Abstract
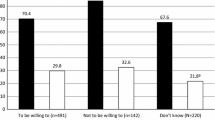
HIV pre-exposure prophylaxis (PrEP) is underutilized among Hispanics, women, and low-income individuals. To better understand PrEP barriers in this population, questionnaires were administered to 500 patients attending public health clinics in southern Arizona which provide family planning and sexually transmitted infections care. Sixty-three percent believed that they had no risk of HIV infection. When asked “Before today, did you know that there was a pill that can prevent HIV infection?” 80% of persons answered no. Among women, 88% answered no to this question. As expected, individuals with a higher perceived HIV risk (OR 1.76) or one HIV risk factor (OR 5.85) had a higher probability of knowledge. Among survey participants 87% would take a daily pill, 91% would visit a health-care provider every 3 months, and 92% would have laboratory testing every 3 months. Fifty-four percent would not be afraid or embarrassed if friends or family knew they were taking PrEP. Seventy-two percent would take PrEP despite temporary nausea. Sixty-two percent would pay ≥ $40 every 3 months for PrEP. Lack of knowledge, rather than patient attitudes, is the more important barrier to wider utilization of PrEP among individuals, especially women, attending public health clinics in Southern Arizona. Future efforts need to focus on education and access to PrEP in underserved populations including women and Hispanics.


Similar content being viewed by others
References
Centers for Disease Control and Prevention. (2018). US public health service: preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. Retrieved Dec 11, 2018 from https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv- prep-guidelines-2017.pdf.
Huang, Y. A., Zhu, W., Smith, D. K., Harris, N., & Hoover, K. W. (2018). HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. Morbidity and Mortality Weekly Report,67(14), 1147–1150.
Center for Disease Control and Prevention. HIV and Hispanics/Latinos. Retrieved Feb 2, 2019 from https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html.
Finlayson, T., Cha, S., Xia, M., et al. (2019). Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men- 20 urban areas, 2014 and 2017. Morbidity and Mortality Weekly Report,68(27), 597–603.
Centers for Disease Control and Prevention. (2019) HIV in the United States and dependent areas. Retrieved Sept 2, 2019 from https://www.cdc.gov/hiv/pdf/statistics/overview/cdc-hiv-us-ataglance.pdf.
An, Q., Prejean, J., McDavid Harrison, K., & Fang, X. (2013). Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. American Journal of Public Health,103(1), 120–126.
Centers for Disease Control and Prevention (2018) HIV surveillance report, 2017; 29. Retrieved Feb 2, 2019 from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
Arizona Department of Health Services. 2018 Arizona HIV/AIDS epidemiology supplemental report. Retrieved Feb 2, 2019 from https://www.azdhs.gov/documents/preparedness/epidemiology-disease-control/disease-integrated-services/hiv-epidemiology/reports/2018/supplemental-report.pdf.
Georgescu, A., Egurrola, C., Schaff, S., et al. (2017). PrEP uptake and emergent HIV infections in southern Arizona: Is there a disconnect? Open Forum Infectious Diseases,4(S1), S438–S439.
United States Zip Codes. (2018). United States zip codes—Tucson. Retrieved Nov 29, 2018 from https://www.unitedstateszipcodes.org/85746/.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics,42(2), 377–381.
R Core Team. (2013). R: A language and environment for statistical computing. Retrieved Dec 11, 2018 from https://www.r-project.org.
County Health Department Business Operations (eds). (2018). Pima County Health Department clinical visit summary data from eClincal Works. Fiscal year 2018. Pima County Health Department.
Walters, S. M., Rivera, A. V., Starbuck, L., et al. (2017). Differences in awareness of pre-exposure prophylaxis and post-exposure prophylaxis among groups at-risk for HIV in New York state: New York City and Long Island, NY, 2011–2013. Journal of Acquired Immune Deficiency Syndromes,75(S3), S383–S391.
Koren, D. E., Nicolas, J. S., & Simoncini, G. M. (2018). HIV pre-exposure prophylaxis and women: Survey of knowledge, attitudes and beliefs in urban obstetrics/gynecology clinic. AIDS Patient Care and STDs,32(12), 490–494.
Braksmajer, A., Fedor, T. M., Chen, S. R., et al. (2018). Willingness to take PrEP for HIV prevention: The combined effects of race/ethnicity and provider trust. AIDS Education and Prevention,30(1), 1–12.
