engl J Med. 2004;351(10):951–3.
Ryder AG, Yang J, Zhu X, et al. The cultural shaping of depression: somatic symptoms in China, psychological symptoms in North America? J Abnorm Psychol. 2008;117(2):300–13. https://doi.org/10.1037/0021-843X.117.2.300.
Ryder AG, Chentsova-Dutton YE. Depression in Cultural Context: chinese somatization. Revisit Psychiatric Clin North Am. 2012;35(1):15–36. https://doi.org/10.1016/j.psc.2011.11.006.
Ran MS, Hall BJ, Su TT, et al. Stigma of mental illness and cultural factors in Pacific Rim region: a systematic review. BMC Psychiatry. 2021;21(1):8. https://doi.org/10.1186/s12888-020-02991-5.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: an integrative review. Clin Psychol Rev. 2011;31(6):934–48. https://doi.org/10.1016/j.cpr.2011.05.003.
Ng CH. The stigma of mental illness in asian cultures. Aust N Z J Psychiatry. 1997;31(3):382–90. https://doi.org/10.3109/00048679709073848.
Park J, Lee EJ, Barker K, et al. Mental illness identity development and service utilization experiences among asian Americans with mental illness: a qualitative study. Psychiatr Rehabil J. 2023;46(1):36–44. https://doi.org/10.1037/prj0000557.
Kalibatseva Z, Leong FTL. Depression among Asian Americans: Review and Recommendations. Depress Res Treat. 2011;2011. https://doi.org/10.1155/2011/320902.
National Cancer Institute. Complementary and Alternative Medicine. Published online 2021. https://www.cancer.gov/about-cancer/treatment/cam.
Rhee TG, Evans RL, McAlpine DD, Johnson PJ. Racial/Ethnic differences in the Use of complementary and alternative medicine in US adults with Moderate Mental Distress. J Prim Care Community Health. 2017;8(2):43–54. https://doi.org/10.1177/2150131916671229.
Zhu L, Complementary, Alternative Medical Service Use for Mental Health Problems among Chinese Americans. The Roles of Acculturation-related factors. Soc Mental Health. 2019;9(3):366–87. https://doi.org/10.1177/2156869318804304.
Andersen R, Davidson P. Changing in the U.S. health care system: Key issues in health services policy and management. In: IMPROVING ACCESS TO CARE IN AMERICA Individual and Contextual Indicators. Jossey-Bass; 2007. Accessed December 20, 2020. https://www.academia.edu/14385102/IMPROVING_ACCESS_TO_CARE_IN_AMERICA_Individual_and_Contextual_Indicators.
Aday LA, Andersen R. A Framework for the study of Access to Medical Care. Health Serv Res. 1974;9(3):208–20.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of Health Services Use: a systematic review of studies from 1998–2011. Psychosoc Med. 2012;9. https://doi.org/10.3205/psm000089.
Chen AW, Kazanjian A, Wong H. Determinants of mental health consultations among recent chinese immigrants in British Columbia, Canada: implications for mental health risk and access to services. J Immigr Minor Health. 2008;10(6):529–40. https://doi.org/10.1007/s10903-008-9143-5.
Kang SY, Howard D, Kim J, et al. English language proficiency and lifetime mental health service utilization in a national representative sample of Asian Americans in the USA. J Public Health. 2010;32(3):431–9. https://doi.org/10.1093/pubmed/fdq010.
Derr AS. Mental Health Service Use among Immigrants in the United States: a systematic review. PS. 2015;67(3):265–74. https://doi.org/10.1176/appi.ps.201500004.
Bauer AM, Alegría M. Impact of Patient Language Proficiency and Interpreter Service Use on the quality of Psychiatric Care: a systematic review. PS. 2010;61(8):765–73. https://doi.org/10.1176/ps.2010.61.8.765.
Sentell T, Shumway M, Snowden L. Access to Mental Health treatment by English Language proficiency and Race/Ethnicity. J Gen Intern Med. 2007;2(22):289–93. https://doi.org/10.1007/s11606-007-0345-7.
Yang KG, Rodgers CRR, Lee E, Lê Cook B. Disparities in Mental Health Care utilization and Perceived need among Asian Americans: 2012–2016. PS. 2019;71(1):21–7. https://doi.org/10.1176/appi.ps.201900126.
United States Census Bureau. About Language Use in the U.S. Population. Published online 2021.
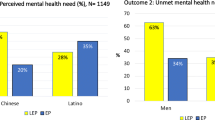
Garcia ME, Hinton L, Gregorich SE, Livaudais-Toman J, Kaplan C, Karliner L. Unmet Mental Health need among chinese and latino primary care patients: intersection of ethnicity, gender, and English proficiency. J Gen Intern Med. 2020;35(4):1245–51. https://doi.org/10.1007/s11606-019-05483-9.
Zhang X, Martinez-Donate AP, Kuo D, Jones NR. How is smoking handled in your home?: agreement between parental reports on home smoking bans in the United States, 1995–2007. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2012;14(10):1170–9. https://doi.org/10.1093/ntr/nts005.
Eng DK, TenElshof JK. Addressing the Stigma Associated with seeking help for Mental Health among Asian Americans. J Psychol Christianity. 2020;39(2):125–33.
Lee SY, Xue Q, li, Spira AP, Lee HB. Racial and ethnic differences in depressive subtypes and access to mental health care in the United States. J Affect Disord. 2014;155:130–7. https://doi.org/10.1016/j.jad.2013.10.037.
