Abstract
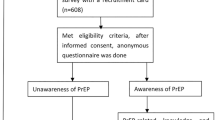
Pre-exposure prophylaxis (PrEP) is a highly effective biomedical prevention strategy that remarkably reduces HIV transmission risk. Although PrEP has been available in Nepal since 2019, very little is known about PrEP use among MSM in Nepal. This study aimed to examine PrEP awareness and its use among Nepali MSM and the factors influencing its adoption. A cross-sectional survey was conducted among MSM in Nepal between October and December 2022 (N = 250). Bivariate analysis and logistic regression were performed to determine factors associated with awareness and use of PrEP. In the study population, 59.6% of participants were aware of PrEP, however, only 30.4% of them had utilized it. The odds of PrEP awareness were higher among participants who had completed high school or above (aOR = 4.1; 95% CI = 1.8–9.6), those with health insurance coverage (aOR = 6.9; 95% CI = 2.1–22.3) and had tested for HIV (aOR = 21.2; 95% CI = 8.3–53.9). Similarly, participants who identified as gay (aOR = 3.4; 95% CI = 1.4–8.4), had visited a doctor within the past 6 months (aOR = 2.9; 95% CI = 1.2–6.5), had previously tested for HIV (aOR = 12.3; 95% CI = 3.4–44.7), and had been diagnosed with sexually transmitted infections (aOR = 7.0; 95% CI = 2.5–19.5) were more likely to have used PrEP. Our results highlight the critical importance of healthcare providers engaging in providing care for MSM, including facilitating as well as discussions about PrEP. In addition, there is a pressing need for innovative strategies (e.g., peer educators, social media, online facilitating technologies) to disseminate PrEP knowledge and reduce stigma surrounding PrEP.

Similar content being viewed by others
Data Availability
All the data used in this study can be obtained after reasonable request to corresponding author.
References
UNAIDS (2016). Prevention Gap Report.
Davies, O., Ustianowski, A., & Fox, J. (2016). Pre-exposure prophylaxis for HIV prevention: Why, what, who and how. Infect Dis Ther, 5, 407–416. https://doi.org/10.1007/s40121-016-0128-8
Chakrapani, V., Newman, P. A., Shunmugam, M., Mengle, S., Varghese, J., Nelson, R., et al. (2015). Acceptability of HIV pre-exposure prophylaxis (PrEP) and implementation challenges among men who have sex with men in India: A qualitative investigation. AIDS Patient Care STDS, 29, 569–577. https://doi.org/10.1089/apc.2015.0143
National Center for AIDS and STD Control -MoHP Nepal. (2022). National standard operating procedure for implementation of oral HIV pre-exposure prophylaxis in Nepal, 3–3.
The Global PrEP Tracker (accessed January 17, 2023). PrEPwatch.org n.d. https://data.prepwatch.org/
Zablotska, I., Grulich, A. E., Phanuphak, N., Anand, T., Janyam, S., Poonkasetwattana, M., et al. (2016). PrEP implementation in the Asia-Pacific region: Opportunities, implementation and barriers. Journal of the International Aids Society, 19, 21119. https://doi.org/10.7448/IAS.19.7.21119
Baral, S., Sifakis, F., Cleghorn, F., & Beyrer, C. (2007). Elevated risk for HIV Infection among men who have sex with men in low- and middle-income countries 2000–2006: A systematic review. Plos Medicine, 4, e339. https://doi.org/10.1371/journal.pmed.0040339
Regmi, P. R., & van Teijlingen, E. (2015). Importance of health and social care research into gender and sexual minority populations in Nepal. Asia Pacific Journal of Public Health, 27, 806–808. https://doi.org/10.1177/1010539515613413
Singh, S., Pant, S. B., Dhakal, S., Pokhrel, S., & Mullany, L. C. (2012). Human rights violations among sexual and gender minorities in Kathmandu, Nepal: A qualitative investigation. BMC Int Health Hum Rights, 12, 7. https://doi.org/10.1186/1472-698X-12-7
Wilson, E., Pant, S. B., Comfort, M., & Ekstrand, M. (2011). Stigma and HIV risk among Metis in Nepal. Culture, Health & Sexuality, 13, 253–266. https://doi.org/10.1080/13691058.2010.524247
National Centre for AIDS and STD Control- MoHP Nepal (2022). National HIV testing and treatment guidelines.
Raifman, S., DeVost, M. A., Digitale, J. C., Chen, Y. H., & Morris, M. D. (2022). Respondent-driven sampling: A sampling method for hard-to-reach populations and beyond. Curr Epidemiol Rep, 9, 38–47. https://doi.org/10.1007/s40471-022-00287-8
Nepal Rastra Bank (accessed November 27, 2023). Nepal Rastra Bank Foreign Exchange Rates n.d. https://www.nrb.org.np/forex/
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kocalevent, R. D., Berg, L., Beutel, M. E., Hinz, A., Zenger, M., Härter, M., et al. (2018). Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol, 6, 31. https://doi.org/10.1186/s40359-018-0249-9
Sherin, K. M., Sinacore, J. M., Li, X. Q., Zitter, R. E., & Shakil, A. (1998). HITS: A short domestic violence screening tool for use in a family practice setting. Family Medicine, 30, 508–512.