Dolezal, C., Frasca, T., Giguere, R., et al. (2015). Awareness of post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) is low but interest is high among men engaging in condomless anal sex with men in Boston, Pittsburgh, and San Juan. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education,27(4), 289–297.
Golub, S. A., Gamarel, K. E., Rendina, H. J., Surace, A., & Lelutiu-Weinberger, C. L. (2013). From efficacy to effectiveness: Facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care and STDs,27(4), 248–254.
Kwakwa, H. A., Bessias, S., Sturgis, D., et al. (2016). Attitudes towards HIV pre-exposure prophylaxis in a United States urban clinic population. AIDS and Behavior,20(7), 1443–1450.
Garfinkel, D. B., Alexander, K. A., McDonald-Mosley, R., Willie, T. C., & Decker, M. R. (2017). Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care,29(6), 751–758.
Food and Drug Administration. (2012). FDA approves first drug for reducing the risk of sexually acquired HIV infection. Retrieved Dec 24, 2018 from https://aidsinfo.nih.gov/news/1254/fda- approves-first-drug-for-reducing-the-risk-of-sexually-acquired-hiv-infection.
US Preventive Services Task Force. Prevention of Human Immunodeficiency Virus (HIV) infection: Pre-Exposure prophylaxis. Final recommendation statement. Retrieved Sept 11, 2019 from https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis.
Hood, J. E., Buskin, S. E., Dombrowski, J. C., et al. (2016). Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS,30(3), 515–519.
Khawcharoenporn, T., Kendrick, S., & Smith, K. (2012). HIV risk perception and preexposure prophylaxis interest among a heterosexual population visiting a sexually transmitted infection clinic. AIDS Patient Care and STDs,26(4), 222–233.
Wilton, J., Senn, H., Sharma, M., & Tan, D. H. (2015). Pre-exposure prophylaxis for sexually-acquired HIV risk management: A review. HIV AIDS,7, 125–136.
Collier, K. L., Colarossi, L. G., & Sander, K. (2017). Raising awareness of pre-exposure prophylaxis (PrEP) among women in New York City: Community and provider perspectives. Journal of Health Communication,22(3), 183–189.
Vanderdrift, L. E., Agnew, C. R., Harvey, S. M., & Warren, J. T. (2013). Whose intentions predict power over condom use within heterosexual dyads. Health Psychology,32(10), 1038–1046.
Auerbach, J. D., Kinsky, S., Brown, G., & Charles, V. (2015). Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care and STDs,29(2), 102–110.
García, M., & Harris, A. L. (2017). Prep awareness and decision-making for Latino MSM in San Antonio, Texas. PLoS ONE,12(9), e0184014.
Martinez, O., Wu, E., Levine, E. C., et al. (2016). Integration of social, cultural, and biomedical strategies into an existing couple-based behavioral HIV/STI prevention intervention: Voices of Latino male couples. PLoS ONE,11(3), e0152361.
Weiss, G., Smith, D. K., Newman, S., Wiener, J., Kitlas, A., & Hoover, K. W. (2018). PrEP implementation by local health departments in US cities and counties: Findings from a 2015 assessment of local health departments. PLoS ONE,13(7), e0200338.
Hanchette, C. L., Gibbs, D. A., Gilliam, A., Fogarty, K. J., & Bruhn, M. (2005). A national, geographic database of CDC-funded HIV prevention services: Development challenges and potential applications. International Journal of Health Geographics,4, 28.
Zhang, H. L., Rhea, S. K., Hurt, C. B., et al. (2018). HIV preexposure prophylaxis implementation at local health departments: A statewide assessment of activities and barriers. Journal of Acquired Immune Deficiency Syndromes,77(1), 72–77.
Acknowledgements
This research was funded by the University of Arizona Division of Infectious Diseases. In addition, we acknowledge Francisco Garcia, MD; the staff at the Pima County Health Department North and Theresa Lee Clinics; Anca Georgescu,MD, Amanda Marie Kendall, Kelechi Catherine Abarikwu, Molly Brady, Lakshmeeramya Mallardi, Ashwini Kaveti, Berna Villanuena, and Adrienne Kishi for assisting with surveys; Elizabeth Connick, MD for editing; and Martha Barron for study administration and survey translation.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the project and development of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shende, T.C., Fisher, J.M., Perez-Velez, C.M. et al. PrEP Knowledge and Attitudes Among Adults Attending Public Health Clinics in Southern Arizona. J Community Health 45, 400–406 (2020). https://doi.org/10.1007/s10900-019-00758-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-019-00758-y