Chen P, Hussey JM, Monbureau TO. Depression and Antidepressant Use among Asian and hispanic adults: association with immigrant Generation and Language Use. J Immigr Minor Health. 2018;20(3):619–31. https://doi.org/10.1007/s10903-017-0597-1.
Li HZ, Browne AJ. Defining mental illness and accessing mental health services: perspectives of asian Canadians. Can J Commun Ment Health. 2000;19(1):143–59. https://doi.org/10.7870/cjcmh-2000-0008.
Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health Public Use file codebook. Substance Abuse and Mental Health Services Administration; 2018.
Center for Behavioral Health Statistics and Quality. 2018 National Survey on Drug Use and Health Public Use file codebook. Substance Abuse and Mental Health Services Administration; 2019.
Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health Public Use file codebook. Substance Abuse and Mental Health Services Administration; 2018.
Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health Public Use file codebook. Substance Abuse and Mental Health Services Administration; 2018.
Kessler RC, Green JG, Gruber MJ, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22. https://doi.org/10.1002/mpr.310.
Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9. https://doi.org/10.1001/archpsyc.60.2.184.
Prochaska JJ, Sung H, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21(2):88–97. https://doi.org/10.1002/mpr.1349.
Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357–62. https://doi.org/10.1017/s0033291702006700.
Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76. https://doi.org/10.1017/s0033291702006074.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59. https://doi.org/10.1016/j.genhosppsych.2010.03.006.
R Core Team. R: A Language and Environment for Statistical Computing. Published online 2020. https://www.R-project.org/.
Nahas R, Sheikh O. Complementary and alternative medicine for the treatment of major depressive disorder. Can Fam Physician. 2011;57(6):659–63.
Rethorst CD, Trivedi MH. Evidence-based recommendations for the prescription of Exercise for Major Depressive Disorder. J Psychiatric Practice®. 2013;19(3):204. https://doi.org/10.1097/01.pra.0000430504.16952.3e.
Trkulja V, Barić H. Current research on complementary and alternative medicine (CAM) in the treatment of major depressive disorder: an evidence-based review. In: Kim YK, editor. Major depressive disorder: rethinking and understanding recent discoveries. Advances in Experimental Medicine and Biology. Springer; 2021. pp. 375–427. https://doi.org/10.1007/978-981-33-6044-0_20.
Pierce BS. The COVID-19 telepsychology revolution: a national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. 20200820;76(1):14. https://doi.org/10.1037/amp0000722.
Benjamen J, Girard V, Jamani S, et al. Access to Refugee and migrant Mental Health Care Services during the First Six months of the COVID-19 pandemic: a canadian Refugee Clinician Survey. Int J Environ Res Public Health. 2021;18(10):5266. https://doi.org/10.3390/ijerph18105266.
Iwamoto DK, Liao L, Liu WM. Masculine norms, avoidant coping, asian values, and depression among asian american men. Psychol Men Masculinity. 2010;11(1):15–24. https://doi.org/10.1037/a0017874.
Nam SK, Chu HJ, Lee MK, Lee JH, Kim N, Lee SM. A meta-analysis of gender differences in attitudes toward seeking professional psychological help. J Am Coll Health. 2010;59(2):110–6. https://doi.org/10.1080/07448481.2010.483714.
Manuel JI. Racial/Ethnic and gender disparities in Health Care Use and Access. Health Serv Res. 2018;53(3):1407–29. https://doi.org/10.1111/1475-6773.12705.
Gagné S, Vasiliadis HM, Préville M. Gender differences in general and specialty outpatient mental health service use for depression. BMC Psychiatry. 2014;14(1):135. https://doi.org/10.1186/1471-244X-14-135.
Sue S, Yan Cheng JK, Saad CS, Chu JP. Asian american mental health: a call to action. Am Psychol. 2012;67(7):532–44. https://doi.org/10.1037/a0028900.
Kuroki Y. Comparison of suicide Rates among Asian Americans in 2000 and 2010. Omega (Westport). 2018;77(4):404–11. https://doi.org/10.1177/0030222816678425.
Twenge JM, Joiner TE. Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol. 2020;76(12):2170–82. https://doi.org/10.1002/jclp.23064.
Rose N, Manning N, Bentall R, et al. The social underpinnings of mental distress in the time of COVID-19 – time for urgent action. Wellcome Open Res. 2020;5:166. https://doi.org/10.12688/wellcomeopenres.16123.1.
Jacoby A, Li Y. Mental Health Care Access and individual help-seeking during the Covid-19 pandemic. Community Ment Health J. 2022;58(8):1572–83. https://doi.org/10.1007/s10597-022-00973-3.
Nguyen D, Lee R. Asian immigrants’ mental health service use: an application of the life course perspective. Asian Am J Psychol. 2012;3(1):53–63. https://doi.org/10.1037/a0026865.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Aliya Kuerban contributes to conception, design of the study, analysis, interpretation of data, drafting the manuscript. Jin Young Seo contributes to revising the draft critically for important intellectual content and adding key discussion components. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The Molloy College IRB has determined this project is EXEMPT FROM IRB REVIEW according to federal regulations due to the study nature of secondary data analysis of publically available data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuerban, A., Seo, J.Y. Conventional or Alternative Mental Health Service Utilization According to English Proficiency Among Asians in the United States. J Immigrant Minority Health 26, 91–100 (2024). https://doi.org/10.1007/s10903-023-01538-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-023-01538-6