Torres, T. S., Luz, P. M., De Boni, R. B., de Vasconcellos, M. T. L., Hoagland, B., Garner, A., et al. (2019). Factors associated with PrEP awareness according to age and willingness to use HIV prevention technologies: The 2017 online survey among MSM in Brazil. Aids Care, 31, 1193–1202. https://doi.org/10.1080/09540121.2019.1619665
Olansky, E., Mansergh, G., Pitts, N., Mimiaga, M. J., Denson, D. J., Landers, S., et al. (2020). PrEP awareness in the context of HIV/AIDS Conspiracy beliefs among Black/African American and Hispanic/Latino MSM in three Urban US cities. Journal of Homosexuality, 67, 833–843. https://doi.org/10.1080/00918369.2018.1557953
Jones, J. T., Smith, D. K., Wiener, J., August, E. M., Finlayson, T., & Wejnert, C. (2021). Assessment of PrEP awareness, PrEP discussion with a provider, and PrEP use by transmission risk group with an emphasis on the Southern United States. Aids and Behavior, 25, 2985–2991. https://doi.org/10.1007/s10461-021-03164-5
Sullivan, P. S., Mena, L., Elopre, L., & Siegler, A. J. (2019). Implementation strategies to increase PrEP uptake in the South. Current Hiv/Aids Reports, 16, 259–269. https://doi.org/10.1007/s11904-019-00447-4
Biello, K. B., Mimiaga, M. J., Santostefano, C. M., Novak, D. S., & Mayer, K. H. (2018). MSM at highest risk for HIV acquisition express greatest interest and preference for injectable antiretroviral PrEP compared to daily, oral medication. Aids and Behavior, 22, 1158–1164. https://doi.org/10.1007/s10461-017-1972-6
Paudel, K., Gupta, S., Gautam, K., Wickersham, J. A., Khati, A., Azwa, I., et al. (2023). High interest in long-acting injectable pre-exposure prophylaxis (LAI-PrEP) for HIV prevention among men who have sex with men (MSM): Result from a nationwide survey in Malaysia. Journal of Community Health, 48, 513–521. https://doi.org/10.1007/s10900-023-01195-8
Wang, H., Zimmermann, H. M. L., van de Vijver, D., & Jonas, K. J. Intention and preference for long-acting injectable PrEP among MSM in the Netherlands: A diffusion of innovation approach. MedRxiv 2022:2022.11.11.22282218. https://doi.org/10.1101/2022.11.11.22282218
Chen, W., Ding, Y., Chen, J., Zhao, P., Wang, Z., Meng, X., et al. (2021). Awareness of and preferences for preexposure prophylaxis (PrEP) among MSM at high risk of HIV infection in Southern China: Findings from the T2T study. Biomed Research International, 2021, 1–11. https://doi.org/10.1155/2021/6682932
Frankis, J., Young, I., Flowers, P., & McDaid, L. (2016). Who will use pre-exposure prophylaxis (PrEP) and why? Understanding PrEP awareness and acceptability amongst men who have sex with men in the UK – a mixed methods study. PLoS One, 11, e0151385. https://doi.org/10.1371/journal.pone.0151385
Sun, Z., Gu, Q., Dai, Y., Zou, H., Agins, B., Chen, Q., et al. (2022). Increasing awareness of HIV pre-exposure prophylaxis (PrEP) and willingness to use HIV PrEP among men who have sex with men: A systematic review and meta‐analysis of global data. Journal of the International Aids Society, 25. https://doi.org/10.1002/jia2.25883
Bauermeister, J., Meanley, S., Pingel, E., Soler, J., & Harper, G. (2014). PrEP awareness and perceived barriers among single young men who have sex with men. Current Hiv Research, 11, 520–527. https://doi.org/10.2174/1570162X12666140129100411
Dubov, A., Galbo, P., Altice, F. L., & Fraenkel, L. (2018). Stigma and shame experiences by MSM who take PrEP for HIV prevention: A qualitative study. Am J Mens Health, 12, 1843–1854. https://doi.org/10.1177/1557988318797437
Calabrese, S. K. (2020). Understanding, contextualizing, and addressing PrEP stigma to enhance PrEP implementation. Current Hiv/Aids Reports, 17, 579–588. https://doi.org/10.1007/s11904-020-00533-y
Aghaizu, A., Mercey, D., Copas, A., Johnson, A. M., Hart, G., & Nardone, A. (2013). Who would use PrEP? Factors associated with intention to use among MSM in London: A community survey. Sexually Transmitted Infections, 89, 207–211. https://doi.org/10.1136/sextrans-2012-050648
Funding
We acknowledge financial support in part by a career development award from the National Institute on Drug Abuse (K01 DA051346) to Dr. Roman Shrestha. The funders had no role in study design, data collection, analysis, manuscript preparation, and decision to publish.
Author information
Authors and Affiliations
Contributions
RS conceptualized and conducted the research. MPK, KP and RS performed the statistical analysis. MPK and KP prepared the first draft of the manuscript by taking the subsequential help of RS, PB, and KG. All the authors critically reviewed the manuscript and provided important inputs. RS supervised the study. All the authors read, reviewed, and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Authors have no competing interest associated with this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paudel, K., Kanak, M.P., Gautam, K. et al. Awareness and Uptake of Pre-Exposure Prophylaxis (PrEP) for HIV Prevention Among Men who have Sex with Men in Nepal. J Community Health 49, 514–525 (2024). https://doi.org/10.1007/s10900-023-01318-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-023-01318-1